Last Updated on November 25, 2025 by Ugurkan Demir

Many think that good cholesterol levels keep arteries clear. But, new findings show that genetics, blood pressure, and how cells work can cause blockages. This can happen even when someone has low or normal cholesterol.Learn if can you have blocked arteries with low cholesterol and why it occurs.
At Liv Hospital, we put patients first. We use the latest research to help everyone. It’s key to understand how cholesterol, genetics, and other risk factors work together.
Cholesterol is vital for our bodies, but too much in the blood raises heart disease risk. Our diet adds about 20% of our cholesterol. We look into how genetic factors, blood pressure issues, and cell stress lead to blocked arteries.
Cholesterol levels and arterial health are closely linked. It’s not just about the numbers. How our body processes cholesterol matters a lot. Keeping our arteries healthy is key to a strong heart.
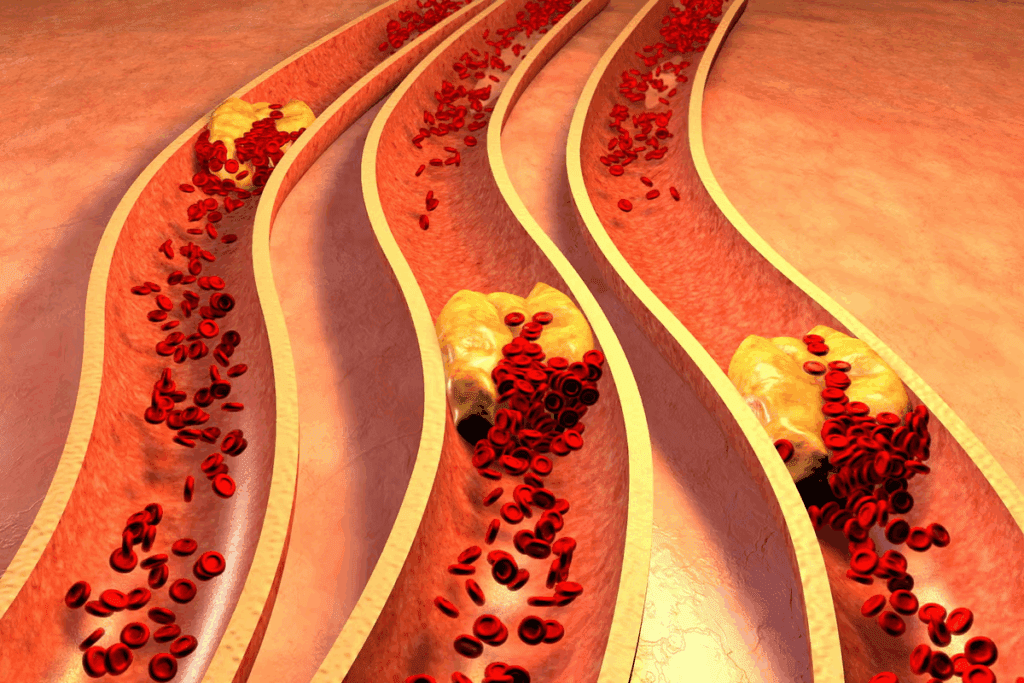
Atherosclerosis means our arteries get hard and narrow. It starts early and grows over time. Plaque, made of fat, cholesterol, and more, builds up inside the arteries.
This buildup can block blood flow. It might cause heart attacks or strokes. Many things can lead to atherosclerosis, like genes and lifestyle.
High cholesterol was once seen as a big risk for plaque and atherosclerosis. High LDL cholesterol, or “bad” cholesterol, was thought to cause plaque. On the other hand, HDL or “good” cholesterol was believed to help clear cholesterol from the blood.
Key factors traditionally linked to plaque formation include:
New research is changing how we see cholesterol and atherosclerosis. Some people with normal or low cholesterol can have a lot of plaque. Others with high cholesterol might not. This shows there’s more to heart health than just cholesterol.
Our approach to heart health is changing too. We’re looking at more than just cholesterol. We’re considering inflammation, genetics, and other health issues.
Recent studies have found a surprising link between normal cholesterol levels and blocked arteries. This challenges the old idea that low cholesterol means healthy arteries.
Research shows a big paradox: up to 50% of people with ideal cholesterol levels have a lot of plaque in their arteries. This is known as the “50 Percent Paradox.” It shows that artery health is more complex than just cholesterol.
We’re learning that cholesterol isn’t the only factor in artery blockage. Other factors are also important.
Many case studies show heart attack victims had normal or low cholesterol. These cases help us understand that heart disease risk isn’t just about cholesterol.
