Last Updated on November 13, 2025 by
Low platelet counts, or thrombocytopenia, are a big worry for cancer patients. They can affect how well patients do and how they are treated. We will look at the cancers that can cause this problem, focusing on blood cancers and solid tumors. What cancers causing thrombocytopenia are linked to low platelets? Discover which terrible diseases commonly affect platelet production.
It’s important to know what thrombocytopenia is and why it happens. Places like LIV Hospital are leading the way in new and honest healthcare. They offer full support to patients from around the world.
Looking into how cancer and low platelet counts are connected shows us that some cancers are more likely to cause this issue. This shows we need to treat each patient as an individual, focusing on their specific needs.
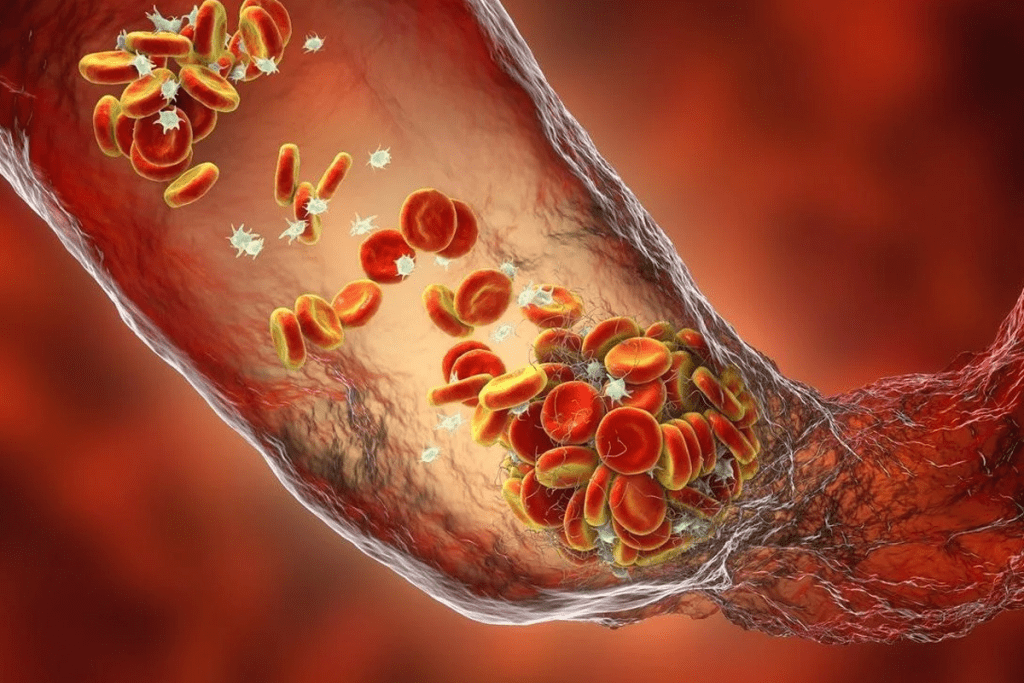
Platelets are vital for our health and for preventing disease. They are small, colorless cells in our blood that help stop bleeding. Their role is key in keeping us from bleeding too much after an injury.
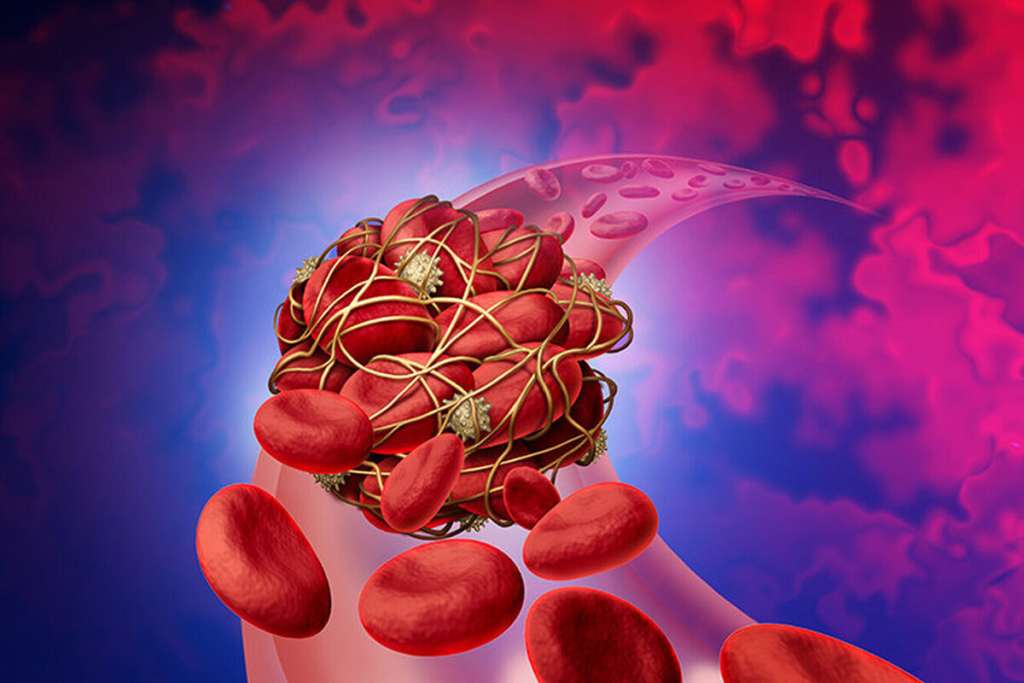
A normal platelet count is between 150,000 to 450,000 per microliter of blood. These cells live for about 8 to 12 days and are made in the bone marrow. Their main job is to clump together and form clots, which stop bleeding.
