Last Updated on November 26, 2025 by Bilal Hasdemir
The digestive system is key to our health. It turns the food we eat into something our bodies can use.
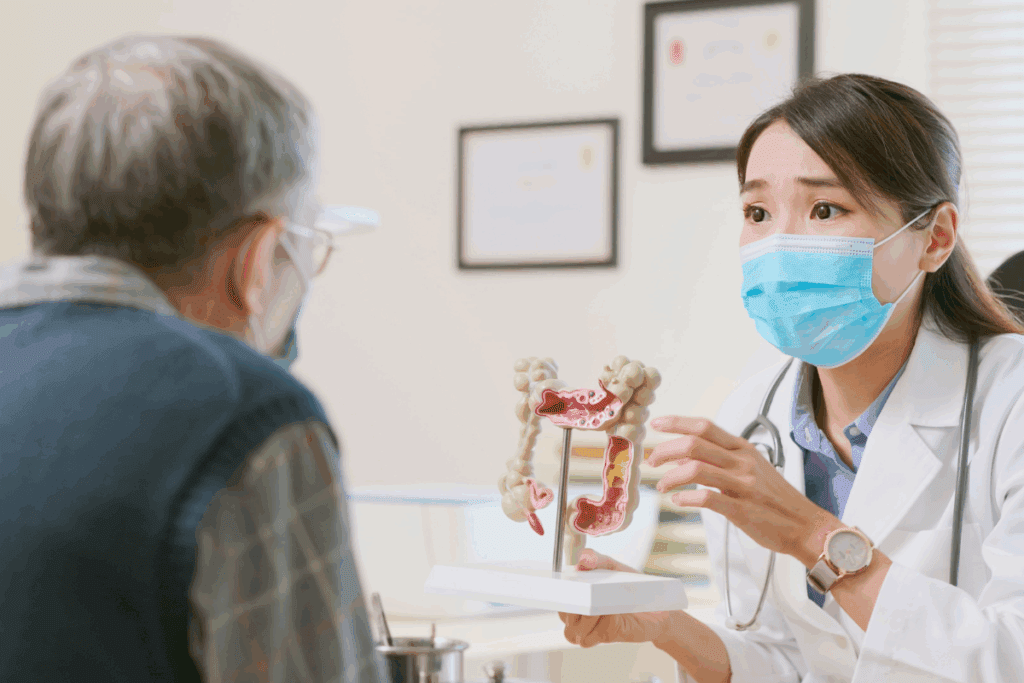
The small and large intestines help digest food and keep our body balanced. They also remove waste. The large intestine, or colon, mainly absorbs water and salts. But it’s possible to live without your large intestine if needed.
Knowing what life is like without intestines is important for those facing this situation. Liv Hospital offers trusted, patient-focused care. This helps patients understand can live without a small intestine and its effects on health.

The digestive system, with the intestines at its core, is key for breaking down food and getting vital nutrients. This complex process involves many organs working together. They break down food, absorb nutrients, and get rid of waste.
The human digestive system is a complex process. It starts in the mouth and goes through the esophagus, stomach, small intestine, and large intestine. It ends at the anus. Each part has a special role in digesting food and absorbing nutrients.
Food starts being broken down in the mouth. Chewing and saliva with enzymes help break down carbs. Then, it goes down the esophagus into the stomach. Here, stomach acids and enzymes further break it down.
“The digestive system’s ability to break down food into essential nutrients is fundamental to human health and survival.”
After the stomach, the food goes to the small intestine. This is where most nutrient absorption happens. The small intestine has villi, which increase the surface area for better absorption.
The small and large intestines work together. The small intestine, 20 to 22 feet long, absorbs most nutrients. It gets vitamins, minerals, and other essential nutrients into the bloodstream.
The large intestine, about 5 feet long, absorbs water and electrolytes. It also houses a big part of the gut microbiome. This microbiome is important for fermentation and making vitamins.
| Intestine | Primary Functions | Length |
| Small Intestine | Nutrient Absorption | 20-22 feet |
| Large Intestine | Water Absorption, Electrolyte Balance, Fermentation | 5 feet |
In summary, the intestines are vital for digestion. The small intestine absorbs nutrients, and the large intestine absorbs water and houses the gut microbiome. Their work together is key to nutritional balance and health.

