Last Updated on November 27, 2025 by Bilal Hasdemir
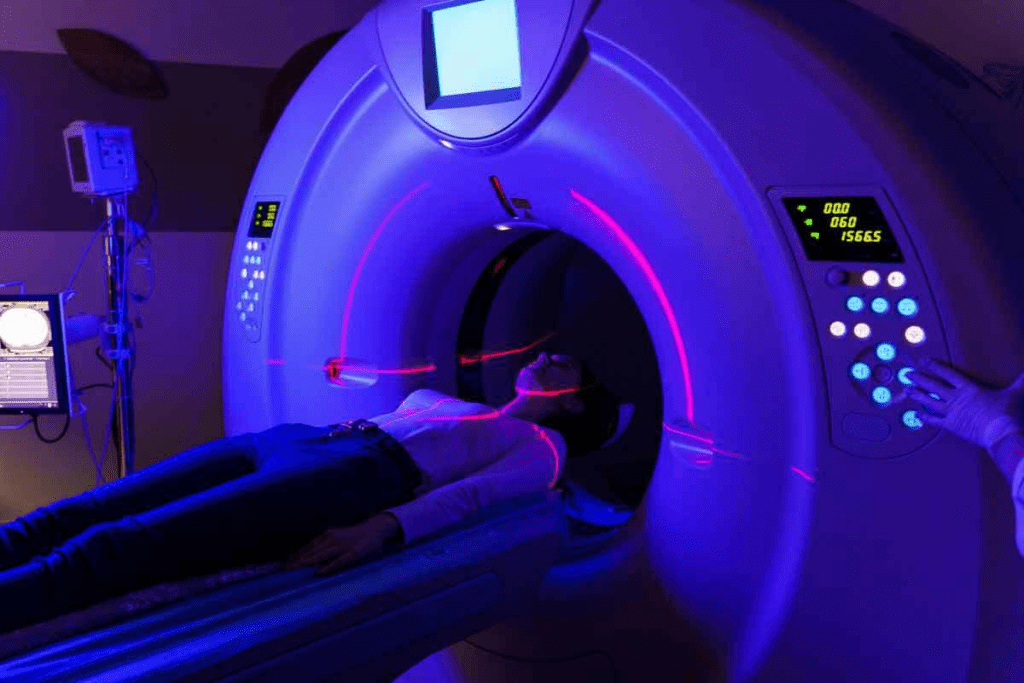
Radiation therapy is a key treatment for many cancers. It uses high-energy particles or waves to kill or harm cancer cells. At Liv Hospital, we follow international standards and focus on our patients to give them the best care. Many people often ask, “can you have radiation therapy more than once? The answer depends on the type of cancer, the area treated, and the patient’s overall health. Our specialists carefully evaluate each case to ensure safe and effective treatment.
This treatment aims to stop cancer cells from growing by damaging their DNA. But, there’s a limit to how much radiation an area can safely get over a lifetime. The National Cancer Institute says going over this limit can cause serious side effects.
It’s important for patients and doctors to know these limits. We’ll look into radiation therapy and its uses. We’ll also talk about what decides the safe dose for cancer patients.
Key Takeaways
- The amount of radiation an area can safely receive is limited.
- Previous radiation exposure affects the feasibility of subsequent treatments.
- The distance between treated areas can impact the possibility of additional radiation therapy.
- Radiation therapy targets cancer cells by damaging their DNA.
- The maximum safe radiation dose is a critical consideration in cancer treatment.
Understanding Radiation Therapy Basics

Learning about radiation therapy is key for those facing cancer. It’s a major treatment that fights cancer. We’ll look at how it works, its types, and its role in cancer treatment.
What Is Radiation Therapy and How Does It Work?
Radiation therapy damages cancer cells’ DNA, killing them or slowing their growth. It uses high-energy particles or waves to target cancer cells. The aim is to hit the tumor with precision, protecting healthy tissues.
Mechanism of Action: Ionizing radiation breaks DNA strands in cancer cells, stopping them from reproducing. This leads to cell death.
Common Types of Radiation Treatment
There are many types of radiation therapy, each with its own use and benefits.
- External Beam Radiation Therapy (EBRT): This is the most common, where radiation comes from outside the body.
- Internal Radiation Therapy (Brachytherapy): This involves placing radioactive material inside or near the tumor.