Having a normal platelet count is important for our health. It shows our body’s clotting system is working properly.
But platelet function is more than just count. How well they can form clots is also key. Problems with platelet function can cause bleeding, even with a normal count. So, knowing both count and function is important for assessing bleeding risks.
Thrombocytopenia is when you have too few platelets, usually less than 150,000 per microliter of blood. It can happen for many reasons, like not making enough platelets, destroying too many, or the spleen taking them in. This condition makes it harder for the body to clot, raising the risk of bleeding.
The severity of thrombocytopenia depends on the count. Counts below 50,000 are considered moderate to severe, and below 20,000 are severe. Knowing the cause and severity of thrombocytopenia is key to managing patients, like those with cancer, as it affects their treatment and outlook.
Key aspects of thrombocytopenia include:
Cancers causing thrombocytopenia, a condition that makes patient care harder. It affects how well treatments work. Thrombocytopenia, or low platelet count, is a big worry in cancer care.

Thrombocytopenia in cancer patients can happen in different ways. Bone marrow infiltration by cancer cells is a main reason. It messes up how platelets are made, leading to fewer of them.
Certain cancers also release things that stop platelets from being made or destroy them. This makes the problem worse.
Chemotherapy is another big reason for low platelets in cancer patients. Many chemo drugs slow down bone marrow, which makes platelet counts drop. How bad and long-lasting the low platelets are can depend on the chemo and the patient.
Thrombocytopenia is more common in some cancers than others. It’s more common in blood cancers than in solid tumors. For example, it’s a big problem in leukemia, lymphoma, and multiple myeloma.
Knowing how common thrombocytopenia is in cancer patients is key to treating it well. A study on non-Hodgkin lymphoma patients found a strong link between low platelets and how severe the disease is. In solid tumors like lung cancer and breast cancer, low platelets can make treatment harder and affect how well patients do.
By understanding how common and why thrombocytopenia happens in different cancers, doctors can better manage it. This can improve how patients are cared for and how well treatments work.
Cancers of the blood and bone marrow, known as hematologic malignancies, often cause low platelet counts. These cancers mess up the process of making blood cells, including platelets. Platelets are key to clotting and stopping bleeding.
Acute leukemia is when abnormal white blood cells grow fast in the bone marrow. This can cause the bone marrow to fail, leading to a lack of normal blood cells, including platelets. As a result, people with acute leukemia often have thrombocytopenia, or low platelet count. This increases their risk of bleeding.
Multiple myeloma is a cancer that grows in the bone marrow. It involves the growth of malignant plasma cells. These cells take over the bone marrow, stopping it from making normal blood cells.
This can cause anemia, infections, and thrombocytopenia. The bone marrow can’t make enough platelets, leading to bleeding problems. Keeping platelet counts in check is key for these patients.
Non-Hodgkin lymphoma (NHL) is a group of cancers that can harm the bone marrow and cause low platelet counts. Thrombocytopenia in NHL can happen in different ways. It can be due to lymphoma cells in the bone marrow, the immune system attacking platelets, or chemotherapy side effects.
It’s important to know why thrombocytopenia happens in NHL. This helps doctors manage it better.
Solid tumors can lower platelet counts, causing thrombocytopenia in cancer patients. This condition, marked by low platelet counts, can stem from the tumor itself or treatments.
Colorectal cancer often leads to thrombocytopenia. This is due to the tumor’s effects on the bone marrow and chemotherapy. Advanced colorectal cancer patients face a higher risk of thrombocytopenia.
“Thrombocytopenia in colorectal cancer patients complicates treatment and may affect survival,” studies show. Managing this condition requires monitoring platelet counts and adjusting chemotherapy.
