Last Updated on October 31, 2025 by

We often hear about cancer in situ, also known as stage 0 cancer, but what does it really mean? Carcinoma in situ is a condition where abnormal cells look like cancer but haven’t spread to other tissues.
This condition offers a chance for early treatment because it’s the first stage of cancer. It’s thought to be 100% curable if caught early. Knowing about cancer in situ helps in managing the disease early and stopping it from getting worse.
Grasping cancer in situ starts with its basic definition. It’s a stage 0 cancer where cells are present but haven’t spread. They stay in their original place.
The term “in situ” comes from Latin, meaning “in its original place.” This etymology is key to understanding cancer in situ. It shows the disease is localized.
In situ cancers stay in the epithelial layer. They don’t invade surrounding tissues. This is important for diagnosis and treatment.
Medically, cancer in situ is stage 0 cancer. This means it’s in its early stage. It hasn’t invaded deeper tissues or spread to other parts of the body.
Stage 0 cancer is a precursor to invasive cancer. Catching it early is key for prevention. Early detection and intervention are vital.
The main difference of cancer in situ is its non-invasive nature. Unlike invasive cancer, it doesn’t spread. It stays in one place.
Here’s a table to show the differences:
| Characteristics | Cancer In Situ | Invasive Cancer |
| Spread | Localized, no invasion | Spreads beyond original site |
| Stage | Stage 0 | Stage I and beyond |
| Treatment Approach | Often less aggressive, may include surveillance | More aggressive, includes surgery, chemotherapy, etc. |
Cancer in situ is a critical condition. It needs careful monitoring and treatment to stop it from becoming invasive cancer. Knowing its definition and nature is the first step in managing it well.

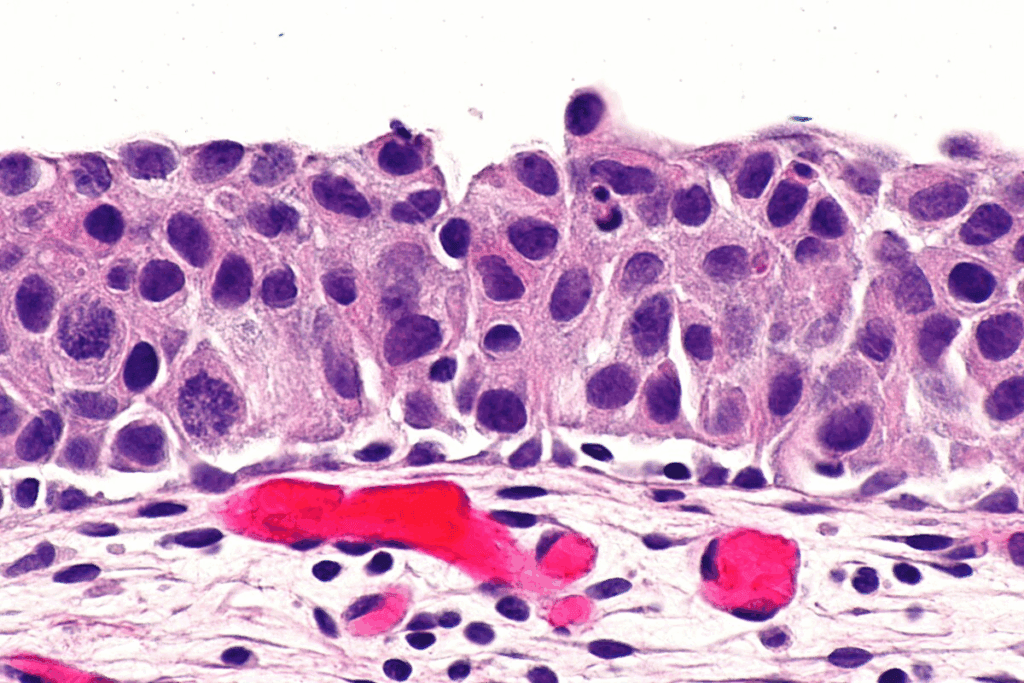
It’s important to know how cancer in situ looks under a microscope to diagnose it early. This condition is a type of tumor that hasn’t spread to other tissues yet. At the cellular level, it shows unique traits that set it apart from normal cells and invasive cancer cells.
