Last Updated on October 31, 2025 by

Did you know that one in four new breast cancer diagnoses is actually carcinoma in situ? It’s a stage 0 cancer that hasn’t spread yet. Knowing about this condition could help find cancer early, when it’s most treatable.
At Liv Hospital, we combine top-notch expertise with caring service. Carcinoma in situ (CIS) is a group of abnormal cells that haven’t spread. They stay in one area of the body.
The word in situ comes from Latin, meaning “in its original place.” This is a stage 0 cancer. It’s non-invasive and stays in its first location, not spreading to other tissues.
Carcinoma in situ definition is a condition where cancer cells are present but haven’t spread. This stage is key because it’s a chance to stop the disease before it gets worse.
To grasp CIS’s importance, we need to know what “in situ” means.
The term “in situ” comes from Latin, meaning “in its original place.” In cancer, it means abnormal cells stay in their place without spreading.
This idea is important because it shows a time when we can stop cancer from getting worse.
Carcinoma in situ is called stage 0 cancer. This is important because it means the cancer is in its early stages and hasn’t spread.
Key Characteristics of Stage 0 Cancer:
Knowing the difference between CIS and invasive cancer is key for early treatment. Invasive cancer has spread and needs stronger treatments.
| Characteristics | Carcinoma in Situ (CIS) | Invasive Cancer |
| Invasiveness | Non-invasive | Invasive |
| Stage | Stage 0 | Stage 1 and beyond |
| Treatment Approach | Localized therapies, possible complete removal | More aggressive treatments, including surgery, chemotherapy, and radiation |
Understanding CIS and its difference from invasive cancer helps us see why early detection is so important. It shows how effective treatment can be at this stage.
Understanding carcinoma in situ is key to knowing how it starts and grows. It’s a stage where cells change but don’t spread. These changes mark the beginning of cancer.
Cellular Changes and Characteristics
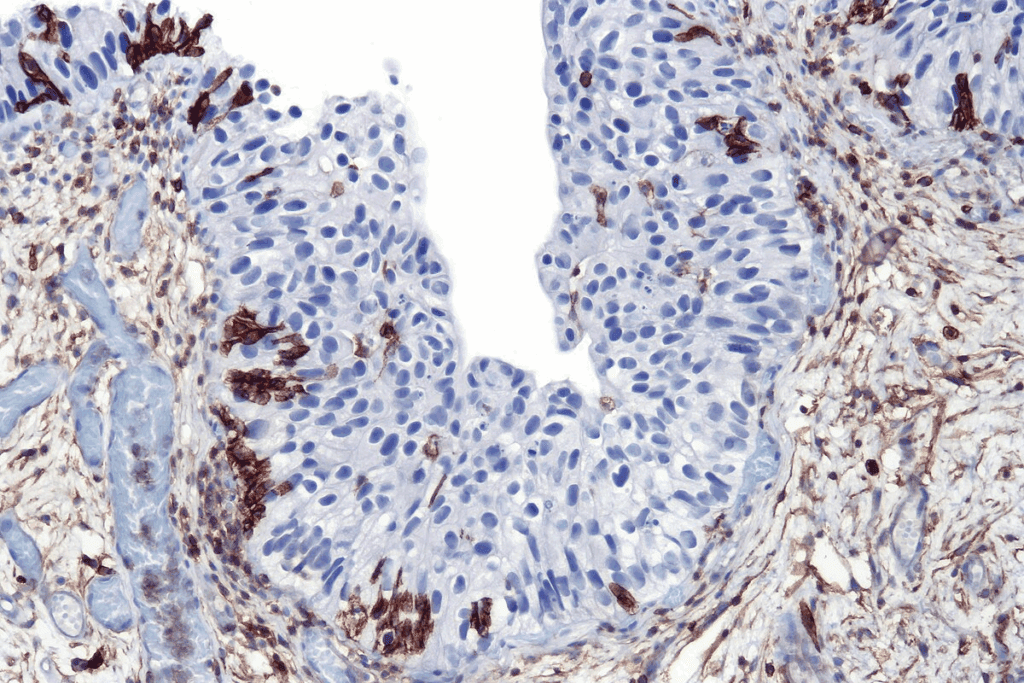
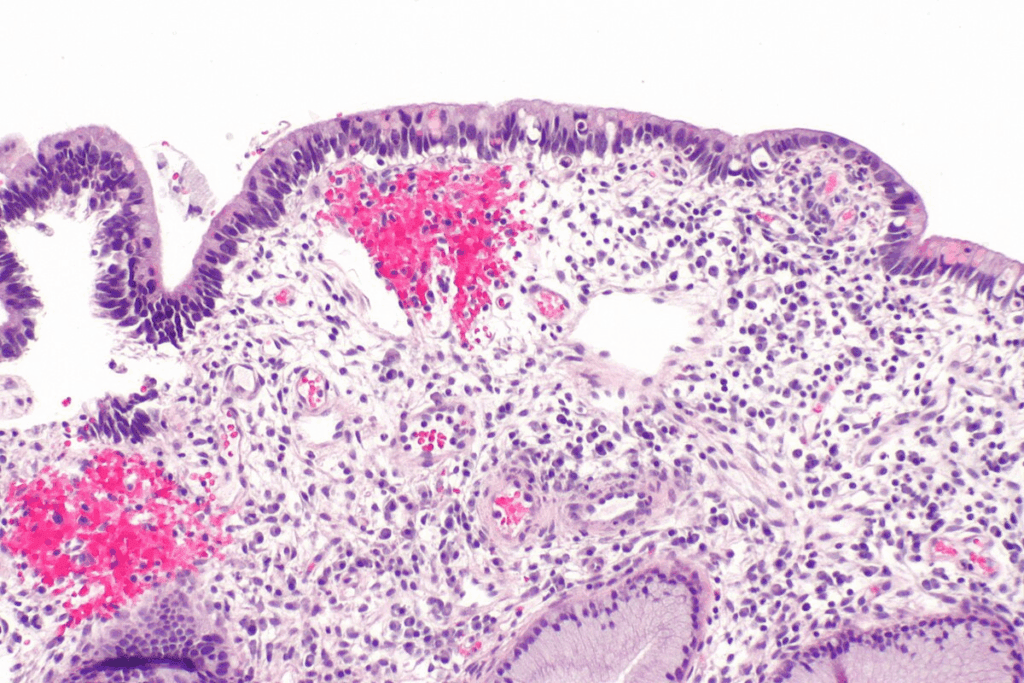
Carcinoma in situ has cancer cells that haven’t crossed the basement membrane. This membrane is a key barrier between cells and tissue. These cells look different from normal cells under a microscope.
