Last Updated on November 27, 2025 by Bilal Hasdemir
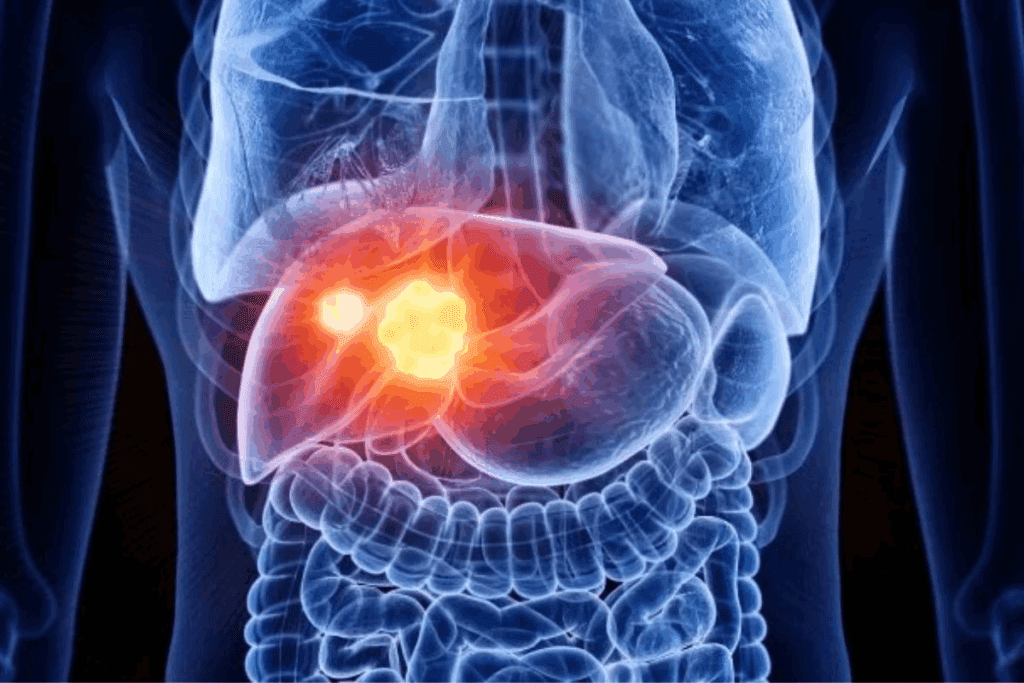
A cancerous liver tumor is a serious issue that needs quick action. The liver is key for many important functions. A liver neoplasm can harm a patient’s health a lot.
We aim to teach you about liver cancer in simple terms. Liver cancer, also known as liver cancer, starts in the liver. Knowing the different types is key for the right treatment.
Key Takeaways
- Liver cancer is a serious condition that requires prompt medical attention.
- There are different types of liver cancer, each with distinct characteristics.
- Understanding the basics of liver cancer is important for effective treatment.
- A cancerous tumor in the liver can significantly impact a patient’s health.
- Liver cancer treatment options vary depending on the type and stage of the disease.
Understanding Liver Cancer Terminology

It’s important for patients and doctors to know the terms related to liver cancer. Liver cancer, also known as hepatic carcinoma, includes different types that harm the liver. The liver is key for many body functions.
Medical Names for Liver Cancer
Liver cancer has several names based on its type and where it starts. The most common is hepatocellular carcinoma (HCC), which comes from liver cells. Other types are cholangiocarcinoma, affecting bile ducts, and angiosarcoma, a rare one from blood vessels in the liver. Knowing these names helps in getting the right treatment.
Incidence and Impact in the United States
Liver cancer is a big problem in the U.S., with many types found. It’s among the top causes of cancer deaths. The number of cases is going up, mainly because of infections like hepatitis B and C, cirrhosis, and lifestyle issues like drinking too much and being overweight.
We know liver cancer, or malignant liver tumor, is a tough condition needing full care. By understanding the terms and how common it is, we can tackle its challenges better. This helps improve how we treat and care for patients.
Cancerous Liver Tumor: Types and Classifications

Cancerous liver tumors are divided into primary and secondary types. Each type has its own treatment and prognosis. Knowing these classifications helps in making effective treatment plans.
