Last Updated on December 1, 2025 by Bilal Hasdemir

Patients getting brain radiation therapy might worry about seizures. Research shows many patients face seizures after radiotherapy for brain tumors. This is a big worry for those fighting cancer.
It’s important to know about seizures after brain radiation. We’ll look into why they happen, what they feel like, and how to treat them. This helps patients and their families deal with this side effect.
Key Takeaways
- Seizures are a possible complication of brain radiation therapy.
- Understanding the causes and symptoms is key for managing them.
- There are many ways to treat seizures after brain radiation.
- It’s vital for patients and caregivers to know the risks and benefits.
- Good medical care can greatly improve outcomes for those affected.
Understanding Brain Radiation Therapy
Brain radiation therapy is a key treatment for brain tumors and cancers. It uses high-energy particles or waves to kill or harm cancer cells. This stops them from growing and dividing.
We use different types of radiation therapy based on the tumor’s type and location, and the patient’s health. Our goal is to give the tumor the highest dose of radiation. We also try to protect the healthy brain tissue around it.
Types of Brain Radiation Treatments
There are several brain radiation treatments, each with its own benefits. These include:
- Whole Brain Radiation Therapy (WBRT): This treats the whole brain, often for patients with many brain metastases.
- Stereotactic Radiosurgery (SRS): A precise treatment that focuses a high dose of radiation on a small tumor.
- Fractionated Stereotactic Radiotherapy (FSRT): Similar to SRS but given in smaller doses over time. It’s used for larger tumors or those near important areas.
Common Indications for Brain Radiation
Brain radiation therapy is used for several conditions, including:
Condition | Description |
Brain Metastases | Cancer that has spread to the brain from other parts of the body. |
Primary Brain Tumors | Tumors that start in the brain, like glioblastoma or meningioma. |
Meningeal Disease | Cancer that has spread to the lining around the brain and spinal cord. |
It’s important for patients and their families to understand brain radiation therapy. This knowledge helps them make informed decisions about treatment. It also prepares them for possible side effects, like seizures.
The Prevalence of Seizures After Brain Radiation
It’s important to know how common seizures are after brain radiation. This knowledge helps doctors take better care of their patients. Seizures can really change a patient’s life, so it’s key to understand the risks.
Statistical Overview
Research shows that many patients get seizures after brain radiation. The exact number depends on the tumor type, how much radiation they get, and their health before treatment.These studies show that seizures are a big side effect of brain radiation. They affect a lot of patients.
Comparison to Other Neurological Side Effects
Seizures are not the only brain side effect from radiation. Other common ones include memory problems, headaches, and feeling very tired.
Looking at how common seizures are compared to other side effects helps us understand the risks better. For example, memory problems can happen in up to 50% of patients. Headaches and tiredness are also common.
Side Effect | Incidence Range |
Seizures | 20-30% |
Cognitive Changes | 40-50% |
Headaches | 30-40% |
Fatigue | 50-60% |
Knowing these numbers helps doctors prepare patients better. It also helps them find ways to lessen these side effects.
Mechanisms Behind Radiation-Induced Seizures
Radiation therapy can cause seizures by affecting the brain in different ways. It’s a key treatment for brain tumors but comes with side effects. These include seizures.
Acute Radiation Effects on Brain Tissue
Acute effects happen right after or during radiation therapy. They can cause inflammation and swelling in the brain. This can lead to seizures.
The inflammation comes from radiation damaging blood vessel cells. This disrupts the blood-brain barrier.
Acute effects can be managed with corticosteroids, which reduce inflammation and swelling. But, these medications have their own side effects and risks.
Delayed Radiation Effects Leading to Seizures
Delayed effects can happen months to years after radiation therapy ends. These effects are often permanent. They can include radiation necrosis, vascular changes, and demyelination.
Delayed Effect | Description | Potential Impact |
Radiation Necrosis | Death of brain tissue due to radiation | Seizures, cognitive decline |
Vascular Changes | Damage to blood vessels | Reduced blood flow, ischemia |
Demyelination | Damage to the myelin sheath surrounding nerve fibers | Disrupted nerve signal transmission |
These delayed effects can cause seizures by messing with brain function. The risk depends on the radiation dose, brain area affected, and how the patient reacts.