- Systemic Radiation Therapy: Uses radioactive substances that travel through the body to find and destroy cancer cells.
| Type of Radiation Therapy | Description | Application |
| External Beam Radiation Therapy (EBRT) | Radiation delivered from outside the body | Most common type, used for various cancers |
| Internal Radiation Therapy (Brachytherapy) | Radioactive material placed inside or near the tumor | Used for localized tumors, such as prostate cancer |
| Systemic Radiation Therapy | Radioactive substances travel through the body | Used for cancers that have spread, such as thyroid cancer |
The Goal of Radiation in Cancer Treatment
The main goals of radiation therapy are to cure cancer, prevent it from coming back, or ease symptoms. The goal depends on the cancer type, stage, and the patient’s health.
Curing Cancer: In some cases, radiation can cure cancer by removing the tumor completely.
Preventing Recurrence: Radiation can be used after surgery to kill any remaining cancer cells, lowering the risk of it coming back.
Palliative Care: For advanced cancers, radiation can help ease symptoms, improving the patient’s quality of life.
Can You Have Radiation Therapy More Than Once?
Many patients wonder if they can have radiation therapy more than once. The answer is not simple. It depends on several important factors.
The Short Answer: Yes, But With Limitations
Yes, you can have radiation therapy again, but there are big limits. The main worry is how much radiation you can safely get. We must weigh the risk of harming healthy tissues against the benefits of treating cancer.
Repeating radiation therapy is decided for each patient separately. We look at the first treatment and the patient’s current health. Our aim is to get the most benefit while keeping risks low.
Factors That Determine Eligibility for Repeat Treatment
Several important factors decide if you can have radiation therapy again. These include:
- The total dose of radiation you’ve had before
- The area of your body treated first
- How long it’s been after the first treatment
- Your overall health and how you responded to previous treatments
We also think about the type of cancer and if it has come back or spread. Each of these factors is key in deciding if more radiation is safe and possible.
Timeframes Between Initial and Subsequent Treatments
The time between the first and any follow-up radiation therapy is very important. Usually, the longer the wait, the better it is for repeat treatment. This is because healthy tissues can recover, making more radiation safer.
But, we’re careful when deciding on repeat radiation. We balance the possible benefits against the risks of side effects and harm to healthy tissues. New radiation technologies help us safely give treatments again.
We look at each patient’s situation carefully. We consider all the factors to make the best decision about repeat radiation therapy. Our goal is to give our patients the best care possible.
The Science Behind Radiation Dose Limits
The science of radiation dose limits is complex. It involves looking at how radiation affects healthy tissues. Radiation therapy can kill cancer cells but also harms healthy tissues, leading to side effects.
The goal is to find a balance. We want to use radiation to fight cancer without harming too much of the body.
How Radiation Affects Healthy Tissues
Radiation therapy damages cancer cells by messing with their DNA. But, it also affects nearby healthy tissues. This can cause side effects.
The damage to healthy tissues depends on several things. These include the dose of radiation, how much tissue is exposed, and the type of radiation.
Acute side effects happen during or right after treatment. These can include fatigue, skin reactions, and stomach problems. Late effects can show up months or years later. They might include fibrosis, secondary cancers, and problems with organs.
Cumulative Radiation Exposure Concerns
The more radiation you get, the higher the risk of side effects. This is a big worry for people who need to have radiation therapy more than once.
When planning radiation treatment, we must think about the total dose. New techniques like IMRT and proton therapy help protect healthy tissues. This reduces the risk of damage from repeated radiation.
Maximum Tolerable Dose Calculations
Finding the maximum tolerable dose (MTD) is a detailed process. It looks at how different tissues and organs can handle radiation. The MTD depends on several factors, like the dose per fraction and the total dose.
| Organ/Tissue | Max Tolerable Dose (Gy) | Complication |
| Spinal Cord | 45-50 | Myelopathy |
| Lung | 20-30 | Pneumonitis |
| Liver | 30-35 | Hepatitis |
Knowing these limits is key to safe and effective radiation therapy. By planning and delivering treatment carefully, we can help patients. We aim to get the most benefit from radiation while protecting healthy tissues.
Tissue Tolerance: Why Some Areas Can’t Be Re-Treated
Radiation therapy is good against cancer but has limits. The body’s tissue tolerance is a big factor. We must think about these limits to treat safely and effectively.