Non-small cell lung cancer (NSCLC) is also linked to thrombocytopenia. The tumor environment in NSCLC can suppress platelet production. Chemotherapy and targeted therapy can also lower platelet counts.
Thrombocytopenia in NSCLC patients is linked to worse outcomes and bleeding risks. Early detection and management of low platelet counts are key in NSCLC care.
Ovarian cancer can cause thrombocytopenia through splenic sequestration and bone marrow effects. The tumor can pool platelets in the spleen and affect bone marrow function.
Splenic sequestration is a major factor in ovarian cancer-related thrombocytopenia. Managing this condition may involve reducing tumor burden or managing splenomegaly.
Gastrointestinal cancers, like gastric and pancreatic, can also lead to thrombocytopenia. These cancers can infiltrate the bone marrow, involve the spleen, or cause other mechanisms leading to low platelet counts.
Managing thrombocytopenia in gastrointestinal malignancies requires a team effort. Oncologists, hematologists, and other specialists work together to improve patient care.
Chemotherapy is a key factor that can cause low platelets in cancer patients. It targets fast-growing cells, including cancer cells and bone marrow cells that make platelets.
Chemotherapy with platinum, like cisplatin or carboplatin, can harm bone marrow. This leads to fewer platelets. The risk of low platelets depends on the platinum drug and the dose. For example, carboplatin is more likely to cause low platelets than cisplatin.
Gemcitabine is used to treat several cancers, including pancreatic, breast, and lung cancer. It can lower platelet counts. This happens because it stops bone marrow cells from making DNA, affecting platelet production. The risk goes up with higher doses.
Some chemotherapy plans are very intense or use many drugs that harm bone marrow. Studies show that up to 82% of patients on these plans get low platelets. This shows the importance of watching patients closely and finding ways to prevent this.
It’s vital to know the risks of different chemotherapy plans to manage low platelets in cancer patients. By spotting high-risk plans and taking steps to prevent low platelets, doctors can help patients better.
Diagnosing thrombocytopenia in cancer patients is a detailed process. It includes lab tests and clinical checks. Thrombocytopenia, defined as a low platelet count, affects cancer treatment and patient results.
Diagnosing thrombocytopenia starts with essential laboratory investigations. A complete blood count (CBC) is key to checking platelet count. More tests might include:
These tests are vital to find out why thrombocytopenia is happening and how to treat it.
It’s important to tell cancer-related thrombocytopenia apart from other types. Cancer-related thrombocytopenia can come from tumor cells in the bone marrow, chemotherapy side effects, or other cancer-related issues.
“Accurate diagnosis of thrombocytopenia is critical in cancer patients to guide treatment decisions and improve patient outcomes.”
Knowing the cause of thrombocytopenia helps doctors create specific plans. This can reduce complications and make cancer treatment better.
Cancer patients with low platelets face many challenges. These challenges can affect their treatment and how long they live. Low platelets can cause serious bleeding, make treatment harder, and impact survival.
Thrombocytopenia increases the risk of bleeding. Patients may bruise easily, get small spots under the skin, or even have severe bleeding. Managing bleeding is key and might include platelet transfusions or changing medications.
Handling bleeding needs a team effort. Doctors, hematologists, and others work together. Quick action is vital to avoid serious problems.
Thrombocytopenia can change how cancer is treated. It might mean reducing or delaying chemotherapy doses. Doctors must weigh the risks and benefits to treat the cancer while managing low platelets.
To adjust treatment, doctors might change chemotherapy plans. They might use treatments that are less hard on the bone marrow. Or, they might add supportive care to help with low platelets.
Thrombocytopenia can mean a worse prognosis for cancer patients. It might show the disease is more aggressive or the bone marrow is affected. Managing thrombocytopenia well is important for preventing bleeding and improving survival.
Studies show early treatment of thrombocytopenia is essential. It can help improve outcomes and survival rates for patients.
Managing thrombocytopenia in cancer patients requires teamwork. Oncologists, hematologists, and nurses work together. This team approach ensures patients get the best care possible.
Oncologists are key in managing thrombocytopenia. They adjust treatments to protect platelets. Their tasks include:
Hematologists specialize in managing thrombocytopenia. They do things like:
Nurses play a big role in caring for patients with thrombocytopenia. They focus on:
Important nursing actions include preventing falls, using gentle care to avoid bruises, and supporting patients emotionally.
Good communication among the healthcare team is vital. It helps manage thrombocytopenia well, reducing its effects on cancer treatment and patient results.
Managing cancer-related thrombocytopenia requires several key approaches. We will look at the guidelines and interventions used by healthcare providers.
Platelet transfusions are a common treatment for thrombocytopenia, mainly in patients with cancer or undergoing chemotherapy. The goal is to prevent or manage bleeding. Platelet transfusion guidelines suggest transfusing platelets when counts drop below certain levels, usually 10 × 10/L for stable patients and 20 × 10/L for those at higher risk.