Doctors diagnose carcinoma in situ by looking at these cell changes during a biopsy. These changes can range from mild to severe, showing how abnormal the cells are.
Carcinoma in situ also has specific molecular markers and genetic factors. These help predict how the condition might progress. They show if it could turn into invasive cancer.
Studies have found genetic mutations in carcinoma in situ similar to invasive cancers. Knowing these changes helps in creating better treatments. It also helps find who’s at higher risk.
Studying carcinoma in situ’s biology helps us understand its complex changes. This knowledge is vital for making targeted treatments. It also improves how we care for patients.
It’s important to know about the different types of carcinoma in situ. This stage 0 cancer includes several conditions, each with its own traits. These traits affect how doctors treat and care for patients.
Ductal carcinoma in situ (DCIS) is a type of breast cancer. It’s found in the ducts but hasn’t spread to the rest of the breast. About 20-25 percent of new breast cancer cases in the U.S. are DCIS.
DCIS starts in the milk ducts and hasn’t spread. The cells in the ducts have changed but haven’t invaded the surrounding tissue. Early detection through mammograms has greatly improved DCIS diagnosis.
Key characteristics of DCIS include:
Lobular carcinoma in situ (LCIS) starts with DNA changes in a milk-producing gland. It’s not a true cancer but signals a higher risk of breast cancer.
LCIS is often found by accident during a biopsy for another reason. It’s more common in women who haven’t gone through menopause yet.
Key aspects of LCIS:
Cervical carcinoma in situ, or cervical intraepithelial neoplasia (CIN), is when abnormal cells are found on the cervix. These cells could turn into cancer if not treated.
CIN is divided into three stages: CIN1 (mild dysplasia), CIN2 (moderate dysplasia), and CIN3 (severe dysplasia or carcinoma in situ).
There are other types of carcinoma in situ, affecting different parts of the body. These include:
Each type of carcinoma in situ has its own characteristics and treatment plans. Knowing these differences is key to giving the right care and support to patients.
The study of carcinoma in situ shows us how common it is and who is at risk. By looking at the numbers and who gets CIS, we learn how it affects health. We also find out who is more likely to get it.