A study found that many heart attack victims had normal cholesterol. This shows we need to look at more than just cholesterol to understand heart disease risk.
Cholesterol tests alone aren’t enough to check heart health anymore. They don’t show other important factors like inflammation, genetics, and lifestyle.
We need a more complete way to check artery health. This should include more risk factors and tests. This way, we can spot risks better and help prevent heart problems.
Genetics play a big role in blocked arteries, even with good cholesterol. This is key to understanding how genes and heart health are connected.
Studies have found certain genetic mutations linked to atherosclerosis. The SVEP1 and ACTA2 genes are key. SVEP1 helps cells stick together, and ACTA2 controls blood vessel muscle contraction. Mutations in these genes can cause plaque buildup.
Key aspects of SVEP1 and ACTA2 mutations include:
Family history is a big factor in atherosclerosis. People with heart disease in their family are at higher risk. This suggests a genetic link to the disease.
Even with good cholesterol, some people can get blocked arteries due to genetics. This shows why genetics are important in heart disease risk. Genetic tests can spot risks early, leading to better treatment plans.
The connection between genetics and heart health is complex. Knowing this helps doctors give better care to those at risk.
The body makes its own cholesterol, which affects artery health. Blood tests show cholesterol levels but don’t show what’s happening in arteries.
The liver makes most of the body’s cholesterol. This internal cholesterol production is key for many body functions. But, too much cholesterol from the liver can increase the risk of artery blockages, even with normal blood cholesterol.
Cellular cholesterol metabolism is how cells handle cholesterol. It involves taking in, storing, and removing cholesterol. If this process goes wrong, cholesterol can build up in arteries, causing blockages.
Blood tests show cholesterol levels but not artery health. The cholesterol in blood doesn’t always match the cholesterol in arteries. So, blood tests alone can’t fully show heart health.
It’s important to understand the difference between internal cholesterol production and blood levels. This helps doctors better prevent and treat heart disease.
The link between cholesterol and artery health is not simple. We must look closely at how cholesterol affects arteries. This includes understanding how plaque forms and the role cholesterol plays in it.
Plaque forms when cholesterol, inflammatory cells, and other materials build up in artery walls. This starts when the artery’s lining gets damaged. Then, lipids and inflammatory cells can get in and build up.
This buildup creates atherosclerotic plaques. These plaques can block blood flow. These plaques are made of cholesterol, other lipids, smooth muscle cells, and inflammatory components.
Cholesterol is a key part of arterial plaque. It grows and makes plaques unstable. Cholesterol’s role in plaques is not just passive. It’s an active process involving cells.
LDL cholesterol is important in making atherosclerotic plaques. LDL cholesterol gets trapped in the artery wall. It gets oxidized and taken up by macrophages, leading to foam cell formation and more plaque.
The idea that cholesterol “clogs” arteries is too simple. Atherosclerosis is a complex disease involving inflammation and cell growth. Understanding this complexity is key to finding effective treatments.
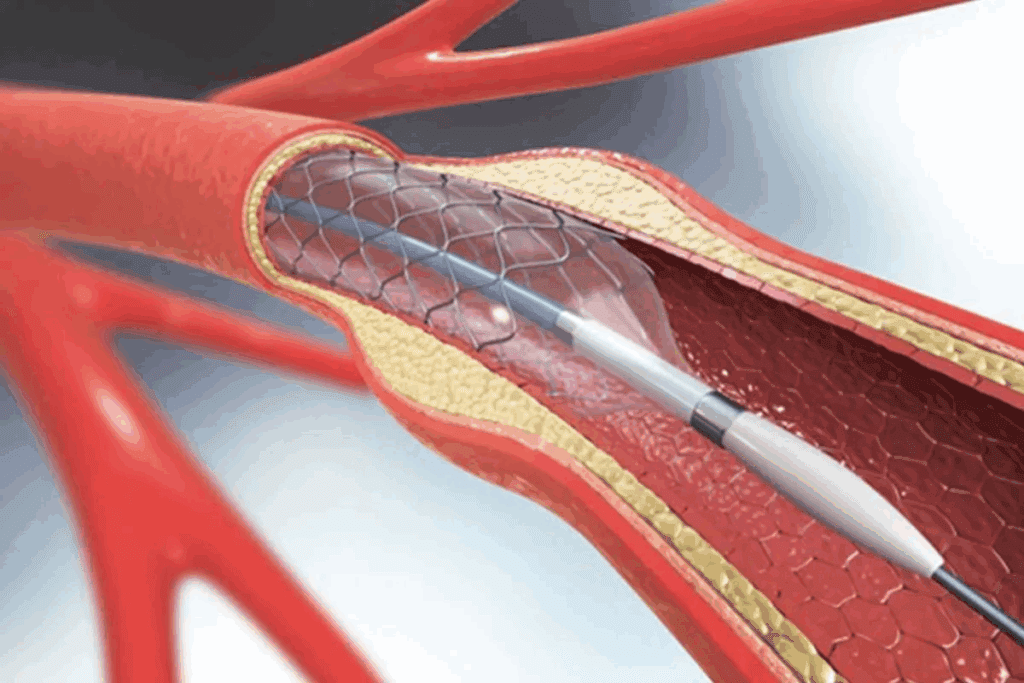
The “clogging” idea makes it seem like a one-way process. But atherosclerosis is dynamic and involves many factors. This shows we need a full approach to heart health, including lifestyle changes and specific treatments.
