Last Updated on December 11, 2025 by Bilal Hasdemir

Carotid artery stenting vs carotid endarterectomy — understanding these two procedures is essential for anyone dealing with carotid artery stenosis. Treating this condition properly is key to avoiding strokes and protecting long-term brain health.
At Liv Hospital, we help patients learn about both carotid artery stenting and carotid endarterectomy so they can make informed decisions about their care.
Many studies show that both methods are effective in preventing strokes. However, knowing the differences between carotid artery stenting vs carotid endarterectomy can help patients and doctors choose the treatment that best fits individual health needs and risks.
Key Takeaways
- Both carotid artery stenting and endarterectomy are effective in stroke prevention.
- The choice between procedures depends on individual patient needs.
- Understanding the differences is key to making informed decisions.
- Liv Hospital offers expert care and guidance to patients.
- We focus on transparency and evidence-based practices.
Understanding Carotid Artery Disease and Treatment Options
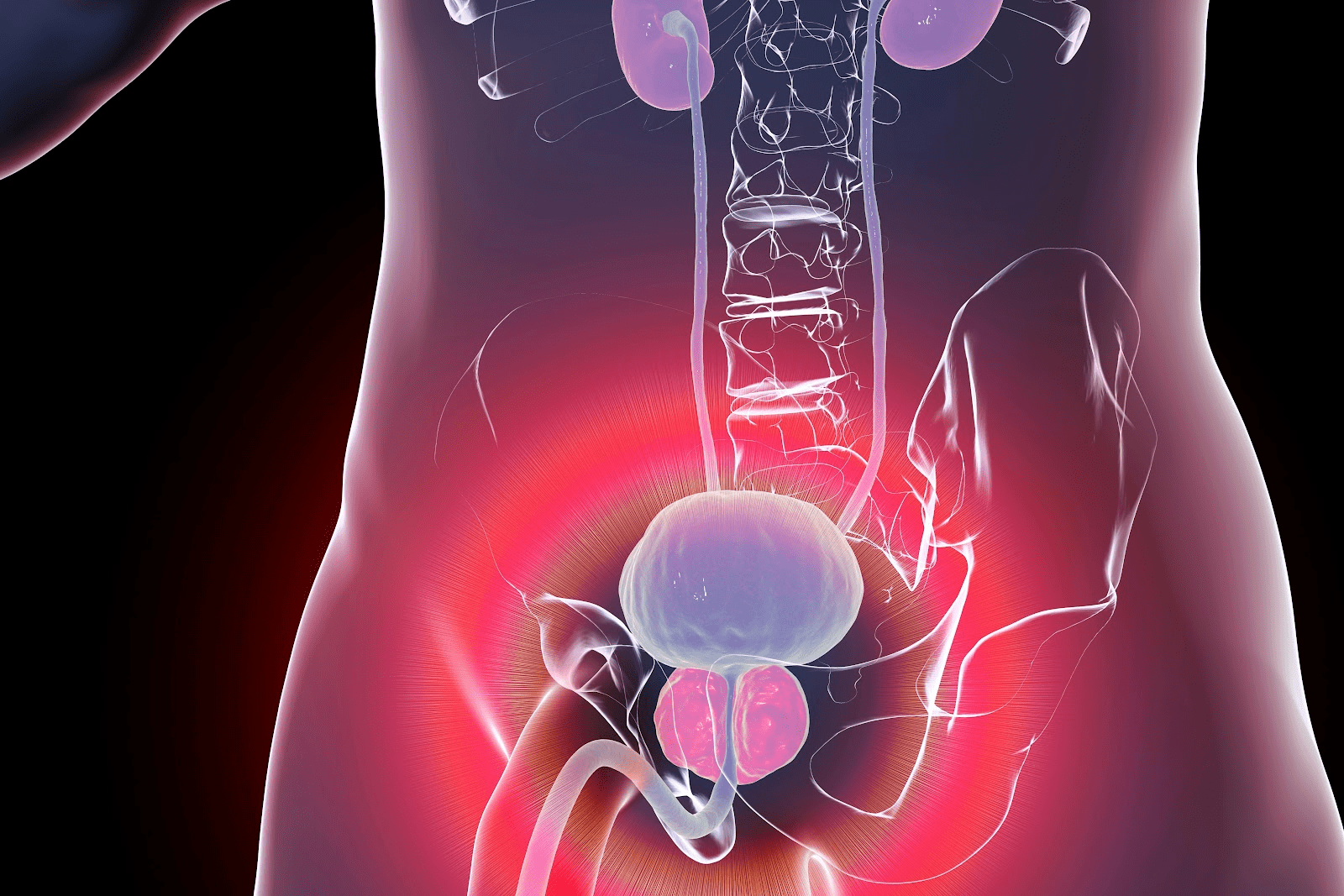
Carotid artery stenosis is a serious condition. It happens when the main blood vessels to the brain get narrowed. This narrowing can lead to a stroke if not treated.