When we look at cancer in situ cells under a microscope, they show abnormal cellular morphology. This means they are different in size, shape, and how they stain. They often have enlarged nuclei and a higher ratio of nucleus to cytoplasm, showing they are not normal.
The look of cancer in situ cells can change based on the type and where it is in the body.
The changes in cancer in situ cells include:
A key feature of cancer in situ is that it stays within the basement membrane. The basement membrane is a thin layer of fibers that keeps epithelial cells from the underlying tissue. In cancer in situ, the cells don’t cross this membrane, unlike in invasive cancer.
This containment is important for diagnosis and treatment. It shows that cancer in situ is a pre-invasive condition. If caught and treated early, it can often be cured.
Understanding the microscopic look and the basement membrane containment of cancer in situ is key. It helps in early detection and managing this condition effectively.
It’s important to know about the different types of cancer in situ. This knowledge helps in diagnosing and treating the disease. Cancer in situ can appear in various ways, depending on where it is and the type of tissue involved.
Ductal carcinoma in situ (DCIS) is a type of breast cancer. It happens when cancer cells stay in the milk ducts. DCIS is not invasive because the cancer cells don’t spread to the rest of the breast. It’s often found during mammograms and treated with surgery or radiation.
Lobular carcinoma in situ (LCIS) is a condition in the breast’s lobules. LCIS is not true cancer but shows a higher risk of breast cancer. People with LCIS need to be watched closely for any changes.
There are other types of cancer in situ, like cervical, skin, and bladder cancer. Each type has its own features and health effects. For example, cervical cancer in situ is found with Pap smear tests. Skin cancer in situ is spotted by looking at the skin.
Cancer in situ can happen in many parts of the body. Knowing where it often occurs is key to catching it early. This knowledge helps in treating it before it gets worse.
Breast cancer in situ is a big worry. It has two main types: Ductal Carcinoma In Situ (DCIS) and Lobular Carcinoma In Situ (LCIS). DCIS affects the ducts, while LCIS affects the lobules.
DCIS makes up about 20% of breast cancer cases in the U.S. Thanks to mammograms, catching it early has greatly improved treatment outcomes.
Cervical cancer in situ, or CIN, means abnormal cells on the cervix. If not treated, these can turn into invasive cancer.
Pap smear tests help find CIN early. This allows for quick action and lowers the risk of invasive cancer.
Bowen’s disease is a skin cancer in situ. It shows up as abnormal cell growth on the skin. It’s linked to too much sun and can turn into invasive cancer if not treated.
Spotting and treating Bowen’s disease early is key to stopping it from getting worse.
Cancer in situ can also happen in places like the mouth, esophagus, and urinary tract. Each has its own risk factors and symptoms. This highlights the importance of staying informed and getting regular check-ups.
| Location | Type of Cancer In Situ | Common Risk Factors |
| Breast | Ductal Carcinoma In Situ (DCIS), Lobular Carcinoma In Situ (LCIS) | Family history, genetic mutations (BRCA1, BRCA2) |
| Cervix | Cervical Intraepithelial Neoplasia (CIN) | HPV infection, smoking, immunosuppression |
| Skin | Bowen’s Disease | Prolonged sun exposure, fair skin, immunosuppression |
Knowing where cancer in situ often occurs is vital for prevention and treatment. Recognizing risk factors and symptoms in different areas helps people act early. This can lead to better outcomes.
Diagnosing cancer in situ involves several steps. We use screening methods and diagnostic procedures to find abnormal cell changes early. This helps prevent cancer from becoming invasive.
Screening is key in catching cancer in situ early. Here are some common methods:
These methods help us find cancer in situ early, when it’s easier to treat.
When screening shows possible issues, we do biopsies to get tissue samples. The main biopsy techniques are:
These biopsies give us tissue samples that help diagnose cancer in situ.
Pathological examination analyzes tissue samples from biopsies. It checks for abnormal cell changes. Pathologists look for specific markers and characteristics that show cancer in situ. They examine:
By looking at these factors, pathologists confirm cancer in situ and give details on the type and extent of the disease.
Cancer in situ is influenced by many risk factors. These can be genetic, environmental, or lifestyle-related. Knowing these factors helps in early detection and prevention.