In the U.S., CIS is a big health issue. Different types of CIS affect different people. For example, ductal carcinoma in situ (DCIS) is a common type of breast cancer in situ. It’s becoming more common because of better screening.
Some important facts are:
Knowing who is at risk for CIS helps us prevent and catch it early. Important risk factors include:
Women with LCIS have a 25% to 30% chance of getting breast cancer over their lifetime. This is much higher than the general risk of about 13%. Knowing these numbers helps us focus on early detection and prevention.
By studying CIS, we can make our health strategies more effective. This helps us tackle CIS better.
Carcinoma in situ shows different signs, often found through screening, not symptoms. It’s an early cancer stage where cells haven’t spread. Knowing its symptoms, or the lack of them, is key for early treatment.
Many cases of carcinoma in situ don’t show symptoms. For example, ductal carcinoma in situ (DCIS) might not show symptoms but can cause a lump or nipple discharge. This shows why regular screening is so important.
If you notice any unusual changes, like a new lump or nipple discharge, see a doctor. Early detection through screening can greatly improve treatment outcomes for CIS.
| Type of CIS | Common Symptoms | Detection Methods |
| Ductal Carcinoma in Situ (DCIS) | Lump, nipple discharge | Mammogram |
| Lobular Carcinoma in Situ (LCIS) | Usually asymptomatic | Biopsy for other conditions |
| Cervical Carcinoma in Situ (CIN) | Abnormal Pap smear | Pap smear, colposcopy |
Getting a correct in situ cancer definition is key for good treatment. It uses imaging, biopsy, and looking at tissues under a microscope. Finding carcinoma in situ (CIS) needs a detailed approach to manage it well.
Imaging is very important for CIS diagnosis. Mammography is a big help, mainly for ductal carcinoma in situ (DCIS). It spots microcalcifications linked to this condition.
Ultrasound and magnetic resonance imaging (MRI) also help. MRI is great at seeing how far DCIS has spread. This helps plan treatment.
| Imaging Technique | Primary Use in CIS Diagnosis | Benefits |
| Mammography | Detection of microcalcifications associated with DCIS | High sensitivity for detecting calcifications; widely available |
| Ultrasound | Evaluation of palpable abnormalities; assessment of lymph nodes | Useful for characterizing lesions; guides biopsy procedures |
| MRI | Assessment of disease extent; evaluation of multifocality | High sensitivity for detecting extent of disease; helpful in surgical planning |
Biopsy is key for a sure CIS diagnosis. The main types are core needle biopsy and surgical biopsy.
“The choice of biopsy technique depends on various factors, including the size and location of the lesion, as well as the patient’s overall health status.”
— Expert Opinion
Core needle biopsy is less invasive and often first used. Surgical biopsy is for when more tissue is needed or if the diagnosis is unsure.
Looking at tissues under a microscope is the best way to diagnose CIS. It confirms CIS and tells it apart from invasive cancer.
It checks the cells and how they are arranged. Histological grading and molecular markers give more info on how likely the cancer is to grow.
Getting the diagnosis right is very important for treatment. Using imaging, biopsies, and looking at tissues helps doctors give the best care for CIS.
Carcinoma in situ treatment depends on the type and location of the condition. The choice of treatment is influenced by factors such as the grade and size of the CIS, as well as the patient’s overall health.
Surgery is a common treatment for carcinoma in situ, aiming to remove the abnormal cells before they become invasive. The type of surgery depends on the location and extent of the CIS.
Radiation therapy is often used after surgery to eliminate any remaining abnormal cells, reducing the risk of recurrence.
For certain types of CIS, medication or hormonal treatments may be recommended, mainly for hormone receptor-positive CIS.
| Treatment Type | Description | Use Case |
| Endocrine Therapy | Blocks hormone receptors or reduces hormone production. | Hormone receptor-positive CIS |
| Chemoprevention | Uses medications to reduce cancer risk. | High-risk patients or those with specific genetic markers |
For some patients with low-risk CIS, active surveillance may be an appropriate option. This involves regular monitoring with imaging tests and biopsies.
Understanding the various treatment options for carcinoma in situ is key for making informed decisions. Patients should discuss their individual circumstances and the most appropriate treatment plan with their healthcare provider.
Knowing the prognosis of carcinoma in situ is key for good patient care. The outlook for CIS is very good, with a high chance of survival with the right treatment.