High-Risk Organs and Structures
Some organs and structures can’t handle radiation well. These include:
- The spinal cord, which can suffer from radiation myelopathy if exposed to high doses
- The brainstem, where radiation damage can lead to serious neurological complications
- The eyes, specially the lens, which can develop cataracts after radiation exposure
- The gastrointestinal tract, where radiation can cause ulcers, strictures, or fistulas
These organs are “serial organs.” Damage to a small part can harm the whole organ. We must be careful when treating areas near these critical structures.
Long-Term Damage Considerations
The long-term effects of radiation therapy are very important. Late effects can include:
- Fibrosis: scarring that can lead to organ dysfunction
- Atrophy: shrinkage of tissues or organs
- Secondary cancers: new malignancies induced by radiation exposure
We weigh these risks against the benefits of radiation therapy. This helps us choose the best treatment plan.
How Previous Treatment Fields Affect Future Options
Previous radiation treatment can limit future options. The body can only handle so much radiation. We look at several factors when deciding if re-treatment is possible:
- The dose and volume of previous radiation treatment
- The time elapsed after the initial treatment
- The specific techniques used in the previous radiation therapy
By evaluating these factors, we find the safest and most effective treatment for each patient.
Re-Irradiation: When Second Courses Are Possible
Thanks to new technology, getting a second round of radiation therapy is now an option for some patients. This is great for those with cancer that comes back in a spot already treated.
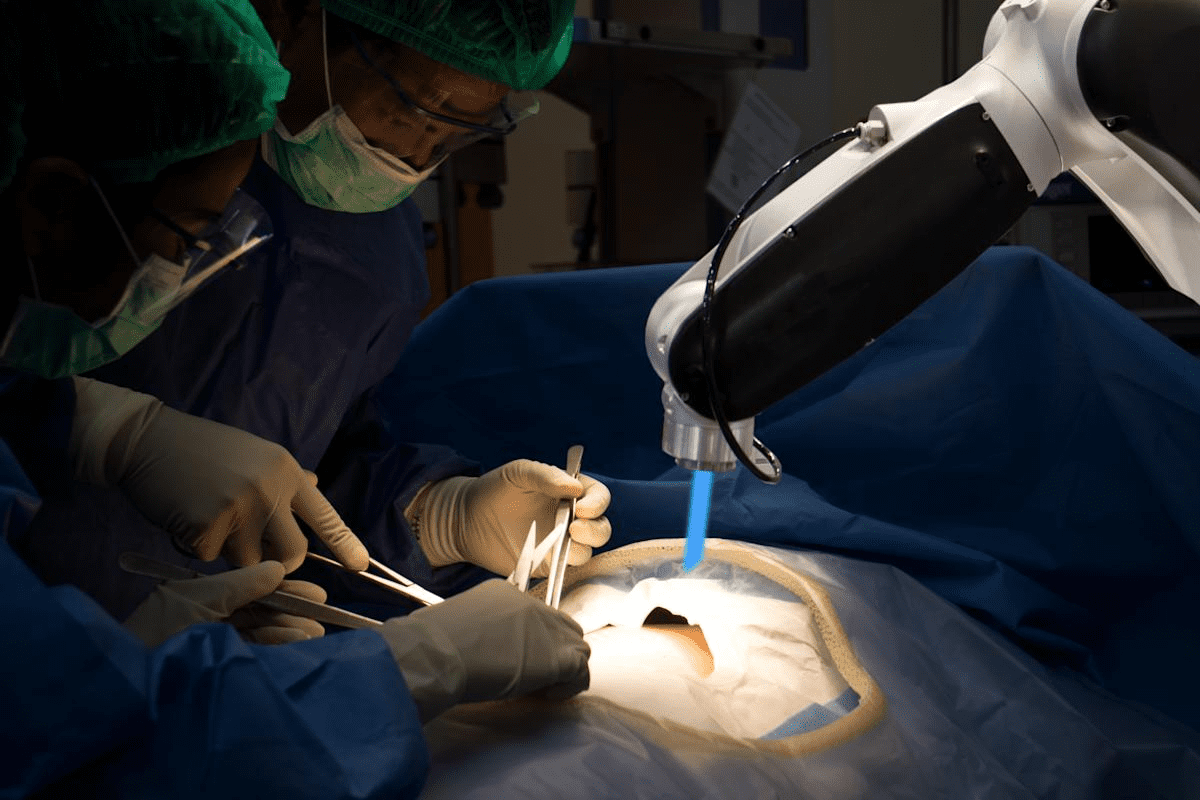
Advanced Precision Techniques Making Re-Treatment Safer
New ways to target tumors with radiation have made second treatments safer and more effective. Stereotactic Body Radiation Therapy (SBRT) and Intensity-Modulated Radiation Therapy (IMRT) are examples. They help avoid harming healthy tissues nearby.
