Last Updated on November 26, 2025 by Bilal Hasdemir

It’s important to know the difference between cardiac catheterization and stenting in heart disease care. At Liv Hospital, we follow advanced protocols to help our patients through these key procedures. Learn the differences between catheterization vs stent and when each heart procedure is needed.
Cardiac catheterization is mainly used to check the heart’s condition. Stenting, on the other hand, is a treatment to keep narrowed arteries open.
We understand how vital it is to know the difference between these procedures. This article will explain their differences and when to use each. It aims to help you make informed choices about your heart health.
Key Takeaways
- Cardiac catheterization is a diagnostic procedure.
- Stenting is a therapeutic intervention.
- Understanding the differences is key for heart disease care.
- Liv Hospital uses advanced protocols for these procedures.
- The choice between catheterization and stenting depends on the patient’s condition.
The Critical Role of Minimally Invasive Cardiac Procedures

Cardiovascular disease is a big problem worldwide. It has led to new ways to treat the heart without big surgeries. Finding good treatments is more important than ever.
The Global Impact of Cardiovascular Disease
Heart disease is the top killer globally, causing millions of deaths each year. The World Health Organization says heart diseases kill more people than any other. This shows we need better heart care.
Heart disease also costs a lot, with huge healthcare bills and lost work. As more people get older and risk factors like high blood pressure and diabetes rise, we’ll need more heart treatments.
Evolution of Interventional Cardiology
Interventional cardiology has changed a lot in recent years. Procedures like cardiac catheterization and angioplasty are now key treatments. They are safer than old open-heart surgeries.
New tech and methods have made these treatments better and safer. For example, better imaging lets us see the heart better. New stents help patients more after angioplasty. So, cardiac catheterization and angioplasty are key parts of heart care today, helping many heart conditions.
What Is Cardiac Catheterization?
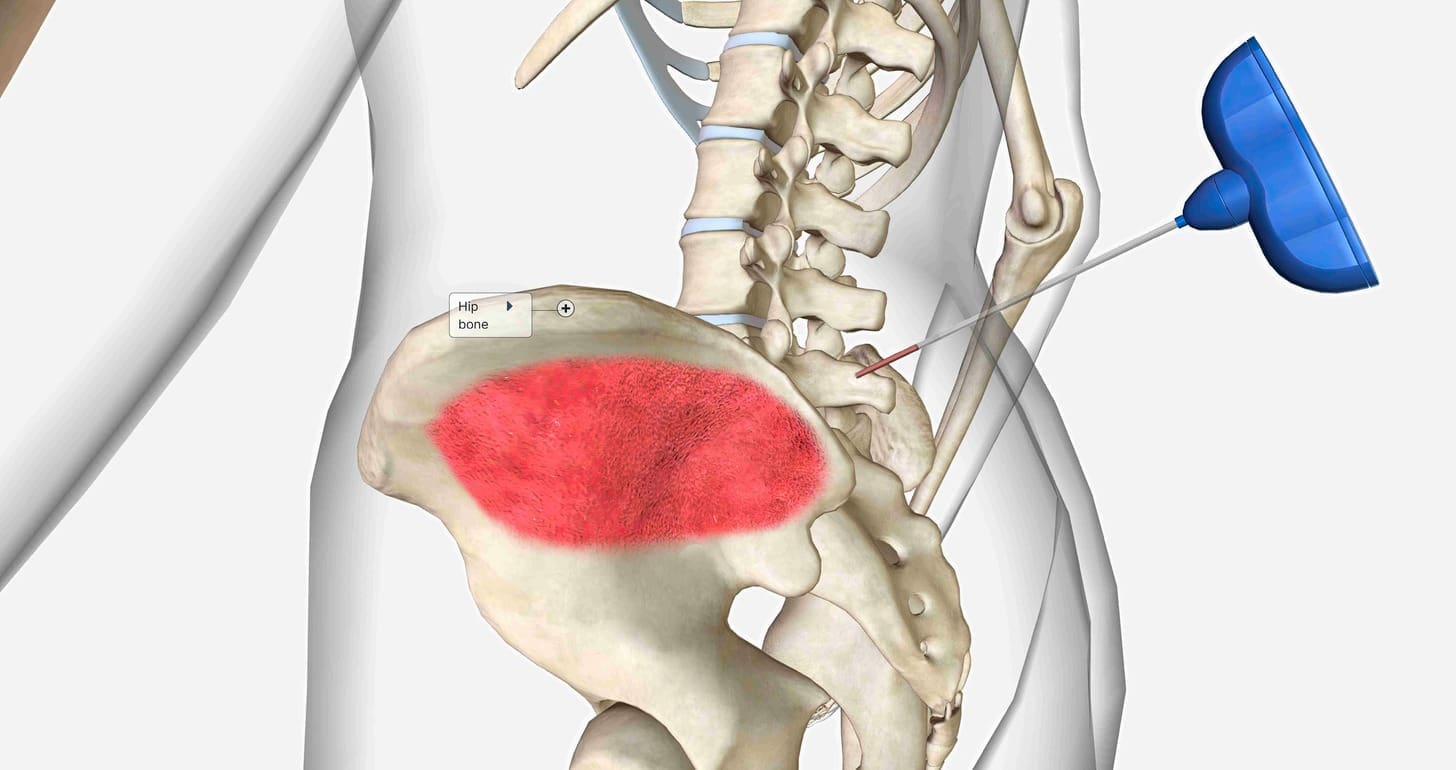
Cardiac catheterization lets doctors see inside the heart. They use a thin tube called a catheter to do this. It helps them find and fix heart problems.