What is Carotid Artery Stenosis?
Carotid artery stenosis is caused by plaque buildup in the carotid arteries. Plaque is a mix of cholesterol, fat, and other substances that hardens over time. This reduces blood flow to the brain.
The risk of stroke increases when this plaque ruptures. It can cause blood clots that block the artery or travel to the brain.
Knowing how severe the stenosis is is key to choosing the right treatment. Diagnostic tests like ultrasound, CT angiography, and MRI angiography help figure out the severity. They guide doctors in making treatment decisions.
The Role of Intervention in Stroke Prevention
Intervention aims to prevent strokes in people with carotid artery stenosis. Carotid revascularization can be done through carotid endarterectomy (CEA) or carotid artery stenting (CAS). The choice depends on the patient’s health, stenosis severity, and other factors.
Studies show that revascularization can lower stroke risk in the right patients. Guidelines suggest it for those with significant stenosis, provided the risk of complications is low.
Evolution of Treatment Approaches
Treatment for carotid artery stenosis has changed over time. Carotid endarterectomy was once the main treatment. Now, carotid artery stenting is also an option. Advances in technology have made both procedures safer and more effective.
Research and clinical trials continue to shape treatment choices. Doctors now consider patient-specific factors and preferences when deciding on treatment. This makes care more tailored to each patient.
Carotid Artery Stenting vs Carotid Endarterectomy: Procedural Techniques

When looking at treatments for carotid artery disease, knowing the differences between carotid artery stenting and carotid endarterectomy is key. Both methods aim to lower stroke risk by fixing carotid artery blockages. Yet, they use different approaches.
After accessing the artery, it’s clamped to stop blood flow. A temporary shunt might be used to keep the blood flowing. The surgeon then removes the plaque through an artery incision.
The artery is repaired, often with a patch to widen it and prevent future narrowing. This surgery has been a top choice for treating carotid stenosis for years.
Carotid Artery Stenting: The Endovascular Approach
Carotid artery stenting is a less invasive method. It involves placing a stent in the narrowed artery to keep it open. The procedure starts with a groin incision to access the femoral artery.
Using fluoroscopic guidance, a catheter is guided to the carotid artery. A stent is then deployed over the plaque, and angioplasty is done to expand it fully. Embolic protection devices are used to catch any debris, reducing stroke risk.
This method is seen as an alternative to endarterectomy, mainly for those at higher surgical risk or with specific anatomical features.
Patients need to understand these techniques to make informed decisions. While both methods treat carotid artery disease, the choice depends on the patient’s health, disease specifics, and personal preferences.
Difference #1: Invasiveness and Recovery Time
Carotid artery stenting and endarterectomy are two ways to treat carotid artery disease. They differ a lot in how invasive they are and how long it takes to recover. Knowing these differences helps patients make better choices about their care.
Surgical Recovery After Endarterectomy
Carotid endarterectomy is a surgery that removes plaque from the carotid artery. It needs a cut in the neck, which means a longer recovery. Patients usually need several weeks to get back to normal after surgery. They might feel pain, swelling, and bruising where the surgery was done.
Research shows that patients in the hospital for carotid endarterectomy stay from 1 to 3 days. This depends on their health and if any problems arise.
Minimally Invasive Benefits of Stenting
Carotid artery stenting, on the other hand, is a minimally invasive procedure. It uses a stent to keep the artery open. This is done through a small hole in the groin, causing less damage and a quicker recovery. Most people can go back to their usual activities in just a few days.
“Carotid stenting offers a less invasive alternative to traditional surgery, with the possibility of quicker recovery times and fewer complications.”
Hospital Stay Comparison
Looking at hospital stays for both procedures shows big differences. Here’s a table that compares the average hospital stay for carotid endarterectomy and stenting:
| Procedure | Average Hospital Stay |
| Carotid Endarterectomy | 1-3 days |
| Carotid Artery Stenting | <1 day (often outpatient) |
The table shows that carotid artery stenting usually means a shorter hospital stay. This is important for patients when they’re deciding which treatment to choose.
Difference #2: Periprocedural Risks and Complications
Choosing between carotid artery stenting and endarterectomy involves looking at risks and complications. It’s key for patients to know these to make the best choice for their care.
Stroke Risk Comparison
Stroke risk is a big worry for both methods. The International Carotid Stenting Study (ICSS) showed stenting had a higher risk of stroke, death, or heart attack than endarterectomy.
We’ll dive deeper into the stroke risk. Both methods have risks, but they are different in nature and how often they happen.
| Procedure | Stroke Risk | Myocardial Infarction Risk |
| Carotid Artery Stenting | Higher | Lower |
| Carotid Endarterectomy | Lower | Higher |
Myocardial Infarction Risk
Myocardial infarction risk is also important. Studies suggest endarterectomy might slightly increase the risk of a heart attack more than stenting.
