Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 1 in 4 strokes happen because of carotid artery disease. This is when fatty deposits build up in the carotid arteries. If not treated, it can lead to a stroke.Learn at what point do they do carotid artery surgery. Understand the level of blockage that triggers the need for a carotid endarterectomy clearly.
Carotid artery surgery, or carotid endarterectomy, is a way to treat this. It removes the plaque buildup. This surgery is usually needed when the blockage is big, to lower the risk of stroke.
Whether to have carotid artery surgery depends on a few things. These include how bad the blockage is and the patient’s health.
Key Takeaways
- Carotid artery disease is a big risk for stroke.
- Carotid endarterectomy is a surgery to remove plaque buildup.
- The choice for surgery depends on the blockage’s degree and the patient’s health.
- Big blockages raise the risk of stroke.
- Surgery can lower the stroke risk in those with severe carotid artery disease.
Understanding the Carotid Artery and Its Function
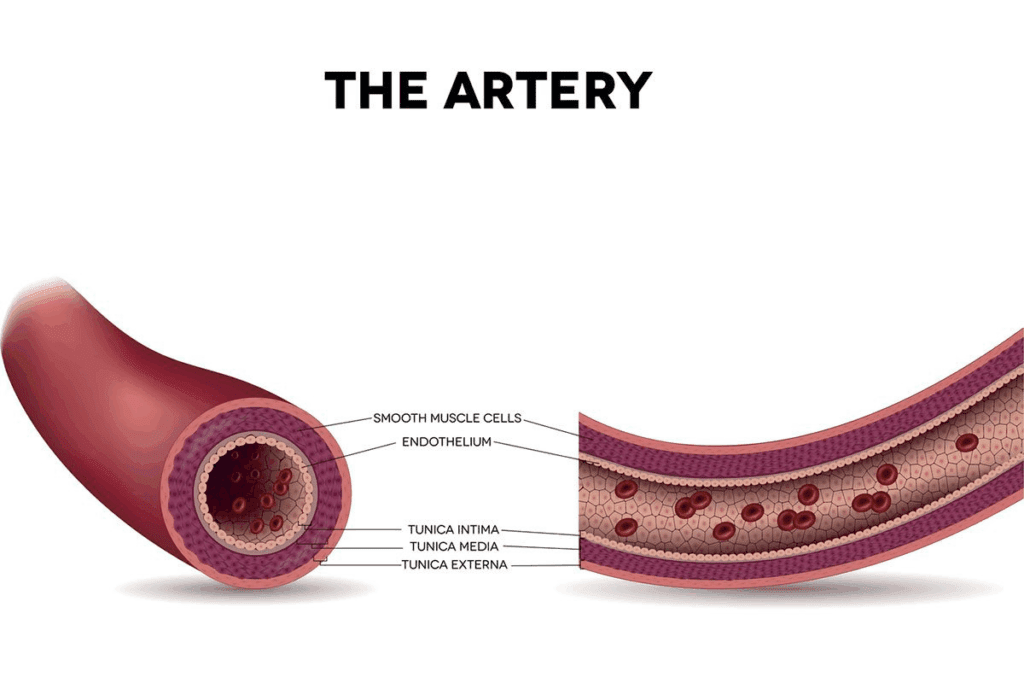
The carotid arteries are two major blood vessels. They carry oxygen and nutrients to the brain. These arteries are key for brain function and health.
Location and Anatomy of the Carotid Artery
The carotid arteries are in the neck, one on each side. They start in the chest and go up the neck. They split into the internal carotid artery and the external carotid artery.
The internal carotid artery goes straight to the brain. The external carotid artery goes to the face and neck.
Role in Blood Supply to the Brain
The carotid arteries are vital for the brain’s blood supply. The brain needs blood constantly to work right. Any problem with this supply can cause serious issues, like stroke.
Importance for Overall Brain Health
Healthy carotid arteries are key for brain health. Problems like carotid artery stenosis can raise stroke risk. It’s important to know about carotid arteries and keep them healthy.
Things that help carotid artery health include:
- Managing blood pressure
- Maintaining a healthy diet
- Exercising regularly
- Not smoking
By focusing on these, people can lower their risk of carotid artery disease. This helps keep the brain healthy.
