Cardiac rehabilitation helps people with heart disease get healthier. It includes exercise training, emotional support, and education on a heart-healthy lifestyle. Cardiopulmonary physical therapy exercises are key in this process. They help restore heart function and improve overall health.
Cardiac rehab programs use aerobic, strength, and balance exercises. They offer a complete approach to recovery. We help patients learn these exercises well, so they get the best results.
Key Takeaways
- Cardiac rehabilitation is a supervised program that improves health in individuals with heart disease.
- Exercise training is a critical part of cardiac rehabilitation.
- Cardiopulmonary exercises are vital for restoring heart function and improving life quality.
- A complete cardiac rehab program also includes emotional support and lifestyle education.
- It’s important to do therapeutic exercises correctly for the best recovery.
Understanding Cardiac Rehabilitation and Its Benefits

Recovering from a heart event is more than just medical care. It’s about a complete cardiac rehab program. This program helps patients get better from heart issues and lowers the chance of future heart problems.
What Is Cardiac Rehabilitation?
Cardiac rehab is a program that mixes exercise training, emotional support, and education on a heart-healthy lifestyle. It helps patients understand and manage their heart condition. They learn to make lifestyle changes to avoid more heart problems.
Evidence-Based Benefits of Exercise-Based Cardiac Rehab
Studies show that exercise-based cardiac rehabilitation cuts down on heart deaths and hospital stays. The benefits of cardiac rehab are clear. They include better heart health, improved physical function, and a lower risk of future heart issues.
Benefits | Description |
Improved Heart Health | Enhanced cardiovascular function and reduced risk of future heart issues |
Enhanced Physical Function | Increased strength, endurance, and flexibility |
Reduced Hospitalizations | Lower risk of hospital readmission due to cardiac complications |
Who Should Participate in Cardiac Rehab Programs
Cardiac rehab is for people who have had heart problems or events, like heart attacks or surgery. It’s also good for those at risk of heart disease. It teaches them how to manage these risks.
Knowing about cardiac rehab helps patients take charge of their recovery and heart health. Our programs offer full support to help patients get the best results.
Getting Started: Preparation for Cardiac Rehabilitation

The journey to recovery through cardiac rehabilitation starts with preparation. This includes getting medical clearance and setting up a good exercise space. Starting a new exercise program, after a heart event, can be scary. It’s key to take the right steps for a safe and effective recovery.
Medical Clearance and Initial Assessment
Before starting cardiac rehab, patients get a detailed initial assessment. This checks their heart health and finds any limits. A cardiopulmonary exercise test (CPET) is used to see how well they can exercise. It helps create a plan just for them.
Key components of the initial assessment include:
- Medical history review
- Physical examination
- Cardiopulmonary exercise testing (CPET)
- Risk stratification for future cardiac events
Setting Up Your Exercise Space
Having a safe and good space for exercise at home is important. Choose a spot that’s free from distractions and dangers. It should be well-ventilated, well-lit, and at a comfortable temperature.
Essential Equipment for Home-Based Cardiac Rehab
While you don’t need a lot of equipment for home rehab, the right tools help. Essential items include:
Equipment | Purpose | Benefits |
Heart Rate Monitor | Track heart rate during exercise | Ensures safe exercise intensity |
Exercise Mat | Provides comfort during floor exercises | Reduces risk of injury |
Resistance Bands | Facilitates strength training | Improves muscle strength and endurance |
Treadmill or Stationary Bike | Enables aerobic exercise | Enhances cardiovascular fitness |
By preparing well for cardiac rehab, patients can ensure a safe and effective recovery. Getting medical clearance and setting up a good exercise space are key. A well-prepared start is important for a successful rehab program.