Primary Liver Cancers
Primary liver cancers start in the liver itself. The most common is hepatocellular carcinoma (HCC), which comes from liver cells. Other types include cholangiocarcinoma from bile duct cells and rare ones like angiosarcoma and hepatoblastoma.
These cancers are linked to risk factors like hepatitis B or C, cirrhosis, and toxin exposure. The rate of primary liver cancer varies worldwide, with higher rates in areas with more hepatitis B.
Secondary (Metastatic) Liver Cancers
Secondary liver cancers start from cancer cells that spread to the liver from other places. These cancers are more common and often come from cancers in the colon, breast, lung, and pancreas.
Metastatic liver cancers affect treatment and prognosis. Primary liver cancers are treated based on their characteristics. But metastatic liver cancers are treated based on where the cancer first started and how far it has spread.
| Type of Liver Cancer | Origin | Common Primary Sites |
| Primary Liver Cancer | Liver cells or bile duct cells | N/A |
| Secondary (Metastatic) Liver Cancer | Cancer cells from other parts of the body | Colon, Breast, Lung, Pancreas |
It’s important to know the difference between primary and secondary liver cancers. Primary liver cancers focus on treating the liver. But metastatic liver cancers need a treatment plan that looks at the primary cancer site.
Hepatocellular Carcinoma (HCC)
Hepatocellular carcinoma (HCC) is a common liver cancer. It often starts in people with liver disease. Knowing about HCC is key for doctors and patients.
Characteristics and Development
HCC starts in the liver’s main cells, called hepatocytes. It grows due to genetic changes, chronic inflammation, and cirrhosis. Chronic liver diseases, like hepatitis B and C, are big risk factors for HCC.
The growth of HCC is a long process. It starts with liver damage, then cirrhosis, and ends in cancer. Factors like viral hepatitis, alcohol, and NASH can speed this up.
High-Risk Populations
Some groups are more likely to get HCC. These include those with chronic hepatitis B or C, cirrhosis, and genetic disorders like hemochromatosis. Drinking a lot of alcohol and being obese also raise the risk.
Knowing who’s at risk helps catch HCC early. We suggest regular checks for those at high risk. This can lead to better treatment and outcomes.
Cholangiocarcinoma: Cancer of the Bile Ducts
Cholangiocarcinoma is a rare cancer that starts in the bile ducts. These ducts are key for digestion. We’ll look at the types of cholangiocarcinoma and the challenges in diagnosing it.
Intrahepatic vs. Extrahepatic Types
There are two main types of cholangiocarcinoma: intrahepatic and extrahepatic. Intrahepatic cholangiocarcinoma happens inside the liver. Extrahepatic cholangiocarcinoma occurs outside the liver, affecting the ducts leading to the gallbladder and small intestine.
- Intrahepatic cholangiocarcinoma is linked to chronic liver disease and cirrhosis.
- Extrahepatic cholangiocarcinoma is more common and includes perihilar and distal subtypes.
Unique Diagnostic Challenges
Diagnosing cholangiocarcinoma is hard because its symptoms are not clear and the bile ducts are complex. We use CT scans, MRI, and ERCP to see the ducts and get tissue for biopsy.
- Blood tests for liver function and tumor markers.
- Imaging to see the bile ducts and how big the tumor is.
- Endoscopic procedures to get tissue for lab tests.
Early detection and accurate diagnosis are key for effective treatment. We’re working to better understand this complex cancer to help patients.
Rare Forms of Primary Liver Cancer
Hepatocellular carcinoma is the most common liver cancer. But, there are rare types like angiosarcoma, hemangiosarcoma, hepatoblastoma, and fibrolamellar carcinoma. Each one needs a special way to be diagnosed and treated. Knowing about these cancers helps doctors give the best care to patients.
Angiosarcoma and Hemangiosarcoma
Angiosarcoma and hemangiosarcoma are rare and aggressive cancers. They start in the liver’s blood vessels. These tumors grow fast and are hard to treat. Symptoms can be hard to spot early.
Treatment usually includes surgery, chemotherapy, and radiation. This combo aims to fight cancer.
Hepatoblastoma in Children
Hepatoblastoma is a rare liver cancer in kids, often in the first year. It’s a tumor from immature liver cells. When treated early and well, it has a good chance of recovery.
Doctors usually use surgery and chemotherapy together. This helps the child fight cancer.