We’re learning more about reducing these risks with new radiation methods and care after treatment. Knowing how radiation causes seizures helps us find better ways to prevent and treat it.
Risk Factors for Developing Post-Radiation Seizures
It’s important to know the risk factors for seizures after brain radiation. This helps doctors manage and reduce this side effect.
Tumor Type and Location
The type and location of the tumor matter a lot. Tumors in areas like the temporal lobe are more likely to cause seizures. Tumors that are more aggressive also raise the risk.
Radiation Dosage and Schedule
The amount and timing of radiation therapy play big roles. Higher doses and larger doses per fraction can increase seizure risk. Finding the right dosage and schedule is key to treating the tumor without causing seizures.
Pre-existing Neurological Conditions
People with neurological conditions like epilepsy are more at risk. Conditions like brain metastases or previous injuries also raise the risk. Doctors need to consider these factors when planning treatment.
Knowing these risk factors helps doctors create better treatment plans. This can improve patient outcomes and quality of life.
Timing of Seizure Occurrence After Radiation
Radiation therapy can cause seizures at various times. These can happen during treatment or even years later. Knowing when seizures occur is key to caring for patients well.
Acute Seizures (During or Shortly After Treatment)
Acute seizures happen right after or during radiation therapy. They are linked to the brain’s immediate reaction to radiation. This reaction can cause swelling and inflammation, leading to seizures.
Key factors contributing to acute seizures include:
- Tumor location and size
- Radiation dosage and fractionation schedule
- Pre-existing neurological conditions
Delayed Seizures (Months to Years After Treatment)
Delayed seizures occur months or years after treatment. They are linked to long-term brain changes caused by radiation. These changes can damage the brain’s white matter, leading to seizures.
The risk factors for delayed seizures include:
- Higher total radiation dose
- Larger treatment volume
- Presence of necrosis or other late radiation effects
Knowing when seizures happen after radiation helps doctors plan better care. They can adjust monitoring and treatment to meet each patient’s needs.
Types of Seizures Associated with Brain Radiation
Seizures after brain radiation can take many forms. Each type has its own unique traits. Knowing these differences is key for the right diagnosis and treatment.
Focal Seizures
Focal seizures are common after brain radiation. They start in one part of the brain. The symptoms depend on where in the brain they start.
There are two types of focal seizures. One keeps the patient aware, while the other makes them less aware.
Focal seizures can show up in different ways. For example:
- Motor symptoms (e.g., twitching or stiffness)
- Sensory symptoms (e.g., unusual sensations or numbness)
- Autonomic symptoms (e.g., changes in heart rate or blood pressure)
- Psychic symptoms (e.g., feelings of déjà vu or fear)
Generalized Seizures
Generalized seizures affect both sides of the brain right away. They can make someone lose consciousness. These seizures have a big impact on the brain, causing more noticeable symptoms.
Generalized seizures from brain radiation can include:
- Tonic-clonic seizures (formerly known as grand mal seizures), which involve both muscle stiffening and convulsions
- Absence seizures, characterized by brief losses of consciousness
- Atonic seizures, which cause a sudden loss of muscle tone
- Tonic seizures, leading to muscle stiffening
- Clonic seizures, involving repetitive muscle contractions
Both focal and generalized seizures can greatly affect a person’s life. Getting the right diagnosis and treatment is critical to manage these seizures.
We will look into managing and understanding radiation-induced seizures further. This will give a full picture of this complex topic.
Diagnosing Radiation-Related Seizures
Diagnosing seizures linked to radiation therapy needs a detailed approach. We use advanced imaging and neurological checks. If a patient has seizures after brain radiation, we must figure out if it’s from the treatment or another problem like tumor growth.
Diagnostic Tests and Procedures
Several tests and procedures are key in finding out about radiation-related seizures. These include:
- Electroencephalogram (EEG): This test looks at brain electrical activity. It helps spot abnormal patterns that might show seizure activity.
- Magnetic Resonance Imaging (MRI): MRI scans give detailed brain images. They help us see any changes or damage from radiation.
- Computed Tomography (CT) scans: CT scans also help find structural problems or lesions that might cause seizures.
These tools are vital for figuring out why patients with brain radiation therapy have seizures.