High blood pressure is a big risk for heart disease, even with normal cholesterol. We must grasp how high blood pressure harms arteries and increases the chance of blocked arteries.
Hypertension harms arterial walls by applying too much pressure on the endothelial lining. This causes inflammation and damage. The walls then become more likely to form plaque.
The Mechanism of Damage: The constant high pressure can cause tiny tears in the walls. This starts a process that leads to inflammation and repair. Over time, the walls thicken and lose their flexibility.
Blood pressure is a major risk for heart disease on its own. High blood pressure can cause heart attacks and strokes, even without high cholesterol.
The INTERHEART study and other research confirm hypertension’s role in heart attacks and strokes. This shows its importance in heart health.
| Risk Factor | Relative Risk | Confidence Interval |
| Hypertension | 2.5 | 2.0-3.1 |
| High Cholesterol | 2.1 | 1.8-2.5 |
| Smoking | 2.9 | 2.4-3.5 |
Having multiple risk factors, like hypertension, high cholesterol, and smoking, greatly increases heart disease risk. It’s not enough to just manage one risk. A full approach is needed.
Risk Stratification: Knowing how risk factors add up helps sort patients into risk groups. This guides treatment and prevention plans.
A patient with both hypertension and high cholesterol is at higher risk than someone with just one. So, a treatment plan that tackles all risks is key.
People with normal blood pressure but high cholesterol face a special challenge. We must remember that normal blood pressure doesn’t mean no risk from high cholesterol.
Cholesterol can build up even with healthy blood pressure. This is due to genetics and lifestyle. High cholesterol can cause plaque in arteries, raising heart disease risk.
Understanding cholesterol buildup is key. It involves how much the liver makes, what we eat, and how well our body removes excess cholesterol.
Finding hidden heart risks in those with normal blood pressure but high cholesterol needs a detailed look. We examine family history, lifestyle, and other health issues.
A thorough check might include:
Regular checks are vital for those with normal blood pressure but high cholesterol. We suggest:
| Monitoring Parameter | Frequency |
| Lipid Profile | Every 6-12 months |
| Blood Pressure | Every 3-6 months |
| Cardiovascular Risk Assessment | Annually |
By keeping a close eye on these, we can spot problems early. This helps us take steps to lower heart disease risk.
The start of clogged arteries often happens in early adulthood. It’s influenced by many factors. Atherosclerosis, or the clogging of arteries, can start years before symptoms show up.
Studies show that atherosclerosis signs can appear in young adults, even teens. Fatty streaks, early signs of plaque, have been found in young people’s arteries.
These early signs are linked to lifestyle, genetics, and health conditions. For example, eating too much saturated fat and cholesterol can lead to fatty streaks.
How fast atherosclerosis progresses varies a lot. It depends on genetics, lifestyle, and environment.
| Risk Factor | Impact on Progression |
| Smoking | Significantly accelerates plaque buildup |
| High Blood Pressure | Damages arterial walls, facilitating plaque formation |
| High Cholesterol | Contributes directly to plaque buildup |
Knowing these risk factors helps find who’s at higher risk. It’s key for starting prevention early.
Stopping or slowing atherosclerosis needs a plan for each age group.
By using these strategies, people can lower their risk of clogged arteries, no matter their age.
Inflammation and cellular stress play big roles in atherosclerosis. They help form arterial plaque. Knowing how they work is key to finding new treatments, not just lowering cholesterol.
Oxidative stress happens when our body can’t handle reactive oxygen species (ROS). This imbalance can make LDL cholesterol oxidize. Oxidized LDL then helps form plaque in arteries.