Fibrolamellar Carcinoma
Fibrolamellar carcinoma is a rare type of liver cancer. It happens in younger people without liver disease. It has special features and usually shows up as a big tumor.
Surgery is often the main treatment. If the tumor can be removed, the outlook is better.
| Cancer Type | Demographics | Characteristics | Treatment Approaches |
| Angiosarcoma/Hemangiosarcoma | Typically adults | Aggressive, vascular origin | Surgery, chemotherapy, radiation |
| Hepatoblastoma | Primarily children | Malignant, immature liver cells | Surgery, chemotherapy |
| Fibrolamellar Carcinoma | Younger individuals | Distinct histology, large solitary tumor | Surgical resection |
Experts say, “Rare forms of primary liver cancer, such as angiosarcoma and hepatoblastoma, need special treatments.” This shows how vital it is to know and handle these cancers right.
Metastatic Liver Tumors
When cancer spreads to the liver from other parts of the body, it’s called metastatic liver cancer. This shows the cancer has moved from its first place to the liver. The liver is a common place for cancer to spread because of its blood supply.
Common Primary Cancer Sites
Metastatic liver tumors usually start from cancers in other parts of the body. The most common places include:
- Colon and Rectum: Colorectal cancer often goes to the liver.
- Breast: Breast cancer can also spread to the liver, mainly in later stages.
- Lungs: Lung cancer is another common source of liver metastasis.
- Pancreas: Pancreatic cancer can spread to the liver because of its close location.
These cancers can move through the bloodstream or lymphatic system. The liver is a main target because of its blood flow.
Clinical Differences from Primary Liver Cancer
Metastatic liver cancer is different from primary liver cancer in many ways. Primary liver cancer starts in the liver, while metastatic liver cancer comes from somewhere else.
The symptoms can vary, but common ones are:
- Abdominal pain or discomfort
- Weight loss
- Loss of appetite
- Fatigue
Treatment for metastatic liver cancer usually aims to manage symptoms and treat the main cancer site. This might include chemotherapy or targeted therapy.
Risk Factors for Liver Cancer Development
Knowing the risk factors for liver cancer is key to preventing and catching it early. Liver cancer is shaped by genetics, environment, and lifestyle.
Viral Hepatitis (B and C)
Viral hepatitis, like hepatitis B and C, is a big player in liver cancer. Long-term infection can cause cirrhosis and damage the liver. This raises the chance of getting hepatocellular carcinoma (HCC), the main liver cancer type.
People with chronic hepatitis B or C face a higher risk of liver cancer. This is because their liver keeps getting inflamed and trying to heal.
Cirrhosis and Chronic Liver Diseases
Cirrhosis, or scarring of the liver, is a big risk factor for liver cancer. It can come from things like too much alcohol, viral hepatitis, or NASH.
Having cirrhosis means your liver disease is advanced. So, it’s very important to watch for liver cancer signs early.
Lifestyle and Environmental Factors
Lifestyle and environment also play a part in liver cancer risk. Drinking too much alcohol is a known risk. It can cause cirrhosis and up the liver cancer risk.
Some environmental toxins, like aflatoxins from mold on grains and nuts, also raise liver cancer risk. Aflatoxin exposure is a big worry in areas with bad food storage.
Other lifestyle choices, like being overweight or having diabetes, also up liver cancer risk. They do this by leading to NAFLD and NASH.
Signs and Symptoms of Liver Malignancies
It’s vital to spot the warning signs of liver cancer early. This is because liver cancer often shows symptoms that are not clear. This makes it hard to catch it early.
Early Warning Signs
In the beginning, liver cancer might not show obvious signs. You might feel fatigue or loss of appetite. Some people might lose weight without trying or notice swelling in the upper right belly.
Other signs include skin color changes, like jaundice. This is when your skin and eyes turn yellow. It happens when your liver can’t handle bilirubin, a yellow substance in your body.
Advanced Disease Manifestations
When liver cancer gets worse, symptoms get more serious. You might feel severe abdominal pain in the upper right. You could also vomit blood or have black, tarry stools.
Advanced liver cancer can also cause fluid buildup in the abdomen, known as ascites. This can make you uncomfortable and make it hard to breathe. In some cases, liver cancer can affect your brain, causing cognitive changes. This is because toxins build up in your blood, a condition called hepatic encephalopathy.
