Last Updated on October 21, 2025 by mcelik
Hematologic malignancies are cancers that affect the blood, bone marrow, and lymph nodes. They are a big health problem worldwide. These cancers, like leukemia, lymphoma, and myeloma, affect millions of people.
Looking into hematology shows us how important it is to understand these diseases. Hematology, the study of blood disorders, helps us diagnose and manage these cancers.
Haematology is the study of blood and its disorders. It’s key to understanding blood-related cancers. This branch of medicine deals with diagnosing, treating, and managing blood diseases.
Haematology is a medical field that studies blood and its disorders. It focuses on diagnosing and treating blood and bone marrow conditions. Bone marrow is the spongy tissue in bones where blood cells are made.
Haematologists are doctors who specialize in blood disorders, including cancers. They understand how blood components interact and how diseases affect them.
Oncology is the study, diagnosis, treatment, and management of cancer. Haematology and oncology are closely related when it comes to blood cancers.
Blood cancers include leukemia, lymphoma, and myeloma. Haematologists and oncologists work together to care for patients with these cancers.
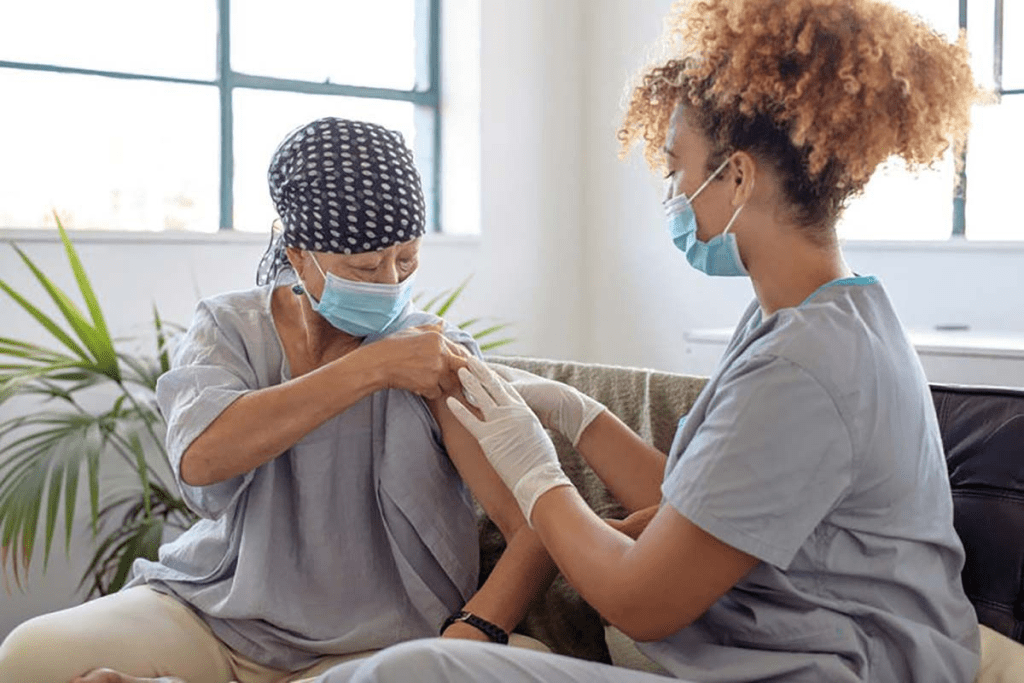
A hematologist is a doctor who specializes in blood disorders. They are key in managing blood cancers. They interpret lab tests and create treatment plans.
Hematologists handle all parts of patient care, from diagnosis to follow-up. They work with a team of healthcare professionals to give patients the best care.
Blood cancer, also known as hematologic malignancy, is a group of diseases. They affect the blood, bone marrow, and lymph nodes. These cancers disrupt the normal production of blood cells, causing health problems. We will explain how blood cancers differ from solid tumors and the role of blood and bone marrow.
Blood cancers start in the blood-forming cells of the bone marrow. They happen when blood cells grow abnormally. This can mess up how the body fights infections and makes blood cells. Leukemia, lymphoma, and myeloma are the main types, each affecting the body differently.
“The diagnosis of a hematologic malignancy can be life-altering, but understanding the disease is the first step towards managing it,” says a leading hematologist. This quote shows how important education and awareness are in dealing with blood cancers.
Blood cancers spread throughout the body, unlike solid tumors that form in one place. This changes how we diagnose and treat blood cancers compared to solid tumors.
The bone marrow is spongy tissue in bones like the hips and thighbones. It makes blood cells. In blood cancers, the bone marrow makes abnormal blood cells. This can cause anemia, infections, and bleeding problems.