We consider several factors when deciding on platelet transfusions. These include the patient’s overall health, the cause of thrombocytopenia, and the risk of bleeding. For example, patients with acute leukemia may need more frequent transfusions due to their high risk of bleeding.
Thrombopoietin receptor agonists (TRAs) are medications that boost platelet production. They are used in some cases of cancer-related thrombocytopenia, mainly when chemotherapy-induced thrombocytopenia is a concern. TRAs mimic the effect of thrombopoietin, a hormone that regulates platelet production.
We use TRAs like romiplostim and eltrombopag to treat thrombocytopenia in patients with chronic immune thrombocytopenia and some cases of myelodysplastic syndromes. Their use in cancer is growing, with ongoing research into their benefits and risks.
Chemotherapy dose modifications are key in managing thrombocytopenia in cancer patients. When thrombocytopenia occurs, we may adjust the chemotherapy regimen. This balances the need for effective cancer treatment with the risk of bleeding complications.
Dose reductions or temporary interruptions of chemotherapy can help manage thrombocytopenia. We weigh the benefits of continuing chemotherapy against the risks of low platelet counts. Adjustments are made as needed to ensure patient safety.
By using these treatment strategies, we can effectively manage cancer-related thrombocytopenia and improve patient outcomes.
To prevent thrombocytopenia, we must assess risks before treatment starts. We teach patients to spot early signs of low platelet counts. This helps us target high-risk patients and reduce the risk of a serious side effect from cancer treatment.
Before starting cancer treatment, a detailed check is key. We look at the patient’s medical history, current platelet count, and the planned treatment. Those with a history of blood cancers or past chemotherapy are at higher risk and need closer watch.
It’s vital to keep an eye on platelet counts during treatment, more so for high-risk patients. Frequent blood tests help catch thrombocytopenia early. We also adjust chemotherapy doses and timing to lower the risk of low platelet counts.
We might adjust chemotherapy doses or pause treatment to let platelet counts bounce back. For very high-risk patients, prophylactic platelet transfusions might be an option.
Teaching patients about thrombocytopenia signs is key. They should know the risks of low platelet counts and report any bleeding or bruising. This way, we can catch problems early and prevent serious issues.
By doing thorough checks before treatment, monitoring closely, and educating patients, we can manage thrombocytopenia risk. This approach improves outcomes for cancer patients.
The fight against thrombocytopenia in cancer is about to get a big boost. New treatments are on the horizon. These could change how we treat this condition.
New research is showing promise in treating thrombocytopenia. These new agents aim to boost platelet production. This could help prevent thrombocytopenia in cancer patients.
New cancer treatments aim to protect platelet counts. They want to fight cancer well but gently on platelets. Some examples are:
Genetic research is showing how genes affect thrombocytopenia risk. This knowledge helps in:
Looking ahead, combining new treatments, targeted cancer therapies, and genetic insights will greatly help cancer patients with thrombocytopenia.
Thrombocytopenia is a big problem in many cancers, making treatment harder. Cancers like breast, lung, ovarian, and others can lead to low platelet counts. Knowing how cancer affects platelets is key to better thrombocytopenia management.
Platelets are vital for our health, and cancer can disrupt this. We’ve looked at how cancers cause low platelet counts and how to manage them. This knowledge helps doctors and nurses improve care for patients.
By understanding the link between cancer and low platelet counts, we can do better for our patients. As research grows, we’ll find new ways to help cancer patients with thrombocytopenia.
Thrombocytopenia is when you have too few platelets in your blood. Platelets help your blood clot. Having too few can make you bleed more easily.
Many cancers can cause thrombocytopenia. This includes blood cancers like leukemia and lymphoma. Solid tumors like lung and ovarian cancer can also cause it.
Chemotherapy can lower your platelet count. This is true for treatments using platinum or gemcitabine. These drugs can slow down platelet production.
Thrombocytopenia can cause serious bleeding. This can make it hard to manage cancer treatment. It might mean changing treatment plans or slowing them down.
Doctors use blood tests and bone marrow exams to find thrombocytopenia. It’s important to know if it’s caused by cancer or something else.
Doctors might give platelet transfusions or use special drugs. They might also change how they give chemotherapy. The best plan depends on how bad the thrombocytopenia is and the type of cancer.
Yes, doctors can try to prevent it. They check patients before starting treatment. They also keep an eye on them during treatment. Teaching patients about the signs of thrombocytopenia is also important.
Scientists are working on new treatments. They want to make drugs that help platelets and don’t cause thrombocytopenia. These new treatments aim to improve platelet counts and reduce bleeding risks.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!