It’s important to know these signs and get medical help. Early treatment can greatly improve your chances of managing liver cancer.
Diagnostic Approaches for Liver Cancer
Accurate diagnosis is key in managing liver cancer. It uses blood tests, imaging, and biopsies. Each method is important for finding and understanding the disease.
Blood Tests and Biomarkers
Blood tests are often the first step. They look for biomarkers like alpha-fetoprotein (AFP). These tests are not always right but help when used with other methods.
Key biomarkers include AFP, important for HCC. But, not all liver cancers have high AFP levels. So, other tests are needed too.
Imaging Techniques
Imaging is vital for seeing the liver’s details. Ultrasound, CT scans, and MRI are used. They help spot tumors and see if cancer has spread.
Each method has its benefits. Ultrasound is easy and common. CT scans give detailed views. MRI is great for finding liver lesions and telling them apart.
Biopsy Procedures
Biopsy is the best way to confirm liver cancer. It takes a liver tissue sample for testing. It can tell if it’s cancer, what type, and more about the tumor.
There are many biopsy types, like fine-needle and core needle biopsies. The choice depends on the tumor’s spot and the patient’s health.
In summary, diagnosing liver cancer needs blood tests, imaging, and biopsies. Using all these tools helps doctors find and treat liver cancer well.
Staging Systems for Liver Cancer
Staging liver cancer is key for treatment plans and predicting outcomes. It shows how far the disease has spread. This is important for choosing the right treatment.
TNM Classification
The TNM classification is a common staging system for liver cancer. It looks at three main factors: the tumor size (T), nearby lymph nodes (N), and if the cancer has spread (M). This helps doctors classify liver cancer into different stages.
| TNM Stage | Description |
| Stage I | Single tumor without vascular invasion or extrahepatic spread |
| Stage II | Single tumor with vascular invasion or multiple tumors ≤ 5 cm |
| Stage III | Multiple tumors > 5 cm or tumor involving a major branch of the portal or hepatic veins |
| Stage IV | Tumor with distant metastasis |
A leading oncologist says, “The TNM staging system is key for understanding liver cancer. It helps make informed treatment choices.”
“The TNM staging system provides a standardized framework for assessing the extent of liver cancer, which is essential for making informed treatment decisions.”
Barcelona Clinic Liver Cancer (BCLC) Staging
The Barcelona Clinic Liver Cancer (BCLC) system also classifies liver cancer. It looks at tumor characteristics, liver function, and patient performance. The BCLC system helps decide treatment based on the stage of the disease.
The BCLC system is useful because it links staging to treatment options. This helps doctors tailor treatments to each patient’s needs.
Understanding liver cancer staging is important. It shows the disease’s complexity and the need for personalized treatment. Both TNM and BCLC systems are key in guiding treatment and predicting outcomes.
Surgical Treatments for Liver Cancer
For many liver cancer patients, surgery offers a chance for a cure. Surgery is considered when the cancer is in one place and the patient is healthy enough for it.
Partial Hepatectomy
Partial hepatectomy, or liver resection, removes the part of the liver with the tumor. It’s used when the cancer is in one area and the rest of the liver can work well.
Key considerations for partial hepatectomy include:
- Liver function: The remaining liver tissue must be able to perform the necessary liver functions.
- Tumor location: The tumor must be located in a way that allows for safe removal.
- Patient’s overall health: The patient must be in good enough health to undergo major surgery.
Liver Transplantation
Liver transplantation replaces the patient’s liver with a healthy one. It’s for patients with early-stage liver cancer and liver disease.
Benefits of liver transplantation include:
- Removal of the cancerous liver
- Treatment of underlying liver disease
- Potential for cure
Ablative Techniques
Ablative techniques destroy cancer cells without removing them. They’re for patients who can’t have surgery or have small tumors.
Types of ablative techniques include:
- Radiofrequency ablation (RFA)
- Microwave ablation (MWA)
- Cryotherapy
These treatments give liver cancer patients options. The right treatment depends on the cancer’s stage, the patient’s health, and liver function.
Non-Surgical Interventional Therapies
Medical technology has improved a lot. Now, we have non-surgical treatments for liver cancer. These options are great for people who can’t have surgery or need more help to manage their disease.