It’s key to understand the link between blood, bone marrow, and lymphatic system. This helps us see how blood cancers develop and grow. It also guides treatment and management of these diseases.
Haematological malignancies are cancers that affect the blood, bone marrow, and lymphatic system. They are divided into several main types. These types are based on the cells they target and their specific traits.
Leukemia starts in the bone marrow’s blood-forming cells. It causes abnormal white blood cells to grow too much. This can lead to anemia, infections, and bleeding problems.
There are different kinds of leukemia. For example, Acute Myeloid Leukemia (AML) and Chronic Lymphocytic Leukemia (CLL) are two common ones.
Lymphoma begins in the lymph system, which is part of the immune system. It has two main types: Hodgkin lymphoma and Non-Hodgkin lymphoma. Each type has its own treatment and characteristics.
Lymphomas can make lymph nodes swell. They can also affect other organs.
Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes too many abnormal plasma cells, leading to bone damage, anemia, and infections. Multiple myeloma often starts with a condition called monoclonal gammopathy of undetermined significance (MGUS).
Myelodysplastic syndromes (MDS) are disorders with poorly formed or dysfunctional blood cells. They often lead to bone marrow failure. MDS can turn into Acute Myeloid Leukemia (AML).
MDS causes anemia, low white blood cells, and low platelets. Understanding these main types of haematological malignancies is key for diagnosis and treatment. Each type has its own risk factors and treatment options. This shows why a personalized care plan is so important.
Leukemia is not just one disease but a group of blood cancers. They affect different parts of the blood and bone marrow. The abnormal growth of blood cells can lead to health problems, depending on the type and how it progresses.
Acute Myeloid Leukemia (AML) is a fast-progressing blood cancer. It affects the myeloid cells in the bone marrow. Symptoms include fatigue, infections, and easy bruising. Treatment usually involves chemotherapy and sometimes a stem cell transplant.
Acute Lymphoblastic Leukemia (ALL) is an aggressive blood cancer. It affects the lymphoid cells. It’s the most common leukemia in kids but can also happen in adults. Treatment approaches often include chemotherapy and targeted therapy.
Chronic Myeloid Leukemia (CML) is a slower-progressing leukemia. It affects the myeloid cells and is marked by the Philadelphia chromosome. Treatment often involves targeted therapy, like tyrosine kinase inhibitors.
Chronic Lymphocytic Leukemia (CLL) is a slow-progressing leukemia. It affects the lymphoid cells and is more common in older adults. Symptoms can be mild and may not need immediate treatment. Treatment varies based on the disease stage and patient health.
In conclusion, knowing the different types of leukemia is key for effective diagnosis and treatment. Each type has its own characteristics and needs a specific approach to manage the disease.
Lymphoma is a group of blood cancers found in the lymphatic system. It’s divided into Hodgkin and non-Hodgkin lymphoma. These cancers start when lymphocytes, a type of white blood cell, grow out of control. We’ll look at the differences between Hodgkin and non-Hodgkin lymphoma, their symptoms, how they’re diagnosed, and treatment options.
Hodgkin lymphoma, also known as Hodgkin’s disease, is marked by Reed-Sternberg cells in lymph nodes. These cells are much larger than normal lymphocytes. It spreads in an orderly fashion from one lymph node group to the next.
Symptoms and Diagnosis: Symptoms include painless swelling in the neck, armpits, or groin, fever, night sweats, and weight loss. A lymph node biopsy confirms the disease by finding Reed-Sternberg cells.
Non-Hodgkin lymphoma (NHL) is a diverse group without Reed-Sternberg cells. It can occur in any part of the body with lymphoid tissue, like lymph nodes, spleen, or the gastrointestinal tract.
Types and Treatment: NHL has over 60 subtypes, from slow-growing to aggressive. Treatment depends on the subtype, stage, and patient factors. It can include chemotherapy, radiation, immunotherapy, or a mix of these.
| Characteristics | Hodgkin Lymphoma | Non-Hodgkin Lymphoma |
| Presence of Reed-Sternberg Cells | Yes | No |
| Spread Pattern | Orderly | Variable |
| Subtypes | Fewer subtypes | Over 60 subtypes |
| Treatment Approach | Often chemotherapy and radiation | Varies by subtype; includes chemotherapy, radiation, and immunotherapy |
It’s important to understand multiple myeloma and its related disorders. These conditions involve abnormal plasma cells in the bone marrow. This can lead to serious health problems.
Multiple myeloma is a blood cancer that affects plasma cells in the bone marrow. Plasma cells help fight infections by making antibodies. But in multiple myeloma, cancerous plasma cells take over, leaving less room for healthy cells.
Symptoms of multiple myeloma include bone pain, feeling tired, and getting sick often. It can also cause anemia, high calcium levels, and harm the kidneys.