Carotid Artery Disease: Causes and Risk Factors

It’s important to know the causes and risk factors of carotid artery disease. This knowledge helps in preventing and managing the disease. Carotid artery disease mainly happens because of plaque buildup in the carotid arteries. This process is called atherosclerosis.
Atherosclerosis and Plaque Formation
Atherosclerosis is when plaque, a mix of fat, cholesterol, and other stuff, builds up in artery walls. This buildup can narrow or block the carotid arteries. It can lead to less blood flow to the brain.
Common Risk Factors
There are several risk factors for carotid artery disease. These can be divided into two groups: modifiable and non-modifiable risk factors.
Modifiable Risk Factors
- Smoking: Smoking harms the blood vessel lining, making it easier for plaque to build up.
- High Blood Pressure: High blood pressure can damage blood vessels, raising the risk of atherosclerosis.
- Diabetes: Diabetes can speed up atherosclerosis.
- High Cholesterol: High levels of LDL cholesterol can help form plaque.
Non-modifiable Risk Factors
- Age: The risk of carotid artery disease grows with age.
- Family History: A family history of heart disease increases your risk.
- Gender: Men are generally at higher risk, but women’s risk increases after menopause.
Progression of Carotid Artery Disease
Carotid artery disease can progress slowly, over many years. It’s important to monitor and manage risk factors to prevent the disease from getting worse. Knowing the causes and risk factors helps individuals take steps to lower their risk of carotid artery disease.
Symptoms and Diagnosis of Carotid Artery Disease
It’s important to know the symptoms of carotid artery disease early. This disease often shows no signs until a stroke or TIA happens.
Warning Signs and Symptoms
The warning signs of carotid artery disease are subtle but key. They signal a high risk of stroke. Symptoms include:
- Transient ischemic attacks (TIAs) or mini-strokes
- Stroke
- Weakness or numbness in the face or limbs
- Difficulty with speech or understanding language
- Vision disturbances, including blindness in one eye
Diagnostic Methods
Several diagnostic methods help find carotid artery disease. Each method gives important info about the arteries.
Carotid Ultrasound
Carotid ultrasound is a safe test. It uses sound waves to show the arteries’ condition, helping doctors see blockages.
CT Angiography
CT angiography uses X-rays and dye to see the arteries clearly. It shows how big any blockages are.
MR Angiography
MR angiography makes detailed images with magnetic fields and radio waves. It spots narrowing or blockages in the arteries.
Cerebral Angiography
Cerebral angiography is a more invasive test. It injects dye into the arteries to see the brain’s blood vessels. It gives detailed info on any problems.
These tests are key to finding carotid artery disease. They help decide the best treatment.
Carotid Endarterectomy: Purpose and Overview
Carotid endarterectomy is a surgery to prevent stroke by removing plaque from the carotid arteries. It’s key for those with severe stenosis, a risk for stroke if untreated.
Doctors decide on this surgery after checking the patient’s stenosis level and health.
Definition and Goals of the Procedure
This surgery removes plaque from the carotid arteries. It aims to improve brain blood flow and lower stroke risk. The main goal is to clear the blockage caused by plaque.
Historical Development of Carotid Endarterectomy
Carotid endarterectomy started in the 1950s. Over time, it has seen many improvements. Better surgical methods, imaging, and patient choices have made it more effective.
Alternatives to Surgical Intervention
Carotid endarterectomy is a top choice for treating artery disease. But, there are other options too. These include carotid artery stenting and managing the condition with medicine.
Carotid Artery Stenting
Carotid artery stenting is a less invasive method. It involves placing a stent to keep the artery open. It’s often chosen for those at high surgical risk.
Medical Management Options
For some, managing the condition with medicine is best. This includes drugs for blood pressure, cholesterol, and clotting. Lifestyle changes also play a big role in reducing stroke risk.
In summary, carotid endarterectomy is a vital surgery for stroke prevention in severe stenosis cases. Knowing about it, its goals, and other options helps in making the right treatment choice.
Medical Indications for Carotid Artery Surgery
Deciding on carotid artery surgery depends on several key factors. These include the degree of stenosis and if a stroke or TIA has occurred. It’s important for both doctors and patients to understand these factors.