Transarterial Chemoembolization (TACE)
TACE is a way to treat liver tumors. It sends chemotherapy directly to the tumor through the blood. At the same time, it blocks the tumor’s blood supply. This method helps shrink the tumor.
The benefits of TACE are:
- Targeted treatment: Chemotherapy goes straight to the tumor, reducing side effects.
- Reduced tumor size: By cutting off blood supply, TACE can make tumors smaller and easier to handle.
- Improved outcomes: TACE can be used alone or with other treatments, leading to better results for patients.
Radioembolization (Y-90)
Radioembolization, or Y-90, is another non-surgical treatment. It involves injecting tiny radioactive beads into the arteries that feed the liver tumor. These beads kill cancer cells from the inside.
Key benefits of radioembolization are:
- Minimally invasive: The procedure uses a small catheter, making recovery quick.
- Effective for inoperable tumors: Radioembolization treats tumors that can’t be removed by surgery.
- Combination therapy: It can be paired with other treatments like chemotherapy or targeted therapy.
TACE and radioembolization are important treatments for liver cancer. They offer hope for better outcomes and a better quality of life for patients.
Systemic Treatments for Advanced Liver Cancer
For those with advanced liver cancer, systemic treatments offer hope. These treatments aim at cancer cells all over the body. They provide a full care approach.
Targeted Molecular Therapies
Targeted molecular therapies are a big step forward in treating advanced liver cancer. They focus on specific molecules that help cancer grow and spread. This way, they harm fewer healthy cells, leading to fewer side effects.
Benefits: These therapies are more effective and have fewer side effects than traditional chemotherapy.
Limitations: Their success depends on the presence of certain molecular targets. Not all patients qualify for these treatments.
Immunotherapy Approaches
Immunotherapy is another hopeful treatment for advanced liver cancer. It boosts the body’s immune system. This lets it fight cancer cells better.
- Checkpoint inhibitors: These therapies let the immune system attack cancer cells more strongly.
- Cancer vaccines: These vaccines help the immune system recognize and fight cancer cells.
Immunotherapy can lead to long-lasting results for some patients. But, its success varies, and it can have side effects.
Conventional Chemotherapy
Even though newer treatments exist, conventional chemotherapy is an option for advanced liver cancer. It’s used when other treatments aren’t possible.
Chemotherapy can make tumors smaller, slow disease growth, and ease symptoms. This improves patients’ quality of life.
But, chemotherapy can harm healthy cells too. This leads to various side effects.
Knowing about these treatments helps patients with advanced liver cancer make better choices. They can do this with the help of their healthcare providers.
Prognosis and Survival Statistics
The outlook for liver cancer patients changes a lot based on when they find out they have it. Knowing these details helps both patients and doctors make better choices about treatment.
Factors Influencing Outcomes
Many things affect how well someone with liver cancer will do. These include:
- The stage of cancer at diagnosis
- The health of the liver
- Other health issues, like cirrhosis or hepatitis
- How well the chosen treatment works
Early-stage liver cancer has a better chance of recovery than later stages. The liver’s health is very important. It affects how well the body can handle treatments.
Five-Year Survival Rates by Stage
Survival rates for liver cancer depend a lot on when it’s found. In the U.S., about 20% of people with liver cancer live for five years. But, this number can be much higher or lower.
For example, if the cancer is found early, the survival rate can be over 30%. But, if it has spread far, it’s less than 3%.
| Stage | 5-Year Survival Rate |
| Localized | 33% |
| Regional | 11% |
| Distant | 3% |
Early detection and treatment are key to better survival chances. New treatments and ways to help patients are making a big difference.
Prevention of Liver Cancer
To lower liver cancer rates, we need to focus on prevention. This includes getting vaccinated against hepatitis and making lifestyle changes. By doing these things, we can greatly cut down the risk of getting liver cancer.
Vaccination Against Hepatitis
Hepatitis B vaccination is key in preventing liver cancer. The virus is a big risk factor for liver cancer. Vaccination has been proven to lower liver cancer rates in high-risk groups.
We suggest that people at high risk, like those with a family history of liver cancer and healthcare workers, get vaccinated. The vaccine is given in a series of shots over six months. It’s important to finish the whole series for the best protection.
