Last Updated on October 31, 2025 by
We are dedicated to giving top care to those with carcinoma in situ. This is a condition where abnormal cells stay put without spreading. It’s a stage 0 cancer, meaning it hasn’t invaded nearby tissues.
Knowing about carcinoma in situ is key for catching it early. At Liv Hospital, we use our global knowledge and focus on the patient. We aim to spot and treat precancerous changes with the latest medical methods.
Key Takeaways
- Carcinoma in situ is a non-invasive, stage 0 cancer.
- Abnormal cells remain in their original location.
- Early detection and treatment can prevent progression to invasive cancer.
- Liv Hospital provides international expertise and patient-centered care.
- Current medical protocols are used to treat precancerous changes.
The Medical Definition of Carcinoma In Situ

To understand carcinoma in situ, we must look at its Latin roots and its role in medicine. The word ‘in situ’ comes from Latin, meaning ‘in its place.’ It shows that these cells are stuck in one spot, not spreading.
The Latin Origin of “In Situ” and Its Clinical Significance
The term “in situ” is key to knowing about carcinoma in situ. It means the cancer cells are stuck in their original spot and haven’t moved to other areas. This is what makes CIS different from invasive cancer.
“The term ‘in situ’ shows these cancer cells are stuck in one place,” says a top oncologist. “This is important for knowing how well a patient will do and what treatments they might need.”
Distinguishing Features from Invasive Cancer
Carcinoma in situ is different from invasive cancer in important ways. CIS is non-invasive, meaning it hasn’t broken through the basement membrane or spread to other tissues. This is why it’s so important for figuring out the right treatment and understanding the patient’s future.
- Carcinoma in situ is stuck in the epithelial layer.
- It hasn’t invaded the surrounding tissues or spread to other places.
- If not treated, it could turn into invasive cancer.
Knowing these differences is key for patients to understand their diagnosis and what it means for their treatment. Finding CIS early gives doctors a chance to act before it becomes invasive.
Understanding Carcinoma In Situ Biology

It’s key to know about carcinoma in situ biology for early cancer detection and treatment. We look into CIS cells’ unique traits and what they mean for patient care.
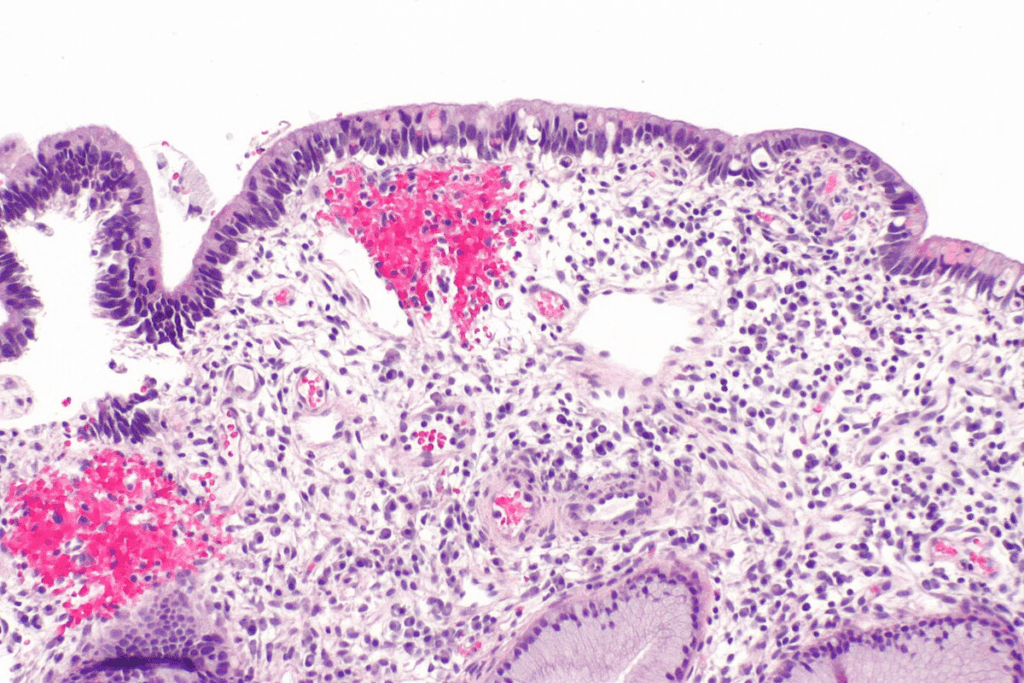
Cellular and Molecular Characteristics
CIS cells have odd cellular and molecular traits, like invasive cancer cells. They show irregular cell shape, changed gene activity, and odd cell behavior. Yet, CIS cells stay in the epithelial layer.