Degree of Carotid Stenosis
The degree of carotid stenosis is a key factor in deciding if surgery is needed. Stenosis is when the carotid artery narrows due to plaque buildup. This can reduce blood flow to the brain.
Guidelines for Asymptomatic Patients
For patients without symptoms, surgery might be considered if stenosis is severe, over 60%. But, each case is different. The decision also depends on the patient’s overall health and surgery risks.
Thresholds for Symptomatic Patients
Patients with symptoms like TIA or stroke are usually recommended for surgery if stenosis is over 50%. Symptoms mean there’s a higher risk of future strokes. Quick surgery is important to prevent more strokes.
Recent Stroke or Transient Ischemic Attack
A recent stroke or TIA is a big sign for needing carotid artery surgery. These events show the artery is blocked, raising the risk of more strokes. Surgery aims to clear the blockage and improve blood flow.
Clinical evaluation after a stroke or TIA looks at stenosis severity and the patient’s health. This helps decide if surgery is needed.
Clinical Decision-Making Process
Deciding on carotid artery surgery involves a detailed look at the patient’s condition. This includes stenosis degree, symptoms, and overall health. The decision is tailored to each patient, considering risks and benefits.
Multidisciplinary teams, like vascular surgeons and neurologists, work together. They decide if surgery is needed and what treatment is best for each patient.
In conclusion, the reasons for carotid artery surgery are complex. They involve a detailed look at stenosis, symptoms, and health status. Understanding these helps doctors make informed decisions about surgery.
Pre-Surgical Evaluation and Preparation
The pre-surgical evaluation for carotid endarterectomy is thorough. It aims to reduce risks and improve results. This step prepares patients physically and informs them about the surgery.
Comprehensive Medical Assessment
A detailed medical check-up is done to assess the patient’s health. It looks at their medical history and current health.This is key to lowering risks.
Tests like blood work, ECGs, and imaging are used. These help understand the carotid arteries better.
- Blood tests to check for clotting disorders or other conditions
- Electrocardiogram (ECG) to assess heart function
- Imaging tests like ultrasound or angiography to evaluate the carotid arteries
Medication Management Before Surgery
Managing medications before surgery is important. Some drugs may increase bleeding risks. Patients must tell their doctors about all medications, including blood thinners and herbal supplements.
| Medication Type | Pre-Surgical Action | Rationale |
| Blood Thinners | Stop or adjust dosage | Reduce risk of bleeding during surgery |
| Antiplatelet Drugs | Continue or adjust as directed | Balance risk of bleeding against risk of clot formation |
Patient Education and Informed Consent
Teaching patients about the surgery is key. They need to know the risks and recovery process. Informed consent is given after explaining the surgery’s details.
Informed consent involves:
- Understanding the purpose and nature of the procedure
- Awareness of possible risks and complications
- Knowledge of other treatment options
- Understanding the recovery and post-operative care
With a detailed pre-surgical evaluation, patients can have a safer and more successful carotid endarterectomy.
The Carotid Endarterectomy Procedure: Step by Step
Knowing the steps of carotid endarterectomy is key for those thinking about it. This surgery includes an incision in the neck, removing plaque, and fixing the artery.
Anesthesia Options and Considerations
Choosing the right anesthesia is important for carotid endarterectomy. Local anesthesia lets the patient stay awake, helping monitor their brain. General anesthesia makes the patient comfortable and helps manage their airway better.
“The choice between local and general anesthesia should be made based on individual patient needs and the surgical team’s expertise.”
Surgical Techniques
Carotid endarterectomy uses two main techniques: conventional and eversion endarterectomy.
Conventional Endarterectomy Method
This traditional method makes a long incision in the carotid artery to get to the plaque.
Eversion Endarterectomy Approach
Eversion endarterectomy flips the carotid artery to remove plaque. It’s good for some specific cases.
Intraoperative Monitoring and Safety Measures
Monitoring during carotid endarterectomy is key for safety. Tools like EEG and neurological monitoring watch for brain issues in real-time.
| Monitoring Technique | Purpose |
| EEG | Monitors brain activity |
| Neurological Monitoring | Assesses neurological function |
Closure and Completion of the Procedure
After fixing the artery, the team closes the incision. Then, the patient goes to the recovery room for care.