Differentiating from Tumor Progression
It’s a big challenge to tell if seizures are from radiation or tumor growth. Tumors can also cause seizures, so it’s important to know the cause for the right treatment.
To tell the difference, we look at the patient’s history, clinical evaluation, and test results like MRI and CT scans. We might also use functional MRI or positron emission tomography (PET) scans to check brain changes.
By studying these diagnostic results, we can find out the seizure cause. Then, we can create a treatment plan that fits the patient’s needs.
Cancer Radiology Side Effects Beyond Seizures
Brain radiation therapy can cause more than just seizures. It can also affect patients’ thinking, physical comfort, and life quality. Knowing these side effects is key to giving the best care.
Cognitive Changes and Memory Issues
Brain radiation therapy often leads to thinking problems. Patients might struggle with memory, focus, and quick thinking. This is because the radiation affects healthy brain areas around the tumor.
Early help and special training can lessen these issues. This way, patients can do everyday tasks better and stay independent.
Headaches and Neurological Symptoms
Headaches are common in patients getting brain radiation. They can be mild or very bad. Other symptoms like dizziness or nausea might also happen.
The severity and how often these symptoms occur can depend on the radiation dose and where in the brain it’s applied. It’s important to manage these symptoms well to keep patients comfortable and happy.
Fatigue and Quality of Life Impact
Fatigue is a big problem for people getting radiation therapy. It affects their body, mind, and social life. Dealing with fatigue needs a plan that includes rest, exercise, and good food.
By tackling fatigue, doctors can greatly improve patients’ life quality. This lets them do more in their daily lives and feel more like themselves during treatment.
It’s vital to understand all the side effects of brain radiation therapy. This way, we can give care that focuses on the patient. By facing these challenges together, we can lessen their impact and support patients through their treatment.
Management of Post-Radiation Seizures
Managing seizures after brain radiation is complex. It requires a detailed approach to improve patient outcomes and quality of life. We will explore the strategies for managing these seizures, focusing on medications and surgery.
Anti-Epileptic Medications
Anti-epileptic drugs (AEDs) are the main treatment for seizures after brain radiation. The right AED depends on the seizure type, patient health, and drug interactions. Levetiracetam is often chosen because it has fewer side effects and interacts less with other drugs.
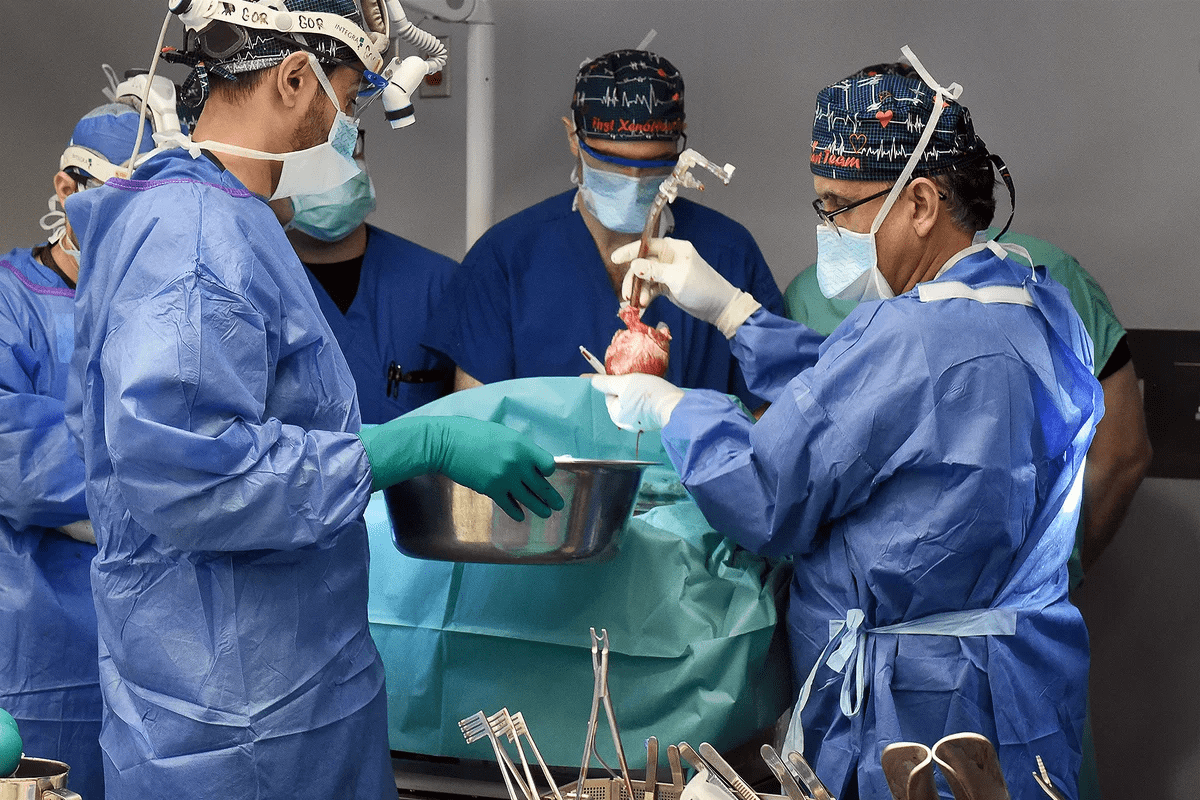
Surgical Interventions
In some cases, surgery is needed to manage seizures after brain radiation. This can include removing the seizure focus or using devices like vagus nerve stimulators. The decision to have surgery depends on how severe the seizures are, how well AEDs work, and where the seizure focus is. Surgical interventions can greatly improve seizure control for the right patients.