A study found these methods work well for cancer that has spread. This is good news for patients facing tough cancer challenges.
Cancer Types Most Amenable to Re-Irradiation
Not every cancer can be treated with a second round of radiation. But, some cancers like head and neck cancers, breast cancer, and prostate cancer might be good candidates. Whether or not to try re-irradiation depends on several things.
These include how much radiation was used first, where the cancer came back, and the patient’s health. A doctor will look at all these factors to decide.
| Cancer Type | Re-Irradiation Suitability | Key Considerations |
| Head and Neck Cancer | High | Proximity to critical structures, previous radiation dose |
| Breast Cancer | Moderate to High | Tumor location, previous treatment fields |
| Prostate Cancer | Moderate | Initial radiation dose, recurrence location |
The Importance of Time Between Treatments
The time between the first and second radiation treatments is very important. A longer gap can help normal tissues recover. This might lower the chance of side effects.
But, how long is best varies from person to person. A radiation oncologist will figure out the best timing for you.
Thinking about getting radiation therapy again can be scary. But, with today’s technology and careful planning, it’s becoming a real option for many. Always talk to a doctor to understand what’s best for you.
Typical Radiation Treatment Protocols
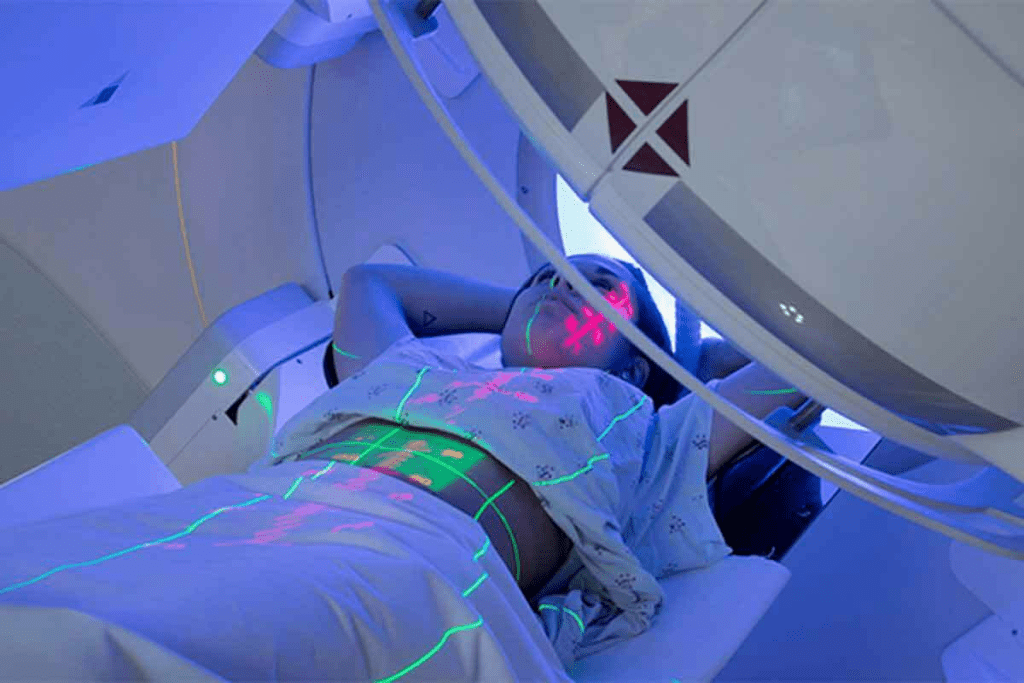
The length and frequency of radiation therapy depend on several things. These include where the cancer is and what the treatment aims to do. Every patient’s treatment is unique, as radiation therapy is highly personalized.