The traits of CIS cells include:
- Odd cell growth and division
- Disrupted cell structure
- Genetic and epigenetic changes
Confinement to the Epithelial Layer: Why It Matters
CIS cells staying in the epithelial layer is key. It stops them from reaching blood vessels and lymphatic paths, lowering metastasis risk. This is vital for CIS prognosis and treatment.
Why confinement is important includes:
- It stops metastasis by blocking blood and lymph access
- It leads to a better prognosis than invasive cancer
- It allows for less harsh treatment options
Knowing about carcinoma in situ biology helps us see why early detection and right management are so important.
Carcinoma In Situ in the Cancer Staging System
Carcinoma in situ is called stage 0 cancer in the TNM system. This shows it’s not invasive. Knowing this helps doctors understand what to do next and how well a patient will do.
Stage 0 Classification in the TNM System
The TNM system is made by the International Union Against Cancer (UICC). It helps doctors figure out how serious a cancer is. Carcinoma in situ is stage 0 because it hasn’t spread to other tissues.
This is key because it shows CIS is different from cancers that have spread. Those are called stage I to stage IV.
Stage 0 cancer means the tumor is non-invasive. It hasn’t spread past the layer it started in. This is important for choosing the right treatment and knowing how well a patient will do.
Prognostic Implications of Non-Invasive Status
The fact that CIS is non-invasive is very important. It usually means the cancer is easier to treat and less likely to spread.
Knowing this helps doctors pick the best treatment. We’ll talk about how this affects treatment choices and managing CIS.
Treatment decisions for stage 0 cancer aim to stop it from becoming worse. They also try to avoid too many side effects. Because CIS is non-invasive, doctors have many options. These range from surgery to less invasive methods.
Common Types of Carcinoma In Situ
There are several common types of carcinoma in situ. Each has its own characteristics and importance. Knowing these differences helps doctors diagnose and treat better.
Ductal Carcinoma In Situ (DCIS) of the Breast
Ductal carcinoma in situ (DCIS) is a non-invasive breast cancer. It stays in the milk ducts without spreading. It’s often found through mammograms and is a big part of breast cancer cases, with about 56,000 new cases in the U.S. each year.
Key Features of DCIS:
- Non-invasive, confined to milk ducts
- Often detected through mammography
- High incidence, with 56,000 annual diagnoses in the U.S.
- Variable grade, from low to high nuclear grade
Cervical Carcinoma In Situ
Cervical carcinoma in situ means abnormal cells on the cervix’s surface. These cells haven’t invaded deeper tissues yet. It’s found through Pap smear tests and is a step before invasive cervical cancer.
Importance of Screening: Regular Pap smears are key to finding cervical carcinoma in situ. They help stop it from becoming invasive cancer.
Squamous Cell Carcinoma In Situ of the Skin and Mucosa
Squamous cell carcinoma in situ (Bowen’s disease) is when abnormal squamous cells stay in the epidermis. It happens on the skin and mucosal surfaces.
| Type | Location | Key Characteristics |
| Ductal Carcinoma In Situ (DCIS) | Breast | Non-invasive, confined to milk ducts |
| Cervical Carcinoma In Situ | Cervix | Precursor to invasive cervical cancer, detected by Pap smear |
| Squamous Cell Carcinoma In Situ | Skin and Mucosa | Abnormal squamous cells confined to epidermis |
Detecting and Diagnosing Carcinoma In Situ
Diagnosing carcinoma in situ requires screening tests and biopsies. Finding it early is key to successful treatment.