It’s key to know how the large intestine works for our health. The large intestine, or colon, is a long tube in our belly. It helps our body digest food by doing several important jobs.
The colon is great at soaking up water and salts. It pulls water and salts like potassium and sodium from waste. This helps make the waste more solid and keeps our body’s fluids balanced. It’s important for avoiding dehydration.
The colon makes and holds onto stool. After water is absorbed, the waste turns into solid stool. The colon keeps this stool until we go to the bathroom. Muscles in the colon help push the stool towards the rectum.
Making and storing stool is a complex task. It needs the work of many muscles and nerves. Problems here can cause constipation or diarrhea.
The gut microbiome is full of tiny living things in the colon. These tiny beings help break down food, make vitamins, and keep our immune system healthy. A healthy gut is key to good digestion and overall health.
But if the balance of these tiny beings gets off, it can cause health problems. Eating right and living healthy helps keep the gut in balance.
Some medical conditions force doctors to remove the colon, raising questions about life without it. The large intestine is key to digestion. Yet, removing it can save lives for those with severe diseases.
Diseases like ulcerative colitis, Crohn’s colitis, and familial polyposis may require colon removal. These conditions can be very serious and even deadly if not treated right away.
Ulcerative colitis causes inflammation and ulcers in the colon. It leads to diarrhea, pain, and weight loss. Crohn’s colitis can affect any part of the gut, but it is more serious when it hits the colon.
A colectomy is surgery to remove part or all of the colon. There are several types:
Each procedure has its own reasons and benefits. The choice depends on the condition and the patient’s health.
Many people adjust well after a colectomy. They might have more frequent, watery stools and need constant medical advice. The success of colectomy varies based on the condition and surgery type.
Research shows good outcomes for those with ulcerative colitis and familial polyposis after colectomy. Their quality of life improves a lot. But, they need ongoing care and might face complications.
Colon removal surgery, or colectomy, starts a new chapter in life. It’s a big change that affects health and daily life. The colon’s removal is a major surgery.
After surgery, patients face many changes. Bowel movements change first. Stools may be watery until the body adjusts.
The small intestine learns to absorb fluids better over time. But this takes some getting used to.
Ostomy and Its Management: Some patients get an ostomy. This is a surgical opening in the abdomen for stool. It needs special care and hygiene.
There are various ostomies, like ileostomies and colostomies. The type depends on the surgery. Managing an ostomy means using the right bags and skin care to avoid problems.
Long-term, life without a colon brings changes. Bowel habits, nutrition, and health may differ. If the anus is kept, a J-pouch might be created for continence.
| Aspect | Changes After Colon Removal |
| Bowel Movements | More frequent and watery initially, potentially becoming more solid as the body adapts |
| Nutritional Absorption | The small intestine compensates for the loss of the colon, but some nutrients may be malabsorbed |
| Ostomy Management | Requires learning new skills for hygiene and bag management |
Understanding these changes is key to a good life after surgery. With the right care, people can live well and enjoy life.
The small intestine is key to absorbing most nutrients in our bodies. It’s a long, thin tube with three parts: the duodenum, jejunum, and ileum. Each part has special jobs to help digest food and absorb nutrients.
The small intestine’s walls have finger-like projections called villi. These increase the area for absorbing nutrients. The villi are full of blood vessels that carry absorbed nutrients to the bloodstream. Nutrient absorption happens thanks to specialized cells called enterocytes on the villi.
This part of the intestine absorbs many nutrients, like carbs, proteins, fats, vitamins, and minerals. It’s very good at it, absorbing up to 90% of what we eat.
The small intestine makes digestive enzymes to break down food. These enzymes are made by cells lining the intestine and released into the lumen. There, they mix with food.
Important enzymes like lactase, sucrase, and maltase break down carbs into simple sugars. Other enzymes, like enterokinase, help activate pancreatic enzymes to break down proteins and fats.
The small intestine is vital for our immune system. It has a lot of immune cells in the gut-associated lymphoid tissue (GALT). The GALT helps fight off pathogens and toxins from food and drink.