There are two main types of radiation treatment protocols. These are single-session and multiple-week regimens. The choice depends on the cancer type, the patient’s health, and the treatment goals.
Single-Session vs. Multiple-Week Regimens
Single-session radiation therapy, or SBRT, gives a high dose in one go. It’s used for small, hard-to-reach tumors. This method is quick and simple for patients.
On the other hand, multiple-week regimens split the dose into smaller parts. This makes it easier to handle and helps avoid side effects. It also allows for higher doses overall.
- Advantages of Single-Session Therapy:It’s convenient, needing only one visit
- It can be faster overall
- Advantages of Multiple-Week Regimens:It’s easier on the body
- It lets you give more total dose
Fractionation: Breaking Up Doses for Safety
Fractionation is key in radiation therapy. It helps deliver effective doses safely. By splitting the dose, we protect healthy tissues better.
How Treatment Intent Affects Duration
The goal of radiation therapy changes how long it lasts. Treatments meant to cure cancer need more time. They aim to kill all cancer cells.
But treatments meant to ease symptoms are shorter. They use lower doses to improve life quality, not to cure.
- Curative treatments: Longer courses, higher total doses
- Palliative treatments: Shorter courses, lower total doses
Knowing these details helps doctors create the best treatment plans. They balance treatment success with safety and quality of life.
Combining Radiation With Other Cancer Treatments
Cancer treatment often mixes radiation therapy with chemotherapy or other methods. This mix can be very effective against many cancers. We’ll look at how radiation therapy works with other treatments and what it means for patient care.
Concurrent Chemotherapy and Radiation
Concurrent chemotherapy and radiation mean using both treatments at the same time. This makes cancer cells more likely to be killed by radiation. Research shows it can help in treating cancers like head and neck, cervical, and lung cancers.
The benefits of using both treatments together include:
- Enhanced tumor response to treatment
- Potential for improved survival rates
- Reduced risk of cancer recurrence
The “Chemo and Radiation 5 Days a Week” Approach
The “chemo and radiation 5 days a week” method means giving both treatments on the same day, five days a week. It’s used for aggressive or advanced cancers. The goal is to get the best results in less time.
This method needs careful planning and watching because of the higher risk of side effects. Patients need close monitoring to manage side effects and keep their health good.
How Combined Treatments Affect Total Radiation Limits
When radiation therapy is used with other treatments, like chemotherapy, it can change how much radiation a patient can get. It’s important to watch the total radiation exposure to avoid harming healthy tissues too much.
The table below shows how combining treatments can change total radiation limits:
| Treatment Modality | Effect on Radiation Limits | Clinical Considerations |
| Chemotherapy + Radiation | May require adjustment of radiation dose | Close monitoring for toxicity |
| Radiation Alone | Standard radiation limits apply | Less risk of cumulative toxicity |
| Surgery + Radiation | May alter radiation distribution | Consideration of tissue healing post-surgery |
Understanding how combined treatments affect radiation limits helps doctors create safer and more effective plans for cancer patients.
Safety Measures and Monitoring During Radiation Therapy
To make radiation therapy safe and effective, we use many safety steps. We focus on advanced technology and careful monitoring. This helps reduce risks from radiation.
Cumulative Exposure Tracking
Radiation oncologists track how much radiation patients get. They keep records of past treatments. This helps decide if more treatment is safe.
Studies show tracking doses is key in radiation therapy. This is important, as seen in research on PMC.
Technological Advancements in Radiation Therapy
New technology has made radiation therapy safer. Modern tools help target tumors better, protecting healthy tissues. Techniques like IMRT and SBRT improve treatment precision.
These advances let us give higher doses to tumors safely. This reduces harm to important areas.
Patient Monitoring Throughout Treatment
Watching patients closely is key in radiation therapy. We check for side effects and changes during treatment. This helps us adjust plans for better results.
Regular checks also catch problems early. This allows us to act fast and prevent bigger issues.
By planning carefully, using new tech, and watching patients closely, we keep radiation therapy safe. Our goal is always to protect our patients and improve treatment results.
Special Considerations for Different Cancer Types
Different cancers need different treatments. Radiation therapy is no exception. Each cancer type has its own needs, so a single treatment plan doesn’t work for all.