Oxidized LDL is important in atherosclerosis. It helps create foam cells. These cells, full of lipids, build up in the artery wall, adding to the plaque.
| Factor | Effect on Plaque Formation | Role in Atherosclerosis |
| Oxidative Stress | Increases | Promotes plaque instability |
| Inflammation | Enhances | Contributes to plaque growth |
| Antioxidants | Decreases | May stabilize plaques |
Inflammation is key in atherosclerosis. When an artery gets hurt, it starts an inflammatory response. This brings immune cells and pro-inflammatory cytokines.
“Inflammation is now recognized as a key driver of atherosclerosis, and its modulation represents a promising therapeutic target.”
Source: Expert Review on Cardiovascular Therapy
This inflammation makes plaques grow and become unstable. This can lead to heart attacks or strokes.
There’s a lot of interest in treatments that fight inflammation in atherosclerosis. New drugs and biologics aim to reduce inflammation in the heart.
Some treatments include:
These new treatments show a shift in heart disease treatment. They focus on more than just lowering cholesterol, tackling the complex issues of atherosclerosis.
Cholesterol isn’t the only thing that affects coronary artery disease (CAD). Other factors are just as important. Knowing about these can help us prevent and manage CAD better.
Our lifestyle choices greatly impact CAD risk. Smoking harms blood vessels, making them more likely to block. Physical inactivity leads to obesity and high blood pressure, raising CAD risk.
What we eat also matters. A diet full of saturated fats, trans fats, and sodium increases CAD risk. But eating more fruits, vegetables, and whole grains can help lower it.
Stress and poor sleep quality also raise CAD risk. Stress can cause inflammation and high blood pressure. Bad sleep can disrupt heart health.
Metabolic conditions like diabetes and insulin resistance increase CAD risk. They damage blood vessels and nerves that control the heart. Obesity, too, is a big risk factor, linked to high blood pressure and cholesterol.
Metabolic syndrome is a group of conditions that raise CAD risk. It includes high blood pressure, high blood sugar, and excess body fat. Managing these conditions is key to lowering CAD risk.
Environmental factors also affect CAD risk. Air pollution exposure can increase cardiovascular disease risk. Exposure to certain chemicals can also raise CAD risk.
Socioeconomic factors play a role too. People from lower socioeconomic backgrounds often face barriers to healthcare and healthy living. This can increase CAD risk.
Understanding CAD’s many risk factors is key to prevention and management. By tackling lifestyle, metabolic, and environmental factors, we can reduce CAD incidence and improve heart health.
Arterial health is more than just about cholesterol levels. It’s influenced by many factors, like genetics, how our body makes cholesterol, and lifestyle choices. Even with normal or low cholesterol, conditions like atherosclerosis can occur.
Managing our arteries well means looking at all risk factors and prevention strategies. Knowing how plaque forms, the role of inflammation, and the effects of our lifestyle helps us tackle heart disease and cholesterol better.
Looking at arterial health in a new way means considering genetics, environment, and body functions. This approach helps people make better choices for their heart health. It goes beyond just looking at cholesterol numbers.
Using this knowledge in our daily lives helps us reduce heart disease and cholesterol risks. It leads to a healthier heart by combining smart lifestyle choices and medical care.
Yes, blocked arteries can happen even with normal cholesterol. This is due to genetics, high blood pressure, and cellular stress.
High blood pressure damages the walls of arteries. It’s a risk factor for heart disease on its own. It also makes other risks worse, leading to blocked arteries.
Yes, you can have clogged arteries even with normal blood pressure. Genetics, lifestyle, and metabolic conditions play a role.
Cholesterol is part of plaque formation. But, inflammation, cellular stress, and genetics also play a big part.
Yes, high cholesterol can lead to heart disease, even with normal blood pressure. It helps form plaque in arteries.
Atherosclerosis can start early, even in young adults. It’s influenced by genetics, lifestyle, and metabolic conditions.
High cholesterol and normal blood pressure are risky for heart disease. It’s important to watch for hidden risks and monitor closely.
Genetics, including certain mutations, can lead to plaque formation. They affect artery health, regardless of cholesterol levels.
The liver’s cholesterol production and cell metabolism affect artery health. Blood cholesterol levels don’t always show artery condition.
No, cholesterol tests alone can’t measure cardiovascular risk. They don’t consider lifestyle, metabolic conditions, or environmental factors.
The “clogging” metaphor simplifies plaque formation. It doesn’t show the many factors that cause blockage.
New treatments aim to reduce inflammation in atherosclerosis. They target oxidative stress and inflammation to slow plaque growth.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!