Treatment | Seizure Control Rate | Common Side Effects |
Levetiracetam | 70% | Fatigue, Irritability |
Valproate | 65% | Tremors, Weight Gain |
Surgical Intervention | 80% | Surgical Risks, Infection |
Healthcare providers use a mix of medications and surgery to manage post-radiation seizures. The best treatment depends on the patient’s specific needs. A detailed care plan is key for the best results.
Prophylactic Approaches to Prevent Seizures
Prophylactic strategies are key in lowering the risk of seizures after brain radiation therapy. By using preventive measures, doctors can greatly reduce seizure chances. This improves patient outcomes and quality of life.
Preventive Medications
Preventive medications are a mainstay in managing seizures after brain radiation. Anti-epileptic drugs (AEDs) are given to patients at high risk of seizures. The right AED depends on the patient’s history, tumor type, and radiation dose.
“The use of AEDs has been shown to lower seizure rates in brain radiation patients,” studies say. Starting AED therapy early is key to prevent seizures and long-term seizure disorders.
Radiation Planning Strategies
Along with meds, radiation planning is critical in lowering seizure risk. Advanced radiation techniques like stereotactic radiosurgery and intensity-modulated radiation therapy target tumors precisely. This spares brain tissue, reducing seizure risk.
Good radiation planning looks at the tumor’s location, size, and how close it is to brain structures. This way, doctors can avoid sensitive areas, lowering the chance of seizures and other brain side effects.
As
“Radiation oncology has evolved significantly, with modern techniques improving precision and reducing side effects.”
This progress highlights the need to include radiation planning in managing brain radiation therapy patients.
Comparing Whole Brain vs. Targeted Radiation Side Effects
Choosing between whole brain radiation and targeted radiation therapy affects treatment results and side effects. It’s important to know the differences, like how they impact seizure risk.
Whole brain radiation treats the whole brain. It’s used when cancer might spread to the brain or when there are many brain tumors. Targeted radiation, on the other hand, focuses on specific areas or tumors. It tries to avoid harming healthy brain tissue.
Whole Brain Radiation Seizure Risk
Whole brain radiation therapy (WBRT) can cause side effects like memory loss and tiredness. Seizures are a worry, mainly for those with brain problems or certain brain tumors.
Radiation Approach | Seizure Risk Factors | Common Side Effects |
Whole Brain Radiation | Pre-existing neurological conditions, tumor type and location | Cognitive decline, fatigue, hair loss |
Targeted Radiation | Radiation dose, tumor size and location | Localized tissue damage, radiation necrosis |
Targeted Radiation Approaches
Targeted radiation, like stereotactic radiosurgery (SRS) and intensity-modulated radiation therapy (IMRT), is more precise. It might lower the chance of seizures and other side effects compared to whole brain radiation. These methods give higher doses to specific spots, protecting more of the brain.