Several things can change the chance of CIS turning into invasive cancer. These include the grade and size of the lesion, and certain molecular markers.
A study in a top medical journal found that “The presence of high-grade nuclear features and comedonecrosis in ductal carcinoma in situ (DCIS) is associated with a higher risk of recurrence and progression to invasive cancer.”
“The management of DCIS remains challenging due to the heterogeneity of the disease and the varying risk of progression to invasive cancer.”
Survival rates for CIS are very high, thanks to early detection and treatment.
| Type of CIS | 10-year Survival Rate | 20-year Survival Rate |
| Ductal Carcinoma in Situ (DCIS) | 98% | 96% |
| Lobular Carcinoma in Situ (LCIS) | 95% | 90% |
The table shows that survival rates for DCIS and LCIS are excellent. This highlights the importance of catching it early and managing it well.
In summary, CIS is an early stage of cancer, but knowing its prognosis and natural history is critical for patient care. By looking at factors that affect progression and using high survival rates, doctors can create treatment plans that help patients a lot.
Recent studies have greatly improved our understanding of carcinoma in situ. They have shed new light on its biology and treatment. As research keeps evolving, we learn more about this complex condition.
New research has been key in understanding carcinoma in situ. Genomic tests can now help assess the risk of recurrence. This allows for more personalized treatment plans.
For example, genomic profiling helps identify genetic markers linked to a higher risk of invasive cancer.
Some important research areas include:
These studies have helped healthcare providers offer more targeted and effective care.
New treatment methods are changing how we manage carcinoma in situ. Advances in medical technology and a better understanding of the disease offer tailored treatment options.
Some new treatment approaches are:
These innovative methods are improving patient outcomes and quality of life. As research advances, we can expect even more effective treatments.
Getting a carcinoma in situ (CIS) diagnosis can change your life. CIS is not invasive cancer, but it needs careful handling. It also has big emotional effects.
A CIS diagnosis can really affect your life and mind. The news can be scary, making you feel anxious, fearful, and unsure about the future. It’s important to recognize these feelings and get help when you need it. You might feel shocked, deny it, get angry, or feel sad.
To deal with these feelings, you can:
Support is key when facing a CIS diagnosis. Family and friends offer emotional support, while doctors provide medical advice and treatment plans. Many organizations also offer counseling, support groups, and resources for cancer patients.
Good ways to cope include:
Using these resources and strategies can help you handle CIS better. It can also improve your overall life quality.
Carcinoma in situ, or CIS, is a condition where cancer cells are present but haven’t spread. It’s important to understand CIS early to treat it effectively. If not treated, CIS can turn into invasive cancer.
In situ carcinoma is a condition that doesn’t spread but needs proper care. We’ve covered many aspects of CIS, like its definition, types, and how common it is. We also talked about its symptoms, how to diagnose it, treatment options, and what the future looks like.
Knowing about in situ carcinoma is very important. By understanding CIS, people can take steps to protect their health. This includes regular check-ups and acting quickly when needed. We stress the need for a complete approach to managing CIS for the best results.
Carcinoma in situ is when abnormal cells stay in their original place. They haven’t spread to other tissues yet. It’s an early sign of cancer.
Yes, it is. Carcinoma in situ is stage 0 cancer. It means there’s abnormal cell growth that hasn’t spread.
The main difference is where the cells are. Carcinoma in situ cells stay in their original spot. Invasive cancer cells spread to other areas, which can lead to more serious problems.
There are a few common types. These include ductal carcinoma in situ (DCIS), lobular carcinoma in situ (LCIS), and cervical carcinoma in situ (CIN).
Doctors use imaging, biopsies, and lab tests to find abnormal cells. This confirms if it’s carcinoma in situ.
Treatments vary. They can include surgery, radiation, medicine, hormone therapy, or watching it closely. It depends on the CIS type and where it is.
Yes, it can. If not treated, CIS might turn into invasive cancer. But, the chance of this happening depends on several things.
Several factors can increase your risk. These include genetics, lifestyle, and certain demographics. The specific risks vary by CIS type.
Understanding CIS and getting support are key. Talk to doctors and loved ones. Look into treatment options to manage it well.
The outlook is good. Early detection and treatment lead to high survival rates. This is true for most CIS cases.
“In situ” means the abnormal cells are only in their original place. They haven’t spread to other areas.
Yes, it is. Even though it’s an early cancer stage, it needs quick medical attention. This helps prevent it from becoming more serious.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!