Essential Cardiopulmonary Physical Therapy Exercises for Recovery
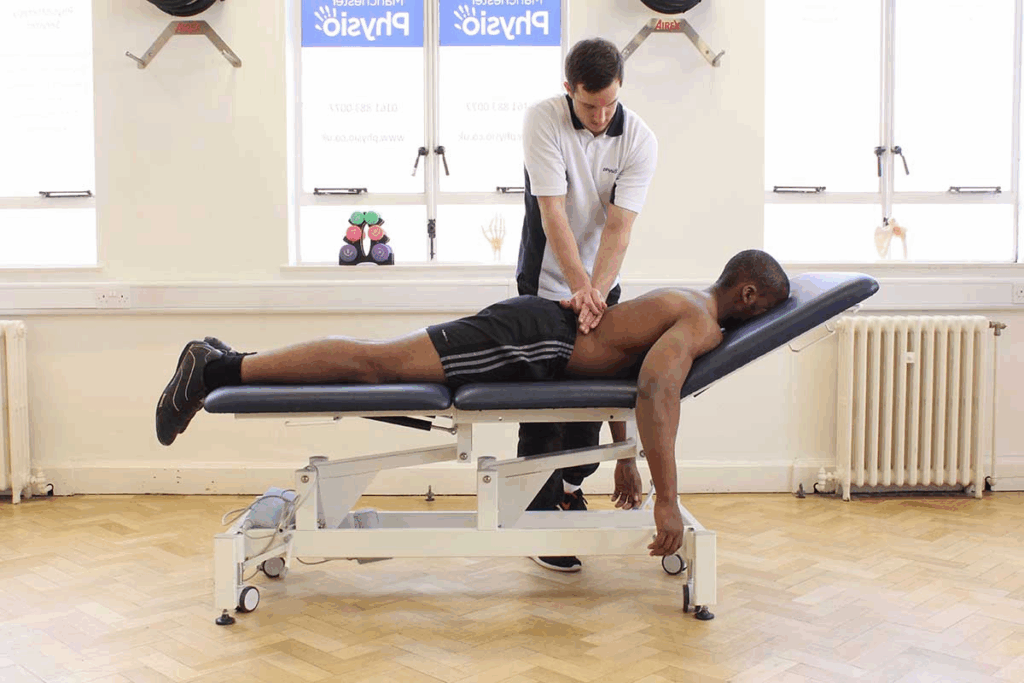
Patients recovering from heart events need cardiopulmonary physical therapy exercises. These help regain strength and improve heart health. Each exercise is tailored to meet the patient’s needs, making it a key part of cardiac rehab.
The Three Pillars: Aerobic, Strength, and Balance Training
Our exercises focus on three main areas: aerobic, strength, and balance training. Aerobic training boosts heart health. Strength training builds muscle and improves function. Balance training lowers fall risk and boosts mobility.
- Aerobic exercises include brisk walking, cycling, and swimming.
- Strength training may involve resistance bands or light weights.
- Balance exercises can include standing on one foot or using a balance board.
A typical cardiac rehab session is 35 minutes of aerobic exercise. It also includes resistance training and balance work. Suitable exercises for heart failure patients include brisk walking, cycling, swimming, and Tai Chi.
Typical Session Structure and Duration
A well-structured session is key to a successful cardiac rehab program. Sessions last 45 to 60 minutes, with warm-up and cool-down periods. The aerobic part takes about 35 minutes, with the rest for strength and balance training.
“Exercise is a celebration of what your body can do, not a punishment for what you ate.” – Unknown
Monitoring Exercise Intensity and Progress
It’s important to monitor exercise intensity to keep patients safe and effective. We use heart rate monitoring, perceived exertion scales, and symptom assessment. Regular checks help us adjust the program for better results.
- Heart rate monitoring: We track heart rate during exercise to ensure it stays within a safe range.
- Perceived exertion scales: Patients rate how hard they feel they are working.
- Symptom assessment: We monitor for any adverse symptoms during exercise.
By closely monitoring progress and adjusting the program, we maximize the benefits of cardiopulmonary physical therapy exercises for each patient.
Aerobic Exercises for Cardiovascular Strengthening
Aerobic exercises are key for cardiac rehab patients. They boost heart health, increase endurance, and improve overall well-being. We’ll look at exercises like walking, treadmill workouts, and stationary cycling for heart health.
Walking and Treadmill Exercises
Walking is a simple yet effective exercise for cardiac rehab. It’s easy on the body and can be done almost anywhere. Brisk walking is best as it raises the heart rate and boosts health without strain.
Treadmill workouts offer a controlled space for walking. They let patients track their progress and adjust the intensity. Many rehab programs use treadmills for their safety and effectiveness.
Stationary Cycling Techniques
Stationary cycling is great for cardiac rehab patients. It’s a low-impact, high-intensity workout that can be adjusted to fit each person’s fitness level. Proper technique is key to get the most benefits and avoid risks. Patients should keep their back straight, adjust the resistance, and pedal steadily.