A plasmacytoma is a single mass of cancerous plasma cells in the bone marrow or soft tissues. It can be in the bone (osseous plasmacytoma) or outside the bone (extraosseous or extramedullary plasmacytoma).
Treatment for plasmacytoma usually involves radiation therapy. Sometimes, surgery is needed. The outlook is better than for multiple myeloma, but there’s a chance it could turn into multiple myeloma.
Waldenstrom macroglobulinemia is a rare lymphoma. It’s caused by too many IgM antibodies, making blood thick and causing problems.
Symptoms include feeling weak, tired, and neurological issues. Treatment includes plasmapheresis to thin the blood, chemotherapy, and targeted therapy.
Amyloidosis is a group of diseases with amyloid fibrils in tissues. In plasma cell disorders, amyloidosis (AL amyloidosis) happens when plasma cells produce misfolded proteins. These proteins then deposit in organs.
Symptoms of AL amyloidosis vary based on the affected organs. They can include losing weight, feeling tired, and swelling. Treatment aims to reduce the abnormal proteins.
These conditions are complex and hard to manage. Our team is dedicated to giving full care and support to patients with multiple myeloma and related plasma cell disorders.
Understanding myeloproliferative neoplasms is key to diagnosing and treating these complex diseases. Myeloproliferative neoplasms (MPNs) are diseases where the body makes too many blood cells. This can cause serious health problems.
Polycythemia vera (PV) is a type of MPN. It causes too many red and white blood cells and platelets. This can lead to blood clots and heart problems. Key characteristics include:
Essential thrombocythemia (ET) is another MPN. It causes too many platelets, which can lead to blood clots. Clinical features may include:
Primary myelofibrosis (PMF) is a serious MPN. The bone marrow turns into fibrotic tissue. This leads to anemia, enlarged spleen, and other issues. Notable aspects include:
Chronic neutrophilic leukemia (CNL) is a rare MPN. It involves the constant growth of mature neutrophils in the blood and bone marrow. Diagnostic criteria include:
MPNs need careful diagnosis and management to improve patients’ lives. We will look deeper into these conditions and their treatments in the next sections.
Myelodysplastic syndromes (MDS) are a group of disorders where the bone marrow fails to make healthy blood cells. This can cause anemia, infections, and bleeding problems.
MDS is divided into several types based on the bone marrow and blood’s cell count, genetic changes, and other factors. The main types are:
The outlook for MDS varies based on several factors. These include the type of MDS, the patient’s age, and genetic mutations. Risk factors include exposure to chemicals, radiation, and previous chemotherapy. The International Prognostic Scoring System (IPSS) helps predict the prognosis.
Knowing the risk factors and prognosis is key to choosing the right treatment. Patients with higher-risk MDS might need more aggressive treatment. Those with lower-risk MDS might start with supportive care.
Treatment for MDS is customized based on the patient’s type, risk, and health. Options include:
Managing MDS needs a detailed approach, including regular checks and treatment adjustments. Medical research is constantly improving our understanding and treatment of this complex condition.
Rare haematological malignancies are a group of blood and bone marrow disorders. They are less common but have a big impact on health. We will look at rare conditions like histiocytic disorders, mastocytosis, dendritic cell neoplasms, and T-cell large granular lymphocytic leukemia.
Histiocytic disorders are diseases where histiocytes, part of the immune system, grow too much. These can be benign or malignant. Examples include Langerhans cell histiocytosis and Erdheim-Chester disease.
Mastocytosis is a disorder with too many mast cells in organs. It can show up in different ways, from skin to systemic.
Key Features of Mastocytosis:
Dendritic cell neoplasms are rare tumors from dendritic cells, important in the immune system. They are hard to diagnose because they are rare and can show up differently.
Diagnostic Challenges:
T-cell large granular lymphocytic leukemia (T-LGLL) is a rare chronic leukemia. It’s caused by large granular lymphocytes. It often leads to low blood counts and can be linked to autoimmune diseases.
Clinical Features:
In conclusion, rare haematological malignancies are tough to diagnose and treat. Knowing about these conditions is key to better patient care and improving treatment.
Knowing the symptoms of blood cancers is key to better patient care. Blood cancers, or haematological malignancies, show symptoms in many ways. Some symptoms are common, while others are specific to certain cancers.
General symptoms of blood cancers include:
Each type of blood cancer has its own symptoms:
If you’re feeling symptoms that won’t go away, see a hematologist. Early diagnosis is key to better treatment. Look for medical help if you notice:
Knowing the early signs can lead to quicker diagnosis and treatment. Look out for:
Spotting these symptoms early and getting medical help can greatly improve treatment for blood cancers.
Diagnosing blood cancers is a detailed process. It involves both clinical checks and advanced tests. These tests help find the right treatment for each patient.