Definition and Diagnostic Purpose
A catheter is put into a blood vessel in the arm or leg. It goes to the heart. This lets doctors see the heart’s arteries and find any problems.
Doctors use a special dye and X-rays to see the arteries. This helps them know how bad the heart disease is. They can then decide the best treatment.
Types of Cardiac Catheterization Procedures
There are different types of cardiac catheterization. Each one has its own purpose:
- Coronary Angiography: This is the most common type. It helps find heart disease in the arteries.
- Right Heart Catheterization: This checks the right side of the heart. It looks at pressures and oxygen levels.
- Left Heart Catheterization: This checks the left side of the heart. It looks at the left ventricle and the mitral valve.
How the Procedure Is Performed
The procedure is done in a special lab. Here’s what happens:
- The patient lies on an X-ray table. The area where the catheter goes is cleaned and numbed.
- A small cut is made, and a sheath is put into the blood vessel.
- The catheter goes through the sheath and into the heart. X-rays guide it.
- Contrast dye is used, and X-rays are taken to see the arteries.
- The catheter is taken out, and the sheath might stay in for later use.
The American Heart Association says cardiac catheterization is very helpful. It’s a way to look at and fix heart problems without a big surgery.
“Cardiac catheterization has changed cardiology. It lets doctors diagnose and treat heart disease very accurately.”
— Cardiologist
| Procedure Type | Purpose | Key Features |
| Coronary Angiography | Diagnose coronary artery disease | Visualizes coronary arteries using contrast dye |
| Right Heart Catheterization | Measure pressures and oxygen levels | Assesses right heart function |
| Left Heart Catheterization | Assess left ventricle function and mitral valve | Evaluates left heart structure and function |
What Is a Cardiac Stent?
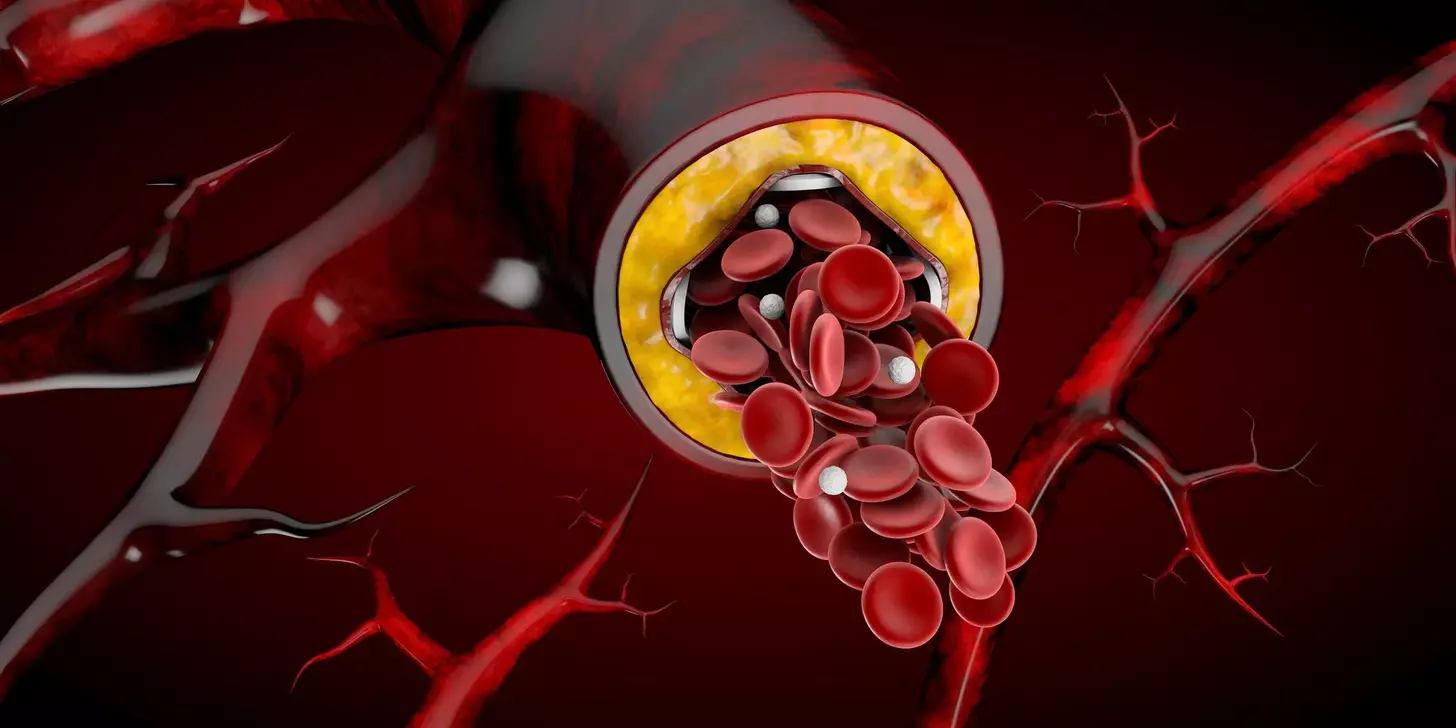
Cardiac stents are tiny, expandable tubes used to restore normal blood flow in blocked arteries. They support the artery walls and keep them open. This improves blood flow to the heart, treating coronary artery disease and preventing heart attacks.
Definition and Therapeutic Function