Screening Methods for Different Types
Screening methods vary by type and location. For example, mammography is used to find ductal carcinoma in situ (DCIS) in the breast. It helps spot abnormal cell growth early.
Pap smears are used to find cervical carcinoma in situ. They are part of routine gynecological exams. Pap smears can find precancerous and cancerous cells in the cervix.
- Mammography for breast CIS
- Pap smears for cervical CIS
- Dermatological examinations for skin CIS
These methods are essential for catching carcinoma in situ early. This makes it easier to treat.
Biopsy Techniques and Pathological Assessment
When screening tests show CIS, biopsy techniques are used to confirm it. A biopsy takes a small tissue sample from the area in question.
The biopsy sample is then checked under a microscope in pathological assessment. This step is key to confirming CIS and ruling out invasive cancer.
- Needle biopsy for breast lesions
- Colposcopy-guided biopsy for cervical lesions
- Skin biopsy for dermatological lesions
Pathological assessment not only confirms the diagnosis but also helps guide treatment.
Comprehensive Treatment Approaches for Carcinoma In Situ
Managing CIS requires a variety of treatments. These include surgery and non-surgical methods. The right treatment depends on the CIS’s type, size, and location. It also depends on the patient’s health and what they prefer.
Surgical Management Options
Surgery is often the first step in treating CIS. Lumpectomy and mastectomy are common surgeries. For example, if CIS is found in the breast, a lumpectomy followed by radiation might be suggested.
“The main goal of surgery is to remove all CIS cells,” explains Dr. Jane Smith, a leading oncologist. “Whether to choose lumpectomy or mastectomy depends on the CIS’s size and the patient’s wishes.”
Non-Surgical Treatments
Non-surgical treatments are also used for CIS. Radiation therapy is often used after surgery to kill any leftover cancer cells. Hormonal therapy is also recommended for CIS that is hormone receptor-positive.
- Radiation therapy to eliminate remaining cancer cells
- Hormonal therapy to reduce the risk of recurrence in hormone receptor-positive CIS
- Close surveillance to monitor for any signs of progression
Personalized Treatment Decision-Making
Choosing the right treatment for CIS is very personal. Doctors and patients work together to find the best plan. This plan considers the CIS’s details, the patient’s health, and their personal choices.
The American Cancer Society agrees. “Patients should be involved in making treatment decisions. They should think about the benefits and risks of each option. They should also consider their own values and preferences.”
Risk Assessment and Progression to Invasive Cancer
It’s important to know what makes carcinoma in situ (CIS) turn into invasive cancer. CIS is a stage where abnormal cells are stuck in the top layer of cells. But, these cells can grow and spread to other tissues.
Knowing the risk helps doctors choose the right treatment and care plan. We’ll look at what makes CIS more likely to become invasive. We’ll also talk about how to keep an eye on patients.
Predictive Factors for Malignant Transformation
Several things can tell us if CIS might turn into invasive cancer. These include:
- Histological grade: How much the CIS cells look like normal cells matters a lot.
- Size and extent: Bigger CIS areas or those that spread out more are at higher risk.
- Biological markers: Some markers, like hormone receptors in breast CIS, can raise the risk.
- Genetic factors: Changes in genes, like in BRCA1 and BRCA2, can also increase the risk.
For example, women with lobular carcinoma in situ (LCIS) face a 25% to 30% chance of getting breast cancer. Knowing these factors helps doctors plan the best care for each patient.
Surveillance Protocols and Follow-up Care
Watching CIS closely is key to catching any changes early. The right watch plan depends on the CIS type and the patient’s risk.
For breast CIS, like ductal carcinoma in situ (DCIS), patients might get regular mammograms and check-ups. They might also have MRI scans. How often they get these tests depends on their treatment and risk level.
Good watch plans help find invasive cancer early. This means doctors can act fast, which can help a lot. We make sure each patient gets care that fits their needs.
By understanding CIS risks and using the right watch plans, we can help CIS patients a lot. This way, we can catch any problems early and treat them quickly.