The small intestine also makes antibodies and immune factors. These help neutralize pathogens and keep the gut microbiome healthy. The gut microbiome is full of trillions of microorganisms that are essential for our health.
| Function | Description | Importance |
| Nutrient Absorption | Absorption of carbohydrates, proteins, fats, vitamins, and minerals | Essential for energy and nutrient supply |
| Digestive Enzyme Production | Production of enzymes to break down food | Critical for nutrient breakdown and absorption |
| Immune System Functions | Production of antibodies and immune factors | Vital for gut health and immune defense |
Living without a small intestine is rare. It usually happens due to severe damage or disease. The small intestine is key to absorbing nutrients. Without it, you can face big nutritional problems.
Several medical conditions may require the removal of the small intestine, including:
These conditions can lead to a significant loss of intestinal function. This makes it hard for the body to absorb essential nutrients.
When a big part of the small intestine is removed, patients may develop short bowel syndrome. This condition is marked by poor nutrient absorption. It can cause malnutrition and dehydration.
The severity of short bowel syndrome depends on how much and where the intestine was removed. Patients often need special nutritional support.
The survival rate for individuals without a small intestine varies. It depends on the cause of removal, how much was removed, and the patient’s health.
Medical nutrition and intestinal rehabilitation have improved outcomes. Some may need total parenteral nutrition (TPN). Others might be candidates for intestinal transplantation.
A study on patients with short bowel syndrome showed different survival rates. This highlights the need for personalized care and management.
When a lot of the intestine is lost, doctors must act fast. This loss can happen due to surgery or illness. It means finding new ways to get nutrients and to digest food.
Total Parenteral Nutrition (TPN) gives nutrients through an IV. It’s great when the intestine isn’t working right or is gone.
TPN sends a nutrient-rich solution straight into the blood. This way, the body gets the nutrients it needs without using the digestive system.
Key components of TPN include:
In some cases, getting a new intestine might be an option. This is a big surgery where a healthy intestine from a donor is put in.
Doctors might suggest this if other treatments like TPN don’t work. It’s a big decision that needs careful thought and matching of the donor and recipient.
New treatments for intestinal loss are being explored. This includes things like tissue engineering and regenerative medicine. These new methods aim to fix the intestine and improve life for those affected.
Some exciting research areas include:
As medical science keeps getting better, managing intestinal loss is becoming more advanced. This brings hope to those dealing with this condition.
Surgery on the intestines can greatly affect a patient’s health. It needs careful care after surgery. Removing or changing parts of the intestines, like in a colectomy or small bowel resection, can cause problems. It’s important for patients and doctors to know about these issues and how to handle them.
After intestinal surgery, patients might face several health issues. These include bleeding, blood clots, infection, injury to nearby organs, and tears in the sutures that fix the digestive system. Handling these problems often needs a team effort from doctors, nurses, and other health experts.
One big risk after intestinal surgery is malnutrition. The intestines are key for absorbing nutrients, and changes to them can affect this. Patients might need special diets or supplements to avoid malnutrition. Also, dehydration is a risk, mainly if they have frequent or watery stools. It’s important to drink enough water.
After intestinal surgery, ongoing care is key. Regular visits to healthcare providers help catch and treat late problems, like adhesions, bowel obstruction, or vitamin deficiencies. Keeping an eye on nutrition and overall health is also important for a good quality of life.
| Complication | Management Strategy |
| Bleeding | Immediate surgical intervention or transfusion |
| Infection | Antibiotics, possible drainage of abscess |
| Malnutrition | Dietary adjustments, nutritional supplements |
| Dehydration | Increased fluid intake, intravenous fluids if necessary |
When intestines are removed or severely compromised, nutritional intake becomes a critical concern. Individuals facing such significant changes must adapt their diets to manage their condition effectively.
One of the primary challenges is malabsorption, as the intestines play a key role in nutrient absorption. Without a fully functional intestinal system, patients may experience deficiencies in vital nutrients. A malabsorptive bariatric surgery, such as gastric bypass, illustrates this issue by limiting the calories absorbed by the small intestine.