Stationary cycling boosts heart health by raising heart rate and blood flow. It strengthens the heart and increases endurance.
Low-Impact Aerobic Alternatives
For those who find walking or cycling hard, there are low-impact options. Swimming and water aerobics are great as they work the whole body without the impact of land exercises. They’re good for patients with joint problems or mobility issues.
Other low-impact choices include elliptical trainer workouts and low-impact aerobics classes. These exercises are easy on the joints but effective for a cardiovascular workout.
Strength Training Exercises for Heart Health
Strength training is key for heart health. It boosts muscle strength and improves how well you can do daily tasks. It’s a big part of cardiac rehab.
Studies show strength training can raise VO2 peak. This is a key measure of heart health. It helps you stay strong and independent.
Upper Body Strengthening Exercises
Exercises for the upper body are important. They help you get stronger and more able. Some good ones are:
- Dumbbell shoulder press
- Bicep curls
- Tricep extensions
- Chest press (using a resistance band or light dumbbells)
You can start with light weights or bands. This makes them easy for everyone, no matter where you are in rehab.
Lower Body Strengthening Exercises
Lower body exercises are just as important. They make your legs stronger and improve balance. Good ones include:
- Squats (starting with bodyweight or assisted squats)
- Lunges
- Leg press (using a leg press machine or resistance band)
- Calf raises
These exercises not only build muscle. They also help you balance better and lower fall risks.
Adding both upper and lower body exercises to your rehab plan can really help. You’ll see big gains in strength, function, and heart health.
Balance and Flexibility Exercises in Cardiac Rehab
Balance and flexibility exercises are key in cardiac rehab. They boost mobility and lower fall risks. These exercises are vital for those recovering from heart issues, as they enhance physical function and prevent injuries. It’s important to include a variety of balance and flexibility exercises in your rehab program for the best results.
Static Balance Exercises
Static balance exercises help you stay steady while standing. Examples include standing on one foot, heel-to-toe standing, and using a balance board. These exercises strengthen your ankle muscles and improve stability. To try a simple static balance exercise, stand on one foot with the other lifted. Hold onto a chair if you need to. Stay like this for 30 seconds and then switch legs.
Dynamic Balance Training
Dynamic balance training involves movements that test your balance while walking or doing other actions. It helps you stay balanced during everyday activities. Examples include walking along a straight line, heel-to-toe walking, and single-leg squats. Dynamic balance exercises are key for better mobility and fall prevention.
Stretching and Flexibility Routines
Stretching and flexibility exercises are important for keeping your range of motion and reducing muscle tension. Examples include hamstring stretches, hip flexor stretches, and chest stretches. Regular stretching boosts flexibility and lowers muscle strain risk. We suggest adding stretching exercises to your daily routine, focusing on major muscle groups.
Combining Exercise Types for Optimal Results
To get the most out of cardiac rehabilitation, mixing aerobic, strength, and balance training is key. Cardiac rehab programs use different exercises to boost heart health.
Integrating Aerobic and Strength Training
Mixing aerobic and strength training is vital in cardiac rehab. Aerobic activities like walking or cycling boost heart health. Strength training, on the other hand, improves muscle strength and overall fitness. It’s best to switch between these or do both in one session.
Aerobic exercises should be done at a moderate pace for 30 minutes. Strength training should target big muscle groups with light to moderate weights.
Sample Combined Workout Routines
Here are some workout routines that mix different exercises:
Day | Aerobic Exercise | Strength Training | Balance/Flexibility |
Monday | 30-minute brisk walking | Upper body strength training | Static balance exercises |
Wednesday | 30-minute stationary cycling | Lower body strength training | Dynamic balance training |
Friday | 30-minute swimming or water aerobics | Core strength training | Flexibility and stretching routines |
Adjusting Exercise Combinations Based on Recovery Phase
Change the mix of exercises based on how far along you are in recovery. Early on, stick to low-intensity aerobic and gentle stretching. As you get better, add strength training and more intense aerobic exercises.
- Early recovery phase: Stick to low-intensity aerobic and gentle stretching.
- Intermediate phase: Start strength training and moderate-intensity aerobic exercises.
- Advanced phase: Try high-intensity interval training (HIIT) and tougher strength training.