It’s important to think about these risks based on each patient’s health and other conditions.
Procedure-Specific Complications
Each method has its own complications. Stenting might lead to stent thrombosis or restenosis. Endarterectomy could cause nerve injury or wound problems.
Knowing these complications helps in educating patients and getting their consent.
By looking at the risks and complications of both stenting and endarterectomy, we can help patients make better choices.
Difference #3: Patient Selection Criteria
Choosing between carotid artery stenting and endarterectomy depends on many factors. These include the patient’s age, symptoms, and body structure. Each factor plays a key role in deciding the best treatment for carotid artery stenosis.
Age Considerations
Age is a big factor in choosing between stenting and endarterectomy. Clinical guidelines often recommend endarterectomy for younger patients because it works well over time. For older patients, carotid artery stenting is sometimes preferred. This is because it’s safer for those with certain health issues or body features.
Symptomatic vs. Asymptomatic Patients
The choice also depends on whether the patient has symptoms. Symptomatic patients who have had a TIA or stroke might need more aggressive treatment. On the other hand, asymptomatic patients need careful evaluation to decide the best treatment.
Anatomical Factors Influencing Choice
The location and severity of the stenosis also matter. Carotid artery stenting is often chosen for patients with specific body features, like a high carotid bifurcation. For those with complex or severe stenosis, endarterectomy might be better.
| Factor | Carotid Artery Stenting | Carotid Endarterectomy |
| Age | Often considered for older patients or those with high surgical risk | Generally recommended for younger patients |
| Symptoms | Suitable for symptomatic patients with high-grade stenosis | Preferred for symptomatic patients with significant stenosis |
| Anatomical Factors | Preferred for patients with high carotid bifurcation or previous neck irradiation | More suitable for patients with complex or severe stenosis |
Difference #4: Short-term vs. Long-term Outcomes
When looking at treatments for carotid artery disease, it’s key to know the short and long-term effects. Carotid artery stenting and endarterectomy both help prevent strokes. Yet, their results vary in different ways.
30-Day Mortality and Morbidity
The first 30 days after a procedure are very important. They show how safe a treatment is. Studies say carotid artery stenting and endarterectomy have similar death rates at this time.
But the chance of having a stroke or heart attack can differ. We’ll look at these risks to understand the short-term results better.
Long-term Effectiveness in Stroke Prevention
It’s also important to know how well these treatments work over time. Research shows both methods can lower stroke risk in people with carotid artery stenosis.
Keeping the artery open and preventing it from narrowing again is key. We’ll talk about how well each method does this.
Restenosis Rates and Reintervention
Restenosis, or the artery narrowing again, is a big worry. The rates and need for more treatments differ between stenting and endarterectomy.
Knowing these differences helps patients and doctors choose the best treatment.
By looking at both short and long-term results, we can see the good and bad of each treatment. This helps improve care for patients.
Difference #5: Cost-Effectiveness and Healthcare Resource Utilization
Choosing between carotid artery stenting and carotid endarterectomy depends a lot on cost. As healthcare expenses grow, it’s key to understand the financial side of these treatments. This is important for patients, doctors, and insurance companies.
Procedural Costs Comparison
Carotid artery stenting and endarterectomy have different upfront costs. Stenting needs pricey stents and devices to prevent blockages, making it more expensive. On the other hand, endarterectomy might cost less for equipment but nrequiresa hospital and anesthesia.
A study showed stenting costs more because of the stent and protection device (1).
Length of Stay and Related Expenses
The time spent in the hospital also affects costs. Stenting is less invasive, leading to shorter stays. This means lower hospital bills.
Research found that stenting patients stay in the hospital less than endarterectomy patients (2). This shorter stay can make stenting cheaper in the short run.
Long-term Economic Impact
Looking at long-term costs, we must think about restenosis, more surgeries, and stroke prevention. Both methods have benefits, but long-term costs can differ. “The cost-effectiveness of carotid stenting versus endarterectomy over a lifetime horizon depends on several factors, including the risk of procedural complications and the cost of managing restenosis.”
“…the economic evaluation of carotid revascularization strategies should consider both short-term and long-term outcomes to accurately assess cost-effectiveness.”
It’s important to compare costs, hospital time, and long-term effects when choosing a treatment for carotid artery disease. This helps doctors make decisions that are both good for patients and the budget.
Current Clinical Guidelines and Recommendations
Current clinical guidelines are key in picking the best treatment for carotid artery stenosis. They are made from the latest research and expert opinions.
American Heart Association/American Stroke Association Guidelines
The American Heart Association (AHA) and American Stroke Association (ASA) have set guidelines for carotid artery stenosis. They focus on choosing the right treatment for each patient. Carotid endarterectomy is suggested for those with severe symptoms. On the other hand, carotid artery stenting is considered for those at high surgical risk.