A cardiac stent is a small mesh tube made of metal or other materials. Its main job is to keep the artery open after an angioplasty. This ensures the artery stays unblocked, improving blood flow to the heart muscle.
The stent acts as a scaffold, supporting the artery walls. This is key for patients who have had angioplasty. It helps keep the artery open.
Types of Stents: Bare Metal, Drug-Eluting, and Bioresorbable
There are several types of cardiac stents, each with its own benefits.
- Bare Metal Stents: These are the original type. They are made of metal mesh and work by mechanically keeping the artery open.
- Drug-Eluting Stents: These stents release medication that prevents cell growth. This reduces the risk of the artery becoming blocked again.
- Bioresorbable Stents: Made from materials that dissolve over time, these stents provide temporary support. They then disappear, potentially reducing long-term complications.
The Stent Placement Procedure
The stent placement procedure usually follows an angioplasty. Here’s how it’s done:
- The cardiologist uses imaging guidance to find the blockage in the artery.
- A balloon angioplasty is done to open up the blocked area.
- The stent is then placed at the blockage site.
- The balloon is inflated to expand the stent. It is then left in place to support the artery.
In summary, cardiac stents are vital for treating coronary artery disease. They keep blocked arteries open. With different types available, cardiologists can choose the best one for each patient. Knowing the stent placement procedure helps patients understand their treatment.
Catheterization vs Stent: 7 Key Differences Explained
Cardiac catheterization and stenting are two different medical procedures. They help diagnose and treat heart problems. Both are minimally invasive but serve different purposes.
Difference 1: Primary Purpose (Diagnostic vs Therapeutic)
Cardiac catheterization is mainly for diagnosis. It lets doctors see the heart’s inner workings to find issues. Stent placement, on the other hand, is for treatment. It keeps arteries open by placing a stent.
Difference 2: Procedure Duration and Complexity
Cardiac catheterization is simpler and quicker, usually taking 30 minutes. Stent placement, which can take 60 to 90 minutes, is more complex. This depends on the case and the number of stents.