Looking at the whole brain and targeted radiation helps us understand their risks and benefits. This knowledge helps make better treatment choices. It balances how well the treatment works with the chance of side effects like seizures.
Long-term Monitoring After Brain Radiation
Monitoring patients after brain radiation is key to managing late effects. As cancer treatment advances, the need for long-term care after brain radiation therapy grows. This care is vital for patient well-being.
Follow-up Protocols
Effective follow-up plans are critical for catching complications early. We suggest a structured schedule for check-ups and tests. The plan’s details depend on the patient’s condition and treatment.
A typical follow-up might include:
- Regular neurological exams
- Imaging tests (like MRI, CT scans)
- Checks on cognitive function
- Surveys from patients
Follow-up Component | Frequency | Purpose |
Neurological Examination | Every 3-6 months | Check neurological health and spot issues |
Imaging Studies | Every 6-12 months | Watch for tumor return or radiation side effects |
Cognitive Function Assessment | Annually | Track cognitive changes and offer support |
Warning Signs Requiring Medical Attention
Patients and caregivers must know the warning signs for urgent medical help. These include:
- Seizures or convulsions
- Big changes in cognitive function or memory
- Worsening headaches or neurological symptoms
- Changes in vision or speech
Spotting these signs early can greatly help treatment. We stress the need to teach patients and their families about these symptoms.
Following a strict follow-up plan and watching for warning signs can boost patient outcomes. Our dedication to care goes beyond the initial treatment. We ensure patients get the ongoing support they need for their long-term health.
Radiation Necrosis and Its Relationship to Seizures
It’s key to understand how radiation necrosis and seizures are connected. This is important for dealing with side effects from brain radiation therapy. Radiation necrosis happens when brain tissue dies because of radiation damage.
Identifying Radiation Necrosis
Finding radiation necrosis can be hard. Its signs can look like other problems, like tumor growth. Symptoms include headaches, confusion, and seizures. MRI and PET scans are vital for telling radiation necrosis apart from other issues.
- MRI: Shows the damaged area and how big it is.
- PET Scan: Helps tell radiation necrosis from tumor growth by looking at metabolic activity.
Treatment Approaches for Necrosis-Related Seizures
Dealing with seizures caused by radiation necrosis needs a few steps. This includes medicines for seizures and sometimes surgery.
- Anti-Epileptic Medications: The first step to control seizures and how often they happen.
- Surgical Intervention: Considered for those with seizures that don’t get better or have a big problem from necrosis.
It’s vital to have a treatment plan that fits each person. Everyone reacts differently to radiation necrosis and seizures.
Advances in Brain Radiation Techniques to Reduce Side Effects
New brain radiation techniques are changing how we treat brain tumors and other conditions. These new methods help reduce side effects and improve patient results. In recent years, radiation therapy has become more precise and effective.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is a precise radiation therapy. It focuses a high dose of radiation on a specific brain area. This method is great for treating small, well-defined tumors.
SRS is effective for various brain conditions, including some cancers and vascular malformations.
Key benefits of SRS include:
- High precision in targeting tumors
- Minimal damage to surrounding healthy tissue
- Short treatment duration, often completed in a single session
Proton Therapy
Proton therapy uses protons instead of X-rays to kill cancer cells. This method is beneficial because protons can stop at a specific depth. This reduces damage to tissues beyond the tumor.
“Proton therapy represents a significant advancement in radiation oncology, improving outcomes and reducing side effects for brain tumor patients.”
Expert in Radiation Oncology
Advantages of proton therapy:
Treatment Aspect | Proton Therapy | Traditional Radiation |
Precision | High, with minimal damage beyond the tumor | Variable, with possible damage to surrounding tissues |
Side Effects | Generally fewer due to precise targeting | Can be more significant due to broader radiation exposure |
Targeted Radiation Approaches
Targeted radiation methods, like intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), also show promise. These techniques allow for real-time adjustments during treatment. This ensures accurate delivery of radiation to the tumor site.
IMRT and IGRT enable:
- Real-time monitoring and adjustment of radiation beams
- Enhanced precision in targeting tumors
- Reduced exposure to surrounding healthy tissues
In conclusion, new brain radiation techniques like SRS, proton therapy, and targeted radiation approaches are greatly improving treatment for brain tumor patients. These innovations not only make treatments more effective but also play a key role in reducing side effects. This improves patient quality of life.