Adjusting exercises based on recovery phase helps patients get the best results and improve heart health.
Progressing Through Cardiac Rehabilitation Phases
As we move through cardiac rehabilitation, it’s key to know the phases. This program helps patients recover from heart issues or surgery. It’s split into three main phases.
Early Mobilization After Cardiac Events
The first phase, early mobilization, starts right after a heart event or surgery. Patients start to move more, slowly, under watchful eyes. The main goal is to avoid problems from too much bed rest and start healing.
This phase is vital. It lays the groundwork for the next steps. Doctors guide patients to do simple exercises. These help improve blood flow, reduce stiffness, and boost physical function.
Outpatient Supervised Rehabilitation
The second phase, outpatient supervised rehabilitation, has a more set exercise plan. Patients go to a rehab center or hospital for sessions. They do aerobic, strength, and flexibility exercises made just for them.
This phase is key for better heart health, more stamina, and stronger muscles. The supervision ensures safe and effective workouts. Adjustments are made based on progress and any symptoms.
Maintenance and Long-Term Exercise Habits
The last phase, maintenance and long-term exercise habits, aims to keep up the good work. Patients are urged to keep exercising at home or in the community. The goal is to keep their heart health and fitness up.
In this phase, patients learn to manage their condition and make healthy choices. They also track their progress. The goal is to help them manage their health long-term, lowering the risk of future heart problems.
By going through these phases, patients can get the most out of cardiac rehab. They can lead a healthier, more active life.
Conclusion: Building a Lifelong Heart-Healthy Exercise Routine
Our guide on cardiopulmonary physical therapy exercises for cardiac rehab is just the start. The real journey is about keeping a healthy lifestyle for life. We urge patients to stick to a heart-healthy lifestyle even after rehab.
Adding aerobic, strength, and balance training to your routine is a big step. These exercises are key to building a strong heart for life. They help you stay healthy in the long run.
To keep a heart-healthy routine forever, keep doing the exercises you’ve learned. Slowly add more intensity and time as you get stronger. This effort will keep the benefits of rehab alive and boost your health.
FAQ
What is cardiac rehabilitation, and why is it important?
Cardiac rehabilitation is a program that helps patients recover from heart events. It includes exercise, emotional support, and lifestyle education. It’s key for improving heart health and quality of life.
What are the benefits of exercise-based cardiac rehabilitation?
This type of rehab improves heart function and reduces health risks. It boosts overall well-being and helps manage conditions like high blood pressure and diabetes.
Who should participate in cardiac rehabilitation programs?
Those who’ve had heart attacks or surgeries should join. Also, people with stable angina or heart failure can benefit.
What are the essential components of a cardiac rehabilitation program?
It includes aerobic, strength, and balance exercises. Emotional support and lifestyle education are also key. The program is tailored to each patient’s needs.
How do I prepare for cardiac rehabilitation?
Get medical clearance first. Then, assess your fitness level and set up a safe place to exercise. Make sure you have the right equipment for home workouts.
What types of exercises are beneficial for cardiovascular strengthening?
Walking, treadmill, and cycling are good for the heart. Swimming or water aerobics are low-impact options too.
How can strength training exercises improve heart health?
Strength training boosts muscle and metabolism. It also lowers blood pressure, improving heart function.
Why are balance and flexibility exercises important in cardiac rehabilitation?
They improve function and reduce fall risks. Balance and stretching routines are vital for better quality of life.
How can I combine different exercise types for optimal results?
Mix aerobic, strength, and balance exercises for best results. Adjust workouts based on your recovery and needs.
What are the different phases of cardiac rehabilitation?
There are three phases: early mobilization, outpatient rehab, and long-term exercise habits.
How can I maintain a lifelong heart-healthy exercise routine?
Keep exercising regularly and make healthy lifestyle choices. This includes a balanced diet and managing stress.
What is the best exercise for cardiac rehabilitation?
A mix of aerobic, strength, and balance exercises is best. The specific exercises and intensity depend on your needs and goals.
How often should I perform strength and balance exercises?
Do these exercises two to three times a week. Adjust frequency and intensity based on your progress and needs.
Can I do cardiac rehabilitation exercises at home?
Yes, you can do them at home with the right guidance and equipment. Home programs can be as effective as supervised ones.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11112512/