To address these challenges, patients often require supplemental nutrition. This can include vitamins and minerals that are not being adequately absorbed through the diet alone. Healthcare providers work closely with patients to identify the necessary supplements and monitor their nutritional status.
Dietary adjustments are key to managing life without intestines. Patients are often advised to consume small, frequent meals to ease digestion and enhance nutrient absorption. The focus is on nutrient-dense foods that are easy to digest, such as lean proteins, cooked vegetables, and certain fruits.
Avoiding foods high in sugar and fat is also recommended, as they can be difficult to digest and may exacerbate symptoms.
In addition to dietary changes, supplements and medical nutrition play a vital role. Total Parenteral Nutrition (TPN) is an example of medical nutrition that provides essential nutrients intravenously, bypassing the digestive system altogether.
Patients may also require specific vitamins and mineral supplements to address deficiencies. Regular monitoring by healthcare professionals is essential to adjust these supplements as needed and ensure that the patient’s nutritional needs are being met.
By understanding the dietary considerations and working closely with healthcare providers, individuals without intestines can manage their condition and maintain a level of nutritional health.
Life without intestines changes in many ways, not just physically. People who have had their intestines removed face big challenges. They must deal with health issues and emotional and social impacts.
Removing intestines, like creating an ostomy, can change how you see yourself. You might feel insecure or embarrassed about your body or the ostomy bag.
It’s key to get support and learn how to manage these feelings. Counseling, support groups, and educational resources can help you understand and adjust to your new life.
Intestinal loss affects more than just you. It can strain relationships with family and friends. Medical appointments, diet changes, and ostomy issues can be tough to handle.
Talking openly and educating others about your condition can help. This way, your loved ones can offer real support.
Support groups are vital for adjusting to life without intestines. They offer a place to share experiences, get advice, and find emotional support from others who understand.
| Resource Type | Description | Benefits |
| Support Groups | Community-based groups for individuals with similar experiences | Emotional support, shared knowledge, and coping strategies |
| Online Forums | Virtual platforms for discussion and information sharing | Accessibility, anonymity, and a wide range of perspectives |
| Counseling Services | Professional guidance for coping with emotional and psychological impacts | Personalized support, coping strategies, and mental health management |
Using these resources can help you deal with the challenges of living without intestines. It can improve your quality and mental health.
It’s important to know how vital the intestines are for our health. They play a key role in digestion and keeping us well. The question of living without a small or large intestine is complex.
Some people with very short intestines can survive with the right care and support. But losing both intestines is not possible. Those who lose their large intestine face big changes in their life.
Those without a small intestine also face big challenges. They might need to get nutrients through an IV or get a new intestine. How well someone can live without intestines depends on many things.
Knowing about the intestines and what happens when they’re lost can help people cope better. It can improve their life, even with the challenges of missing parts of their intestines.
Yes, you can live without a large intestine. Your body can adjust to its loss. With the right care and lifestyle changes, you can live normally.
After removing your colon, your body needs to adapt. You might need an ostomy for waste elimination. You’ll also have to make big changes in your diet.
Surviving without a small intestine is very hard. But, with total parenteral nutrition (TPN) or intestinal transplant, it’s possible.
Living without a colon means big changes in your life. You’ll need to change your diet and manage an ostomy if needed. Regular doctor visits are also key to avoiding problems.
Living without intestines is technically possible. But
it’s very hard. You’ll need a lot of medical help, like TPN or a
transplant, to keep living.
The large intestine absorbs water and electrolytes. It stores and eliminates stool. It also has a vital gut microbiome. Removing it is challenging, but it’s possible to live without it.
Living without bowels is very hard. You’ll likely need total parenteral nutrition (TPN) or other big medical steps to survive.
Life without a small intestine depends a lot on medical help. You’ll need TPN or a transplant. Managing your nutrition and health is key to survival.
Living without a colon means finding new ways to manage waste. You’ll need to change your diet a lot. Regular doctor visits are also important.
Living without a colon is hard, but many people do it. With the right care, lifestyle changes, and support, you can live a normal life.
People without intestines need special nutrition, like TPN. They must carefully watch their diet to avoid malnutrition and dehydration.
Yes, there are support groups for those without intestines. They offer emotional support, practical advice, and a sense of community.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!