Patient Experiences and Quality of Life Considerations
Going through brain radiation therapy is complex. It’s not just about the treatment but also dealing with its effects. Managing side effects like seizures is key to improving patients’ lives.
Coping with Seizures After Radiation
Dealing with seizures after brain radiation can be tough. Seizures can be unpredictable and affect daily life. A patient advocate says, “Living with the uncertainty of when a seizure might occur can be incredibly daunting.”
It’s important for patients to have a strong support system. This can make a big difference.
To manage seizures well, patients can:
- Stick to their anti-epileptic medications
- Keep a seizure diary to track when seizures happen and what might trigger them
- Avoid things that might cause seizures, like certain foods or too much stress
By being proactive, patients can manage their condition better and live a better life.
Support Resources for Patients
Support resources are key for patients dealing with brain radiation therapy and seizures. These can include:
- Support groups, online or in-person, where patients can share and get advice
- Counseling to help with the emotional side of seizures and treatment
- Workshops and materials on managing seizures and improving life quality
One patient said, “Having these resources has changed my life. It’s great to know I’m not alone and that others understand what I’m going through.”
Using these resources can help patients deal with seizures and other challenges. This can greatly improve their quality of life.
Conclusion: Balancing Treatment Benefits and Side Effect Risks
Brain radiation therapy is key for treating many brain conditions, like cancer. But, it can lead to side effects, like seizures. It’s important to know both the good and the bad sides.
Choosing to have brain radiation therapy means weighing its benefits against the chance of side effects. Knowing how seizures can happen from radiation helps everyone make better choices.
There are ways to lessen the chance of seizures. Using special medicines and planning radiation carefully can help. New methods like stereotactic radiosurgery and proton therapy also show promise.
In the end, finding the right balance between treatment benefits and risks is complex. It requires understanding how radiation therapy works with each patient. By considering all these factors, patients and doctors can aim for the best results and lower the risk of seizures.
FAQ
What are the common side effects of brain radiation therapy?
Side effects include fatigue, headaches, and changes in thinking. Hair loss is also common. Some may get seizures, which is a big worry for those who already have seizure disorders.
How does brain radiation therapy cause seizures?
Radiation can damage brain tissue, leading to inflammation and scarring. This damage can disrupt brain activity, causing seizures.
Are seizures a common side effect of whole brain radiation therapy?
Seizures can happen after whole brain radiation therapy. How often depends on the radiation dose, the type of tumor, and any pre-existing conditions.
Can targeted radiation approaches reduce the risk of seizures?
Yes, methods like stereotactic radiosurgery and proton therapy can lower seizure risk. They do this by focusing the radiation on the tumor, sparing healthy brain tissue.
How are radiation-related seizures diagnosed?
Doctors use clinical evaluation, imaging studies, and EEG to diagnose seizures caused by radiation. These tools help assess brain activity.
What is the difference between acute and delayed seizures after radiation therapy?
Acute seizures happen during or right after treatment. Delayed seizures occur months or years later. Both need medical care and proper management.
Can anti-epileptic medications prevent seizures after brain radiation?
Sometimes, doctors may give anti-epileptic medications to prevent seizures in high-risk patients. This choice is made on an individual basis.
How can patients cope with seizures after radiation therapy?
Patients can manage seizures by following their medication schedule and keeping a seizure diary. They should also get support from healthcare providers, family, and support groups.
What are the warning signs that require medical attention after brain radiation?
Warning signs include new or worsening seizures, severe headaches, confusion, or other neurological symptoms. If you experience these, seek medical help right away.
Can radiation necrosis cause seizures?
Yes, radiation necrosis, a complication of radiation therapy, can lead to seizures. Managing it often involves medical and surgical treatments.
Are there any advances in brain radiation techniques that reduce side effects?
Yes, new techniques like stereotactic radiosurgery, proton therapy, and targeted radiation aim to reduce side effects. They deliver precise radiation doses to tumors while protecting healthy tissue.
References
National Center for Biotechnology Information. Postradiotherapy Seizures in Brain Tumor Patients Prevalence. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5654353/