Understanding carotid endarterectomy helps patients prepare for the surgery and recovery.
Recovery and Post-Operative Care
Recovering from carotid artery surgery takes careful steps and precautions. After carotid endarterectomy, patients are watched closely in the hospital. They also get tips for healing at home.
Immediate Post-Surgical Care
Right after surgery, patients are checked in the recovery room for any problems. Close monitoring is key to catch and fix any issues quickly. They also get pain medicine as needed.
Hospital Stay Duration
How long a patient stays in the hospital after carotid endarterectomy varies. Most leave in 24 to 48 hours. It depends on their health and if any complications arise.
Home Recovery Guidelines
When patients go home, they get detailed recovery tips. These include:
- Resting well and avoiding hard work
- Using pain medicine as directed
- Watching the surgical area for infection signs
- Eating healthy to aid recovery
Follow-up Appointments and Monitoring
Follow-up visits are set to check on healing and watch for complications. These visits are key to adjust treatment plans as needed.
Long-term Lifestyle Modifications
To stop carotid artery disease from getting worse, patients need to make long-term lifestyle changes. These include:
- Quitting smoking
- Keeping a healthy weight
- Eating a balanced diet
- Doing regular exercise
Following these tips can greatly improve outcomes and lower the chance of future heart problems.
Conclusion
Carotid endarterectomy is a key surgery for those with carotid artery disease. It helps prevent strokes and keeps the brain healthy. This surgery removes plaque from the carotid arteries, lowering stroke risk.
Carotid artery disease often comes from atherosclerosis, causing plaque and stenosis. If not treated, it can lead to strokes or transient ischemic attacks. Carotid endarterectomy is a proven way to prevent strokes in patients with severe stenosis.
It’s important to know when surgery is needed and what happens before and after. Choosing carotid endarterectomy can greatly lower stroke risk and improve life quality.
If you have carotid artery disease, talking to a doctor is the first step. With the right diagnosis and treatment, you can manage your health and lower stroke risk.
FAQ
What is carotid endarterectomy?
Carotid endarterectomy is a surgery. It removes plaque from the carotid arteries. These arteries carry blood to the brain. The goal is to prevent stroke and improve blood flow.
What is the carotid artery?
The carotid artery is a key blood vessel in the neck. It supplies blood to the brain, face, and neck. It splits into two main branches: the internal and external carotid arteries.
What is carotid artery disease?
Carotid artery disease happens when the carotid arteries narrow or block. This is due to plaque buildup, known as atherosclerosis. It can cause stroke or transient ischemic attack (TIA).
When is carotid artery surgery recommended?
Surgery is suggested for those with severe carotid stenosis or past stroke or TIA. It aims to lower the risk of future stroke.
What are the alternatives to carotid endarterectomy?
Options include carotid artery stenting and medical management. Stenting uses a stent to keep the artery open. Medical management focuses on managing risk factors and using medications.
What is the recovery time for carotid endarterectomy?
Recovery time varies from a few days to weeks. Patients might feel discomfort, numbness, or weakness in the face or limbs.
What are the risks associated with carotid endarterectomy?
Risks include stroke, bleeding, infection, and nerve damage. Though rare, these complications can happen.
How is carotid artery disease diagnosed?
Imaging tests like ultrasound, CT angiography, or MRA diagnose carotid artery disease. They show the extent of stenosis or blockage.
What are the symptoms of carotid artery disease?
Symptoms include TIA or stroke. They can cause weakness, numbness, or paralysis in the face or limbs. Speech and vision changes are also symptoms.
Can carotid artery disease be prevented?
Some risk factors can’t be prevented. But managing high blood pressure, cholesterol, and smoking can reduce the risk.
What is carotid artery stenting?
Carotid artery stenting is a minimally invasive procedure. It places a stent in the carotid artery to improve blood flow to the brain.
What is the difference between carotid endarterectomy and carotid artery stenting?
Carotid endarterectomy removes plaque from the artery. Carotid artery stenting uses a stent to keep the artery open without removing the plaque.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31691294/