Last Updated on November 25, 2025 by Ugurkan Demir

Some people live without a bladder because of medical reasons. Thanks to new medical tech, it’s possible to adjust to this change. It’s important to know the options and what it means for those affected. Can you live without a bladder? Learn about life after a cystectomy, including urinary diversion procedures and long-term outlook.
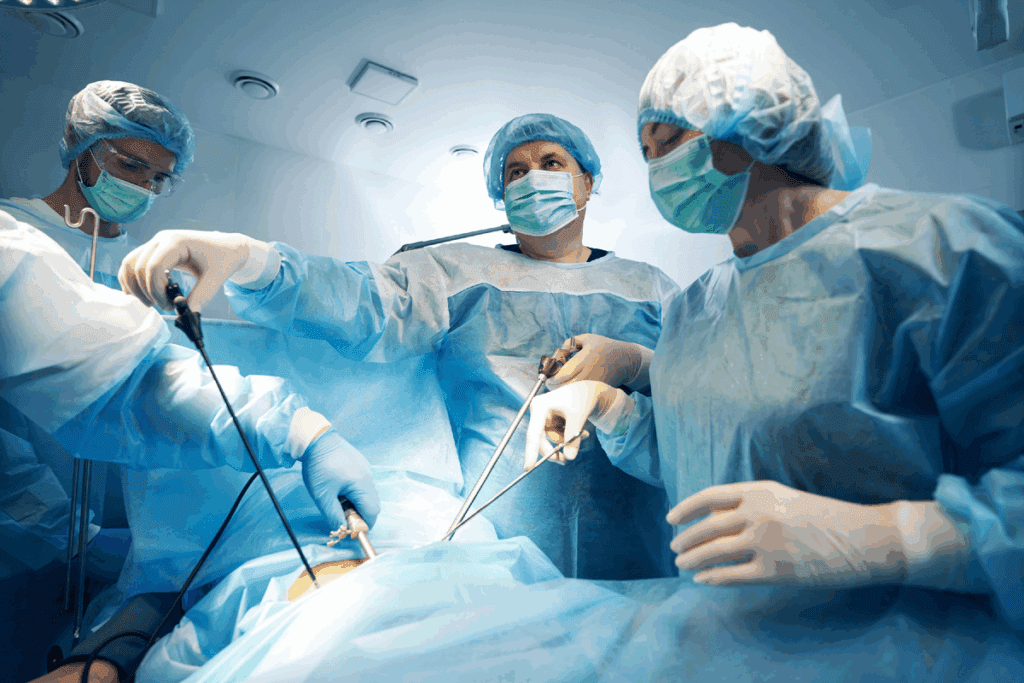
Bladder removal, or cystectomy, is a big surgery for bladder problems. It’s chosen when other treatments don’t work or aren’t possible.
The main reason for this surgery is bladder cancer. Other issues like severe bladder problems or injuries might also require it.
There are many cystectomy procedures, each for different needs.
1. Radical Cystectomy: This is the most common. It removes the bladder, nearby tissues, and lymph nodes.
2. Simple Cystectomy: This removes the bladder but keeps the surrounding tissues and lymph nodes.
Knowing why bladder removal is needed and the types of cystectomy is key for patients facing surgery.
Some people live without a bladder due to medical conditions or surgery. After a bladder removal, they must find new ways to manage their urine. This often means using a urinary diversion, like an ileal conduit, to collect urine.
Those without a bladder face big lifestyle changes. But, with proper medical care, they can live well. It’s key to follow a doctor’s advice on caring for the urinary system and watching for any issues.
They also need to adjust their daily life. This includes managing how much fluid they drink and keeping track of their urine. They must also get used to using a collection device.
Even with these challenges, many people adapt and live healthy, active lives. Understanding their condition and the support available helps them cope.
Helping those without a bladder live well is important. We should be sensitive and give them accurate, helpful information.
Bladder removal surgery, or cystectomy, needs careful preparation. This includes medical tests, choosing a urinary diversion method, and getting emotionally ready. Understanding these steps is key to a successful surgery.
Before surgery, patients must go through many medical tests. These tests check the patient’s health and find any risks. Common tests include:
A leading urologist says, “A thorough preoperative evaluation is key to minimizing risks and improving outcomes.” Preparation is key to a successful surgery.
Choosing the right urinary diversion method is important. There are several options, like ileal conduit, neobladder reconstruction, and continent urinary pouch. Each has its own benefits and drawbacks. The choice depends on the patient’s health, lifestyle, and preferences.
A patient who had surgery says, “Understanding the different urinary diversion options helped me make an informed decision about my care.” It’s essential to discuss these options with your healthcare provider.
Mental and emotional preparation is also vital. Patients may feel anxious or depressed after surgery. Having a support system is important.
“The emotional journey after bladder removal surgery can be challenging, but with the right support, patients can adapt and lead fulfilling lives.”
— Expert in Urological Care
We suggest patients prepare mentally by:
By preparing thoroughly, patients can have a smoother transition and better outcomes after surgery.
Urinary diversion methods are key for patients after bladder removal surgery. The right choice depends on the patient’s health and the surgery’s reason. Knowing the benefits and risks of each method is vital for making informed decisions.
For those who have had their bladder removed, knowing about the ileal conduit procedure is key. It helps manage how they handle urine after surgery. This method creates a new way for urine to leave the body.
The ileal conduit surgery has several important steps. First, a surgeon takes a part of the intestine, usually from the ileum, to make a urine pathway. This pathway is brought to the abdomen to form a stoma. The other end connects to the ureters, which carry urine from the kidneys.