Difference 3: Materials and Devices Used
The tools used are different. Catheterization uses a thin tube, while stenting involves a stent and sometimes a balloon. The stent stays in the artery to keep it open.
Difference 4: Permanence in the Body
Another big difference is how long the devices stay in the body. Catheters are removed after use, leaving nothing behind. Stents, on the other hand, stay in the artery forever. The body gets used to them over time.
It’s important for patients and doctors to understand these differences. This knowledge helps make better choices for heart health. Each procedure has its own role in managing heart conditions.
The Relationship Between Angioplasty and Stenting
Angioplasty and stenting are key in treating heart problems. They offer a way to fix blocked arteries without surgery. Angioplasty opens up narrowed arteries. Then, stenting keeps the artery open.
What Is Balloon Angioplasty?
Balloon angioplasty opens blocked arteries or veins. A balloon is inserted and inflated to clear the blockage. This helps blood flow to the heart muscle.
A cardiologist says, “Balloon angioplasty has changed how we treat heart disease. It’s a less invasive option than surgery.”
“The use of balloon angioplasty has become a cornerstone in interventional cardiology, providing a highly effective method for treating coronary artery stenosis.”
How Angioplasty Prepares the Artery for Stenting
Angioplasty makes the artery ready for a stent. It pushes plaque against the artery walls. This makes the stent work better.
Standalone Angioplasty vs Angioplasty with Stenting
Choosing between standalone angioplasty or stenting depends on the blockage and patient health. Here are the main differences:
| Procedure | Standalone Angioplasty | Angioplasty with Stenting |
| Purpose | Widens the artery | Widens and keeps the artery open |
| Restenosis Rate | Higher | Lower |
| Long-term Outcomes | Less favorable | More favorable |
In summary, angioplasty and stenting are used together to treat heart disease. Knowing how they work together shows the progress in heart care.
Angioplasty vs Catheterization: Understanding the Distinction
Angioplasty and catheterization are used in heart treatments but in different ways. Angioplasty opens blocked arteries. Catheterization is used to see the heart and arteries.
Diagnostic vs Interventional Approaches
Catheterization is the first step to find heart disease. It uses a thin tube to see the heart. Then, angioplasty opens blocked arteries with a balloon and stent.
Key differences in their approaches include:
- Catheterization is for looking, while angioplasty is for fixing.
- Angioplasty is more complex because it includes widening the artery and stent placement.
The Procedural Pathway: From Diagnosis to Treatment
Diagnosis starts with catheterization to find blockages. If blockages are big, angioplasty might follow right away or later.
| Procedure | Purpose | Typical Next Steps |
| Catheterization | Diagnostic | Angioplasty, medication adjustment |
| Angioplasty | Therapeutic | Stent placement, follow-up care |
Patient Experience Differences Between Procedures
Patients after catheterization usually recover faster than those after angioplasty. The type of sedation and procedure complexity affect recovery.
Knowing these differences helps manage patient expectations and prepares them for what’s ahead.
Clinical Indications: When Each Procedure Is Recommended
Choosing between diagnostic catheterization and stenting depends on specific situations. We’ll look at when each is best, making sure patients get the right care.
Symptoms and Conditions Requiring Diagnostic Catheterization
Diagnostic cardiac catheterization is for those with signs of heart disease, like angina pectoris or shortness of breath. It’s also for those with abnormal stress test results or a high risk of heart disease. This procedure lets doctors see the heart’s arteries, checking for blockages or issues.
For example, someone with stable angina might get a catheterization to see how bad their heart disease is. This helps decide the best treatment, like medicine, stenting, or surgery.
When Stent Placement Becomes Necessary
Stents are needed when a big blockage is found during a catheterization and needs fixing. The choice to use a stent depends on the blockage’s size, symptoms, and heart health. Stents are often used with balloon angioplasty to keep the artery open.
In heart attacks, stenting is often used right away to get blood flowing again. The type of stent used depends on the patient’s risk of the artery closing again and their ability to take certain medicines.
Emergency Scenarios vs Elective Procedures
Cardiac catheterization and stenting can be done in emergencies or planned ahead. Emergency catheterizations are for acute heart problems or shock. Quick action is key to avoid more damage or death.
On the other hand, planned procedures are for stable heart disease. The decision to do a planned catheterization or stenting depends on the patient’s overall health, symptoms, and how well they respond to medicine.