Living With a Carcinoma In Situ Diagnosis
Getting a carcinoma in situ diagnosis can stir up many feelings. You might feel relieved it’s not invasive but also worried about what’s next. It’s key to look at the medical side, but also the emotional and lifestyle effects.
Psychological Impact and Support Resources
The emotional side of a carcinoma in situ diagnosis is big. People often feel scared, worried about treatment, and unsure about the future. It’s important to find support to deal with these feelings and make good choices about care.
Support can be many things, like counseling, support groups, and online help. Talking to others who’ve been through the same thing can offer comfort and useful advice. We suggest looking into these options to see what fits best for you.
Lifestyle Considerations and Risk Reduction Strategies
Changing your lifestyle is key in managing carcinoma in situ and lowering the chance of it becoming invasive cancer. Making smart choices about what you eat, exercise, and other health habits can help you stay healthy and possibly lower cancer risk.
Many people worry too much about DCIS coming back, but knowing the real risk can help calm those fears. By living a balanced life and sticking to the recommended check-ups, you can actively manage your condition.
- Eating a balanced diet rich in fruits, vegetables, and whole grains
- Engaging in regular physical activity to improve overall health
- Avoiding smoking and limiting alcohol consumption
- Following the recommended screening and follow-up care schedule
By focusing on these lifestyle changes and staying informed, patients can face their diagnosis with confidence and strength.
Conclusion: Navigating the Journey from Diagnosis to Recovery
Getting a carcinoma in situ diagnosis can be tough. But, with the right info and support, patients can make smart choices about their care. We’ve looked at what carcinoma in situ is, how it works, and how to treat it. This shows why finding it early and treating it right is key.
When you get a carcinoma in situ diagnosis, you need to act fast. Most people with ductal carcinoma in situ (DCIS) are alive 20 years later. This shows how good the treatment is. Knowing about your condition helps you take charge of your recovery and feel sure about your journey.
In the end, a carcinoma in situ diagnosis is more than a health issue. It’s a chance to take care of your health. We urge patients to team up with their doctors to create a treatment plan that works best for them. This way, they can have the best outcome and an easy recovery.
FAQ
What does carcinoma in situ mean?
Carcinoma in situ means abnormal cells are stuck in one place. They haven’t spread to other tissues. It’s called stage 0 cancer.
What is the significance of carcinoma in situ?
Knowing about carcinoma in situ helps catch it early. This can stop it from becoming worse.
What does “in situ” mean in the context of cancer?
“In situ” means “in its place.” It shows the cells haven’t spread to other areas.
How is carcinoma in situ different from invasive cancer?
Carcinoma in situ doesn’t spread. The cells stay in one layer and don’t get into blood or lymph. This stops it from spreading.
What are the common types of carcinoma in situ?
There are a few types. These include ductal carcinoma in situ (DCIS) of the breast, cervical carcinoma in situ, and squamous cell carcinoma in situ of the skin and mucosa.
How is carcinoma in situ diagnosed?
Doctors use tests like mammograms for DCIS and Pap smears for cervical CIS. They also do biopsies and check the cells.
What are the treatment options for carcinoma in situ?
Doctors might use surgery like lumpectomy or mastectomy. They might also use radiation or hormone therapy. Treatment depends on the CIS and what the patient wants.
What is the risk of carcinoma in situ progressing to invasive cancer?
The risk depends on the type of CIS and the patient. Watching patients closely is key to catch any changes.
How does a carcinoma in situ diagnosis affect patients psychologically?
Getting a CIS diagnosis can be tough. Patients need support to deal with it. This helps lower the chance of it getting worse.
What lifestyle considerations and risk reduction strategies are recommended for patients with carcinoma in situ?
Patients can make lifestyle changes to help manage CIS. This can lower the risk of it getting worse.
What does stage 0 cancer mean in the TNM staging system?
Stage 0 cancer means it’s not spreading. This is important for treatment plans and how well patients do.
Why is early detection of carcinoma in situ important?
Finding CIS early is key. It helps stop it from getting worse. This improves how well patients do.
References
- National Health Service (NHS). (2025). What Is Carcinoma In Situ A Complete Definition. Retrieved from https://www.nhs.uk/conditions/carcinoma-in-situ