Breast Cancer Radiation Protocols
Breast cancer often gets treated with radiation. This is true after surgeries like lumpectomy or mastectomy. The goal is to kill any cancer cells left behind.
We use methods like whole-breast irradiation (WBI) and accelerated partial breast irradiation (APBI). These tailor treatments to fit each patient’s situation.
Key considerations for breast cancer radiation include:
- Tumor size and location
- Cancer stage
- Patient’s overall health
- Previous treatments
Brain Tumor Re-Irradiation Challenges
Re-treating brain tumors is tricky. It’s because the brain is very sensitive. We must think carefully about the benefits and risks of re-treatment.
Techniques like stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy (FSRT) help protect healthy brain tissue.
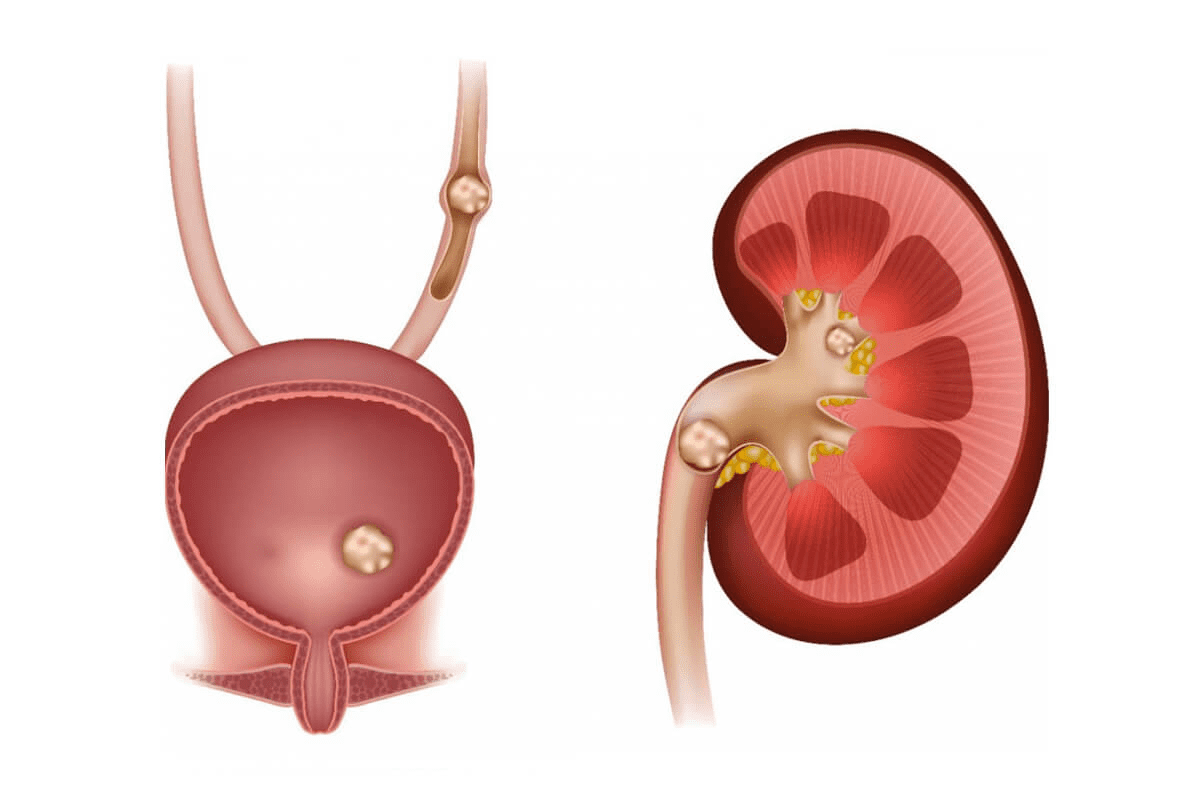
Prostate Cancer Radiation Options
Prostate cancer can be treated with radiation in several ways. We look at the cancer’s stage, Gleason score, and the patient’s health to decide the best treatment.
| Radiation Technique | Description | Benefits |
| EBRT | External beam radiation therapy | Non-invasive, precise targeting |
| Brachytherapy | Internal radiation therapy | High dose delivery directly to tumor |
Head and Neck Cancer Considerations
Head and neck cancer radiation needs careful planning. We aim to avoid harming nearby important areas like the eyes and salivary glands. Techniques like intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) help us target the tumor accurately.