Lifestyle Modifications
Living a healthier lifestyle is also important in preventing liver cancer. This means avoiding alcohol, keeping a healthy weight, and being careful about aflatoxin exposure. Aflatoxins are harmful toxins found in some foods, mainly in areas with bad food storage.
By changing our lifestyle, we can lower our risk of liver cancer. Also, knowing about job-related dangers and taking safety steps can help even more.
Screening for High-Risk Individuals
It’s important for people at high risk to get regular liver cancer screenings. This includes those with chronic hepatitis B or C, cirrhosis, and other liver diseases. Tests like ultrasound and alpha-fetoprotein (AFP) blood tests can find liver cancer early, when it’s easier to treat.
We advise high-risk individuals to talk to their doctors about a screening plan. This plan should be made just for them.
| Prevention Strategy | Description | Benefit |
| Hepatitis B Vaccination | Vaccination against hepatitis B virus | Reduces liver cancer risk by preventing hepatitis B infection |
| Lifestyle Modifications | Avoiding alcohol, maintaining a healthy weight, avoiding aflatoxins | Reduces risk factors associated with liver cancer |
| Regular Screening | Ultrasound and AFP blood tests for high-risk individuals | Enables early detection and treatment of liver cancer |
Conclusion
Understanding liver cancer is key to managing it well. It includes types like hepatocellular carcinoma and cholangiocarcinoma. A cancerous liver tumor is a serious health issue, making early detection very important.
We’ve looked at the different liver cancer types, risk factors, and how to diagnose and treat it. Prevention is also critical, with steps like getting vaccinated against hepatitis and making healthy lifestyle choices.
Managing liver cancer involves preventing it, finding it early, and treating it right. Knowing the risks and symptoms helps people get medical help fast. This can lead to better health outcomes. As we learn more about cancer, there’s hope for better survival rates and quality of life for those affected.
FAQ
What is a cancerous liver tumor?
A cancerous liver tumor is an abnormal growth in the liver. It can start in the liver or spread from another part of the body.
What are the different types of liver cancer?
Liver cancer types include hepatocellular carcinoma (HCC), cholangiocarcinoma (bile duct cancer), and metastatic liver cancer. Angiosarcoma, hemangiosarcoma, hepatoblastoma, and fibrolamellar carcinoma are rare forms.
What are the risk factors for developing liver cancer?
Risk factors include viral hepatitis (B and C), cirrhosis, and chronic liver diseases. Lifestyle factors like heavy alcohol use and aflatoxin exposure also play a role. Certain genetic conditions increase risk.
What are the symptoms of liver cancer?
Symptoms include abdominal pain, weight loss, and fatigue. Loss of appetite, jaundice, and swelling in the abdomen are also signs. Early stages may not show symptoms, making screening important.
How is liver cancer diagnosed?
Diagnosis involves blood tests and imaging like ultrasound, CT, and MRI scans. A biopsy confirms the presence and type of liver cancer.
What are the treatment options for liver cancer?
Treatments include surgical resection, liver transplantation, and ablative techniques. Transarterial chemoembolization (TACE), radioembolization, and targeted therapies are also options. Immunotherapy and chemotherapy are used based on the cancer’s stage and type.
What is the prognosis for liver cancer patients?
Prognosis depends on the cancer’s stage, liver function, and overall health. Early-stage cancer has a better outlook. Advanced stages have poorer outcomes. Five-year survival rates vary by stage.
Can liver cancer be prevented?
Prevention includes hepatitis B vaccination and lifestyle changes. Reducing alcohol use and avoiding aflatoxins helps. Screening high-risk individuals for early detection is also key.
What is the role of staging in liver cancer management?
Staging systems like TNM and Barcelona Clinic Liver Cancer (BCLC) help determine disease extent. They guide treatment and predict outcomes.
How does liver cancer impact patients and their families?
Liver cancer diagnosis and treatment affect patients and families physically, emotionally, and financially. It highlights the need for support services.
References
New England Journal of Medicine. Liver Cancer Terminology and Etiology. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMra1001683
The Lancet. Liver Cancer Terminology Types and Impact. Retrieved from https://www.thelancet.com/journals/langas/article/PIIS2468-1253(21)00224-8/fulltext
National Center for Biotechnology Information. Liver Cancer Nomenclature Types and Importance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8796122/