European Society for Vascular Surgery Recommendations
The European Society for Vascular Surgery (ESVS) also has guidelines for carotid artery disease. These guidelines are similar to the AHA/ASA ones. They stress the importance of choosing the right treatment for each patient. The ESVS guidelines give detailed advice on when to use stenting or endarterectomy.
Evolving Evidence and Changing Practices
The field of managing carotid artery stenosis is always changing. New research and findings are constantly updating treatment options. As new evidence comes in, guidelines are updated to ensure patients get the best care.
Choosing between stenting and endarterectomy depends on many factors. These include the patient’s preferences, the condition of their arteries, and the risks of each procedure. By keeping up with the latest guidelines, doctors can tailor care to each patient’s needs.
Post-Procedure Care and Lifestyle Modifications
Carotid artery stenting and endarterectomy are just the beginning. Proper care after these procedures is key to the best results. Patients need careful management to recover well and avoid complications.
Medical Therapy After Intervention
After stenting or endarterectomy, patients get medicine to prevent stroke and heart problems. This treatment often includes:
- Antiplatelet therapy: Medications like aspirin and clopidogrel stop blood clots.
- Statins: These drugs lower cholesterol and reduce heart risks.
- Blood pressure management: Keeping blood pressure low is important to avoid stroke and heart issues.
Following the doctor’s advice on medicine is critical for the procedure’s success and heart health.
Activity Restrictions and Return to Normal Life
After the procedure, patients are told to avoid heavy lifting and bending. They also need to limit strenuous activities for a while. As they get better, they can slowly start doing normal things again, with their doctor’s okay.
Most people can get back to their usual activities in a few weeks. But this time can vary based on the person’s health and the procedure details.
Long-term Follow-up Requirements
Long-term care is important after stenting or endarterectomy. This includes:
- Regular visits to the doctor to check on their health
- Imaging tests to watch for any problems
- Managing risks like smoking, high blood pressure, and high cholesterol
By sticking to these guidelines, patients can greatly improve their long-term health and lower the chance of future heart problems.
Conclusion: Making the Right Choice for Carotid Revascularization
Choosing between carotid artery stenting and carotid endarterectomy is a big decision. It affects how well a patient does after treatment. We’ve looked at the main differences between these two options.
These differences include how the procedures are done, how invasive they are, and the risks involved. We also talked about who should get each treatment and the results in the short and long term. Plus, we looked at how much each option costs.
The choice between carotid artery stenting and carotid endarterectomy depends on many things. This includes the patient’s health, the shape of their arteries, and the skill of the doctor. Knowing the pros and cons of each option is key to making a good choice.
Healthcare providers can help patients choose the best treatment. This depends on what’s best for each person. We aim to give patients the info they need. This way, they can make choices that lead to the best results.
FAQ
What is carotid artery stenosis?
Carotid artery stenosis occurs when the main blood vessels to the brain are narrowed. This happens because of plaque buildup.
What are the treatment options for carotid artery stenosis?
There are two main treatments: carotid artery stenting and carotid endarterectomy.
What is the difference between carotid artery stenting and endarterectomy?
Carotid artery stenting is a less invasive procedure. Carotid endarterectomy is a surgery to remove plaque from the artery.
What are the benefits of carotid artery stenting?
It’s less invasive and has a shorter recovery time compared to endarterectomy.
What are the risks associated with carotid artery stenting?
Risks include stroke, heart attack, and complications specific to the procedure.
What are the benefits of carotid endarterectomy?
It’s a proven method for preventing strokes and has a long history of success.
What are the risks associated with carotid endarterectomy?
Risks include stroke, heart attack, and surgical complications.
How do I choose between carotid artery stenting and endarterectomy?
The choice depends on age, symptoms, and the anatomy of the arteries.
What are the post-procedure care and lifestyle modifications after carotid artery stenting and endarterectomy?
Patients must follow a medical therapy, adhere to activity restrictions, and attend follow-up appointments.
What are the restrictions after carotid artery surgery?
Patients should avoid heavy lifting, bending, or strenuous activities for a while.
How effective are carotid artery stenting and endarterectomy in stroke prevention?
Both methods are effective in preventing strokes. But long-term success depends on individual factors.
What is the cost-effectiveness of carotid artery stenting and endarterectomy?
Cost-effectiveness varies based on procedural costs, length of stay, and other expenses.
What are the current clinical guidelines for carotid artery stenting and endarterectomy?
Guidelines come from organizations like the American Heart Association/American Stroke Association and the European Society for Vascular Surgery.
References
- Mullen, M. T., & McGarvey, M. (2023). Carotid artery stenosis. National Library of Medicine, StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK442025/