Genetics play a big role in cancer in situ. People with a family history of cancer are at higher risk. Certain genes, like BRCA1 and BRCA2 for breast cancer, raise the risk a lot.
| Genetic Mutation | Cancer Type | Increased Risk |
| BRCA1 | Breast Cancer | High |
| BRCA2 | Breast Cancer | High |
Environmental factors are also key. Certain chemicals and radiation can raise cancer in situ risk. UV radiation, for example, is a risk for skin cancer in situ.
Common Environmental Risk Factors:
Lifestyle and behavior also matter. Smoking, diet, exercise, and alcohol use can affect risk. A diet full of processed foods and lacking fruits and veggies can increase risk.
Lifestyle Modifications to Reduce Risk:
By tackling these risk factors, people can lower their cancer in situ risk.
It’s key to know how cancer in situ presents early for treatment. This condition has cancer cells but they haven’t spread. The symptoms, or lack of them, are important for diagnosis and care.
Many in situ cancers don’t show symptoms. This makes regular check-ups and screenings critical for catching them early. For example, ductal carcinoma in situ (DCIS) in the breast is often found during mammograms before symptoms show.
Screening is vital for catching cancer in situ before it becomes invasive. Even without symptoms, harmful cells can be present. So, taking proactive steps is important.
While many are asymptomatic, some cancers in situ have specific warning signs. For example:
These signs can vary by location. Knowing these signs can lead people to get checked by a doctor.
It’s important for people to know their bodies and report any unusual changes to their doctor. Early detection greatly improves treatment outcomes.
We suggest following screening guidelines and talking to your doctor about your risk factors. This helps ensure early detection and management of cancer in situ.
Treatment for cancer in situ involves surgery, radiation, and hormonal treatments. The right treatment depends on the cancer type, location, and the patient’s health.
Surgery is often the first step to remove cancerous cells. For breast cancer, lumpectomy or mastectomy might be used. For cervical cancer, conization or LEEP (Loop Electrosurgical Excision Procedure) are common.
Dr. Jane Smith, a top oncologist, says, “Surgery is usually the best way to treat cancer in situ early.”
“Early detection and surgical removal can significantly improve outcomes for patients with cancer in situ.”
Radiation therapy can be used after surgery or alone. External beam radiation therapy and brachytherapy are two main types used for cancer in situ.
For hormone-positive breast cancer, hormonal therapy is used. Medications like Tamoxifen or Anastrozole help prevent cancer from coming back.
Active surveillance is sometimes recommended. It involves regular tests and biopsies to watch the cancer. This is for low-risk cancer or when immediate treatment isn’t best.
Choosing the right treatment for cancer in situ is key for the best results. Patients should work closely with their healthcare team to make the best decisions for their care.
Cancer in situ progression rates change a lot. They depend on the type and where the cancer is. Knowing these rates helps doctors choose the right treatment and improve patient care.
Many things can make cancer in situ turn into invasive cancer. These include genetic predispositions, environmental exposures, and lifestyle factors. For example, people with a family history of cancer might be at higher risk. Also, being exposed to certain harmful substances can raise the risk.
Biomarkers and molecular characteristics of the cancer are also key. New tests help find these markers. This lets doctors better understand the risk.
The rate at which cancer in situ turns into invasive cancer changes a lot. For instance, ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS) have different rates. Also, cancers in different places like the breast, cervix, or skin have different rates too.
It’s important to know these differences to make good treatment plans. We’ll look at the specific rates for different cancers and what it means for treatment.
By knowing what affects progression and how it varies, doctors can give more tailored care.
The outlook for people with cancer in situ is very positive. This is because of the progress in medical treatments. Early detection means a high chance of successful treatment, often stopping the cancer from becoming invasive.
Survival rates for cancer in situ are encouraging. For example, ductal carcinoma in situ (DCIS), a common breast cancer type, has a high survival rate with proper treatment. Research shows that managing DCIS well can lower the risk of it turning into invasive cancer.
| Type of Cancer In Situ | 5-Year Survival Rate | 10-Year Survival Rate |
| Ductal Carcinoma In Situ (DCIS) | 98-100% | 95-98% |
| Lobular Carcinoma In Situ (LCIS) | 95-98% | 90-95% |
| Cervical Cancer In Situ | 100% | 100% |
Table: Survival rates for different types of cancer in situ. These statistics are based on data from various cancer research studies and may vary depending on individual circumstances.