The complexity of head and neck anatomy demands a highly personalized approach to radiation therapy. Advanced radiation techniques help improve outcomes and reduce side effects.
Making Informed Decisions About Repeat Radiation
Understanding the benefits and risks of repeat radiation therapy is key. As a patient, being involved in your care is vital. It’s important to talk openly with your radiation oncologist.
Questions to Ask Your Radiation Oncologist
To make informed choices, ask the right questions. Discuss the benefits and risks of repeat radiation therapy with your oncologist. Also, ask about the success rate and other treatment options. Here are some questions to consider:
- What are the possible side effects of repeat radiation therapy?
- How might repeat radiation therapy affect my quality of life?
- Are there other treatments I should look into?
- What are the chances of success with repeat radiation therapy?
Weighing Benefits Against Risks
It’s important to balance the benefits against the risks of repeat radiation therapy. Understand the side effects, how it might affect your life, and the success rate. Your oncologist can guide you based on your situation.
Key factors to think about include the radiation dose, how often it’s given, and where it’s applied. Also, consider your overall health. By looking at these, you can decide if repeat radiation therapy is right for you.
Second Opinion Considerations
Getting a second opinion is a smart move. It can give you more insights and confidence in your treatment. When looking for a second opinion, find a radiation oncologist experienced in your cancer type.
By being proactive and seeking the right information, you can make choices about repeat radiation therapy that fit your needs.
Conclusion
Radiation therapy is a complex treatment for cancer. Its success depends on many factors. These include the cancer type, its location, and the patient’s health.
This article has covered the details of radiation therapy. We looked at its limits and when it can be repeated.
It’s important to know that radiation therapy can be repeated. But, there are limits to how many times it can be used in one area. These limits are based on how much radiation the body can handle.
Knowing these limits helps make radiation therapy safer and more effective. It ensures the treatment’s benefits are maximized while risks are minimized.
Our summary shows how important safety in radiation therapy is. Advanced techniques, careful planning, and monitoring patients are key. These steps help improve treatment results and lower risks.
As we keep improving in radiation oncology, we can give better care. This care is tailored to each patient’s needs. It improves their life quality and treatment results.
In summary, radiation therapy is a key part of cancer treatment. It offers hope and healing to many. By understanding its limits and safety, we can use it to better help patients.
FAQ
Can you have radiation therapy more than once?
Yes, but there are limits and things to consider. These include the dose of radiation you’ve had before and how long it’s been.
Why can’t you have radiation therapy twice in the same area?
Some places can’t be treated again because of tissue tolerance. There’s also a risk of harming healthy tissues, which is a big concern.
What is the maximum number of radiation treatments you can have?
It varies a lot. It depends on the cancer type, the treatment goal, and your personal health.
How often can you have radiotherapy?
Radiotherapy frequency varies. It can be one session or many weeks. It depends on the treatment plan and your health.
Can you do chemo and radiation at the same time?
Yes, some cancers are treated with both chemotherapy and radiation at once. But, it’s important to weigh the risks and benefits.
What are the concerns with cumulative radiation exposure?
Getting more radiation can harm healthy tissues. This is a big worry when thinking about getting radiation again.
How do radiation oncologists track cumulative exposure?
They use advanced tech and careful planning. This helps them keep track of radiation exposure and reduce risks.
Are there special considerations for different types of cancer?
Yes, each cancer type has its own radiation treatment plan. This includes breast, brain, prostate, and head and neck cancers.
What questions should you ask your radiation oncologist about repeat radiation therapy?
Ask about the benefits and risks, how likely it is to work, and other treatment options.
How do you weigh the benefits against the possible risks of repeat radiation therapy?
Think about your situation and talk to your doctor. Getting a second opinion can also help.
Can you have radiation treatment more than once for the same cancer?
Sometimes, yes. It depends on the cancer type, the first treatment, and how long ago it was.
What is re-irradiation, and when is it considered?
Re-irradiation is getting radiation therapy again, often with new techniques. It’s considered for some cancers and patients.
References
- De Bari, B., et al. (2023). Safety and efficacy of reirradiation using advanced radiotherapy techniques: A systematic review. Frontiers in Oncology, 13, 890123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8968587/