Key Steps in the Ileal Conduit Surgery:
Having an ileal conduit means living with an external stoma and a colostomy bag. This bag collects urine. Patients must learn to care for the stoma and bag to stay clean and avoid problems.
Tips for Managing the Stoma and Colostomy Bag:
It’s vital to take good care of the ileal conduit to avoid issues and live well. This includes watching for infection signs, managing the stoma, and keeping the colostomy bag in good shape.
| Aspect of Care | Description | Frequency |
| Stoma Cleaning | Cleaning the stoma and surrounding area with mild soap and water | Daily |
| Colostomy Bag Maintenance | Emptying the bag and checking for leaks or damage | As needed, typically every 2-4 hours |
| Skin Barrier Application | Applying a skin barrier to protect the skin around the stoma | During stoma cleaning |
Understanding the ileal conduit procedure and its effects helps patients prepare for life after bladder removal surgery. Following the doctor’s care and maintenance advice is key to avoiding complications.
Neobladder reconstruction is a complex surgery. It lets patients keep their urine function almost normal. The surgery makes a new bladder from the small intestine and connects it to the urethra.
The surgery starts by picking a part of the small intestine. This part is then made into a pouch for the new bladder. The surgeon connects this pouch to the urethra, so patients can urinate naturally after they heal.
Making a neobladder needs careful surgery and knowing the patient’s body well. The aim is to make a bladder that works like a normal one.
After the surgery, patients must learn to use their new bladder. They need to know how to urinate right and handle any changes in how they pee. They often get physical therapy to make their muscles stronger for urination.
Getting used to the neobladder takes time, and it can be hard at first. But with the right training and support, many patients can pee almost like normal people. Being patient and persistent is important during this time.
Neobladder surgery has many benefits but also some challenges. Some patients might have trouble with urine leaks or emptying the bladder. Seeing a doctor regularly is key to fix any problems fast.
Also, there’s a chance for long-term problems like metabolic changes or vitamin shortages because of the intestinal tissue. Keeping an eye on these issues and managing them is vital for health.
Continent urinary diversion is a surgery that makes a pouch for urine. It helps people manage their urine without using a bag. This is good for those who have had a cystectomy or have urinary issues.
The surgery takes a part of the intestine, like the ileum, and makes a pouch. The ureters are then connected to this pouch. It’s made with a valve to stop leaks.
People with this surgery need to use a catheter to empty the pouch. They insert a catheter through the stoma to drain urine.
This surgery can make life better for patients. It removes the need for a bag, giving more freedom. But, it comes with risks like infections or pouch failure.
To avoid these risks, patients must be chosen carefully. They need to be watched closely after surgery to manage their condition well.
In summary, continent urinary diversion is a complex surgery. It has benefits but is not for everyone. Patients should talk to their doctor to see if it’s right for them.
Recovering from bladder removal surgery is a journey that needs patience and following doctor’s orders. At first, patients stay in the hospital for a few days to make sure they’re okay. Then, they can start doing things they normally do again.
Right after surgery, patients might feel pain, discomfort, and tiredness. Doctors focus on making the pain go away. They give medicine to help with this.
As the body heals, patients can start doing more things. They might go for short walks and then do more as they get better.
It can take weeks or months to fully recover from bladder removal surgery. Patients need to keep following their doctor’s advice and go to check-ups. This helps them heal well.
Knowing how to recover and following the doctor’s advice is key. This way, patients can get back to their usual life smoothly.
After bladder removal surgery, patients often see a big boost in their quality of life. With the right care and support, they can adjust well and live active, meaningful lives.
Research shows that bladder cancer patients have a 64% to 77% chance of surviving five years. While these numbers are hopeful, it’s key to remember that results can differ. This depends on the patient’s health and the cancer’s stage at diagnosis.
Patients going through bladder removal surgery may feel a mix of emotions. Knowing about survival rates and how others feel can help them prepare for what’s next.
By grasping the effects of bladder removal and the help available, patients can better handle their journey. This can lead to a better quality of life.
We’ve looked into life after bladder removal and found that with the right care, patients can do well. Living without a bladder needs big changes, but new ways to manage urine have helped a lot. This has made life better for many.
Many patients live healthy, active lives with the right care and changes. Today’s options for managing urine help people live well after surgery. This makes life fulfilling.
The secret to success is a complete plan that includes good medical care, the right way to manage urine, and ongoing support. Knowing the options and challenges helps patients make good choices. This way, they can enjoy a good quality of life.
Yes, many people do. They adapt to life without a bladder. The right care and urinary diversion method help them live well.
Options include ileal conduit, neobladder reconstruction, and continent urinary pouch. Each has its own benefits and challenges. The right choice depends on your health and needs.
Recovery time varies. Most people take weeks to months to get better. The hospital stay is usually 1–2 weeks. Full recovery can take up to 6 weeks or more.
No, urination changes after bladder removal. You might need a urinary diversion method like an ileal conduit or neobladder reconstruction.
Long-term effects include changes in urination and possible complications. But, with proper care, many people live active and fulfilling lives.
Managing involves regular cleaning and care of the stoma or urinary diversion site. Your healthcare provider will guide you on how to manage it.
Yes, with proper care and management, you can lead an active and normal life. This includes sports, traveling, and other activities.
Neobladder reconstruction offers a more natural urination experience. It may also be more aesthetically pleasing for some patients.
Risks include infection, bleeding, and complications. Your healthcare provider will discuss these risks in more detail.
Emotional changes are normal after bladder removal. Support from healthcare professionals, family, and friends can help you cope.
Predicting the Probability of 90-day Survival in Elderly Bladder Cancer Patients Treated with Radical Cystectomy – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6472701/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!