Blood tests are the first step in finding blood cancers. They look for odd blood cell levels that might show cancer. Complete Blood Count (CBC) is a key test for this.
A CBC can spot issues like anemia or low blood cell counts. It can also find proteins on cancer cells.
A bone marrow biopsy is a key test for blood cancers. It takes a bone marrow sample for checking. The sample is then looked at for cancer cells and genetic changes.
This test helps find leukemia and multiple myeloma. It also shows how far the disease has spread, helping plan treatment.
CT scans, PET scans, and MRI are used to see how far cancer has spread. They spot big lymph nodes, tumors, or other issues.
These tests are key for knowing how to treat blood cancers. They show how the disease is growing and help plan treatment.
Genetic and molecular tests are very important for blood cancers. They look at cancer cell genes for specific changes.
Tests like fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) find genetic changes. This info helps tailor treatments to each patient.
| Diagnostic Test | Purpose | Information Provided |
| Blood Tests | Identify abnormal blood cell levels | Presence of anemia, leukopenia, or thrombocytopenia |
| Bone Marrow Biopsy | Examine bone marrow for cancer cells | Diagnosis of leukemia, multiple myeloma, and disease extent |
| Imaging Studies | Determine disease spread | Identification of enlarged lymph nodes, tumors, or abnormalities |
| Genetic and Molecular Testing | Analyze genetic material of cancer cells | Detection of specific mutations or abnormalities for targeted therapy |
Managing haematological cancers requires a detailed plan. This plan is made just for each patient. The treatment choice depends on the cancer type, stage, and the patient’s health.
Chemotherapy is key in fighting haematological malignancies. It uses drugs to kill or slow cancer cells. Patients can take these drugs by mouth or through an IV, often with other treatments.
Types of Chemotherapy:
Radiation therapy kills cancer cells with high-energy rays. It’s good for treating cancer that’s in one place or for easing symptoms like pain.
Types of Radiation Therapy:
Stem cell transplantation replaces bad stem cells with good ones. It’s a major treatment for many haematological cancers.
Types of Stem Cell Transplantation:
| Type | Description |
| Autologous | Uses the patient’s own stem cells. |
| Allogeneic | Uses stem cells from a donor. |
Targeted therapies aim at specific cancer cell molecules. They’re more precise, harming fewer normal cells.
“Targeted therapies have revolutionized the treatment of haematological malignancies, bringing new hope to patients with specific genetic mutations.”
Examples of Targeted Therapies:
These treatments show the complexity and variety in fighting haematological cancers. Knowing the options helps patients and doctors choose the best treatment.
It’s key to know about hematological malignancies for early detection and treatment of blood cancers. We’ve looked at different types like leukemias, lymphomas, myelomas, and myelodysplastic syndromes. Each has its own traits and treatment methods.
Early detection and treatment are very important. They greatly help patients. Spotting blood cancer symptoms early and getting medical help fast is critical. New ways to diagnose and treat, like chemotherapy and targeted therapies, have changed how we manage these diseases.
As we learn more about blood cancer, we can give better care to patients. We must keep researching and spreading awareness to fight hematologic malignancies. Together, we can improve care and give hope to those with these diseases.
Hematology is a branch of medicine. It focuses on blood and bone marrow disorders, including blood cancers.
Hematological malignancies, or blood cancers, affect the blood, bone marrow, or lymphatic system. They include leukemia, lymphoma, myeloma, and myelodysplastic syndromes.
Leukemia affects the blood and bone marrow. Lymphoma targets the lymphatic system. They have different treatments.
Symptoms include fatigue, weight loss, fever, and swollen lymph nodes. Bleeding or bruising easily is also common. Symptoms vary by cancer type.
Doctors use blood tests, bone marrow biopsies, and imaging studies to diagnose. Genetic testing helps determine the cancer type and stage.
Treatments include chemotherapy, radiation, stem cell transplantation, and targeted therapies. The choice depends on the cancer type, stage, and patient’s health.
Hematologists diagnose, treat, and manage blood disorders, including cancers. They provide essential care to patients with blood cancers.
Cure chances vary by cancer type and stage, and treatment response. Some cancers can be cured, while others need ongoing management.
Acute leukemia progresses quickly and needs immediate treatment. Chronic leukemia progresses slowly and may not require urgent treatment. The difference lies in cell type and disease speed.
Myelodysplastic syndrome (MDS) involves poorly formed or dysfunctional blood cells. It can lead to acute myeloid leukemia (AML) in some cases.
Risk factors include exposure to chemicals, radiation, and viruses. Genetic predisposition and family history also play a role.
Avoiding certain chemicals and radiation helps. A healthy lifestyle and regular check-ups can also reduce risk.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!