Survival rates are important, but so is quality of life for those with cancer in situ. Treatment choices can affect a patient’s life quality, making it key to talk about these with doctors. For instance, surgery, though effective, can affect a patient’s physical and emotional health.
Quality of life includes physical health, emotional well-being, and social functioning. People with cancer in situ should know how their treatments might affect these areas. They should talk about any worries with their healthcare team.
Understanding the prognosis and long-term outlook helps individuals with cancer in situ make informed decisions. They can balance the need for effective treatment with the goal of maintaining a good quality of life.
Preventing cancer in situ is key to good health. It involves screenings, lifestyle changes, and preventive steps. By using these methods, people can lower their cancer risk.
Screenings are vital for cancer prevention. Each age group has its own screening advice. For example, women over 40 should get a mammogram every year for breast cancer checks.
For cervical cancer, women start with Pap smears at 21. These guidelines help catch cancer early.
| Age Group | Screening Recommendation |
| 21-29 | Pap smear every 3 years |
| 30-65 | Pap smear and HPV test every 5 years or Pap smear alone every 3 years |
| 40+ | Mammogram annually |
Making lifestyle changes is important for cancer prevention. Keeping a healthy weight through diet and exercise helps. Also, not smoking and drinking less alcohol are key.
Eating more fruits, veggies, and whole grains is good. Avoiding processed and red meats is also beneficial. Regular exercise helps keep weight in check and lowers cancer risk.
Preventive meds or interventions might be suggested. For example, tamoxifen or raloxifene may be given to high-risk breast cancer women. Knowing the pros and cons of these options is important.
By following screening guidelines, making lifestyle changes, and using preventive meds when needed, you can lower your cancer risk. It’s important to talk to your doctor about the best plan for you.
Understanding cancer in situ is key for early detection and effective management. We’ve looked at its definition, types, diagnosis, and treatments. This gives a clear summary of the main points.
Knowing the cellular traits and risk factors of cancer in situ helps in prevention and early action. We’ve learned that cancer in situ is a critical stage. It’s when the disease is contained and can often be cured.
We’ve talked about the role of screening, biopsies, and pathological exams in diagnosing cancer in situ. There are also treatments like surgery, radiation, and active surveillance to manage it.
In conclusion, awareness, early detection, and proper management are vital to stop cancer from spreading. By understanding cancer in situ, we can better support those affected. This helps us navigate the complexities of cancer care.
“In situ” comes from Latin and means “in its original place.” In cancer, it means abnormal cells that haven’t spread. This is also known as stage 0 cancer.
Cancer in situ, or stage 0 cancer, is when abnormal cells are in one place. They haven’t spread to other areas or invaded nearby tissues.
Cancer in situ is non-invasive, with cells staying in one place. Invasive cancer, on the other hand, spreads to other areas, invading tissues and possibly metastasizing.
Common types include ductal carcinoma in situ (DCIS), lobular carcinoma in situ (LCIS), cervical cancer in situ, and skin cancer in situ (Bowen’s disease).
It’s diagnosed through screening like mammograms, Pap smears, or biopsies. Then, a pathologist checks the cells to confirm the diagnosis.
Risk factors include genetic predispositions, environmental exposures, and lifestyle choices. These can vary by cancer type and location.
Yes, it can be treated. Options include surgery, radiation, medication, or active surveillance. The choice depends on the cancer type, location, and patient factors.
The prognosis is usually excellent, with high survival rates. It’s a non-invasive condition. But, the risk of becoming invasive cancer varies by type and location.
Prevention includes following screening guidelines, making lifestyle changes, and sometimes using preventive medications or interventions.
Carcinoma in situ is another term for cancer in situ. It refers to abnormal cells that haven’t invaded surrounding tissues.
“Ca in situ” is short for “carcinoma in situ.” It means cancer that stays in its original place and hasn’t spread.
National Center for Biotechnology Information. (2025). What Is Cancer In Situ Definition and Meaning. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5161057/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!