Evidence for Medical Therapy as an Alternative
Medical therapy is a big part of treating heart disease, alongside catheterization and stenting. For some, the right medicines and lifestyle changes can manage symptoms and lower heart risk.
Research shows that for stable heart disease, the right medicines can be as good as surgery or stenting in some cases. The choice between medicine and procedures depends on the patient’s risk, symptoms, and what they prefer. This shows the importance of tailoring care to each person.
Risks and Complications: What Patients Should Know
It’s important for patients to know about the risks of cardiac catheterization and stenting. These procedures are generally safe but can have risks. Understanding these risks is key for those considering them.
Common Risks of Diagnostic Catheterization
Diagnostic cardiac catheterization helps see the heart’s inner workings. It’s safe but comes with some risks. These include bleeding, reactions to dye, and damage to blood vessels or the heart.
The chance of major problems is low but not zero. Patients might face allergic reactions, kidney issues, or even heart attack or stroke.
Potential Complications of Stent Placement
Stent placement keeps arteries open. But, it can lead to bleeding, infection, or reactions to the stent. There’s also a chance of the artery closing again or blood clots forming.
Stenting often requires taking drugs to prevent clots. This lowers clot risk but raises the chance of bleeding.
Risk Factors That Increase Complication Rates
Some factors can up the risk of problems with these procedures. These include being older, having kidney disease, diabetes, or complex heart disease.
| Risk Factor | Impact on Complication Rate |
| Older Age | Increased risk of bleeding and vascular complications |
| Chronic Kidney Disease | Higher risk of contrast-induced nephropathy |
| Diabetes | Increased risk of restenosis and complications |
Modern Approaches to Risk Reduction
Modern cardiology uses new ways to lower risks. Using radial access instead of femoral access cuts down on bleeding. Drug-eluting stents also help prevent artery closure.
Choosing the right patient, thorough checks before the procedure, and careful care after are also key. New tech and techniques make these procedures safer.
Recovery and Aftercare Following Cardiac Procedures
After cardiac catheterization or stenting, knowing the recovery process is key. This period is vital for healing and getting back to normal. It’s a time to focus on your health.
Hospital Stay Duration Expectations
The time you spend in the hospital varies. For simple catheterizations, you might go home the same day or after a night. Stenting procedures often require a longer stay, sometimes a few days, due to complications.
| Procedure | Typical Hospital Stay |
| Diagnostic Catheterization | Same day or 1 night |
| Stenting | 1-2 nights |
Activity Restrictions and Return to Normal Life
After the procedure, you’ll need to follow activity rules. Avoid heavy lifting and strenuous activities for a few days to a week. Most people get back to their usual life in a week or two.
“The key to a successful recovery is adhering to the post-procedure instructions provided by your healthcare team.”
— Cardiologist
Dual Antiplatelet Therapy After Stenting
Stenting patients often take dual antiplatelet therapy (DAPT) to prevent clots. The length of DAPT depends on the stent type and patient risk. Following the treatment plan is important to avoid complications.
Duration of DAPT: It usually lasts from 6 to 12 months. But, it can change based on your health and doctor’s advice.
Long-term Lifestyle Modifications for Heart Health
Long-term recovery means making big lifestyle changes. Eat healthy, exercise regularly, quit smoking, and manage stress. These steps are key to keeping your heart healthy and preventing future heart problems.
By focusing on recovery and aftercare, patients can greatly improve their outcomes. It’s a journey that needs patience, commitment, and support.
Latest Advances in Cardiac Catheterization and Stenting
Cardiac catheterization and stenting are getting a big boost from new technologies. These advancements are making care better and safer for patients. They also make the whole experience more comfortable.
Technological Innovations Improving Outcomes
New tech is key to better cardiac care. Some big changes include:
- Advanced Imaging Techniques: Better images help doctors place stents more accurately.
- Robotic-Assisted Procedures: Robots give doctors more control, which can lead to fewer problems and better results.
- Pressure Wire Technology: This tech helps doctors see how bad a blockage is, helping them decide the best treatment.
Biodegradable Stents and Future Directions
Biodegradable stents are a big step forward. They:
- Provide Temporary Support: They support the artery while it heals.
- Gradually Dissolve: They break down after they’re no longer needed, which could reduce long-term risks.
More research is needed to make biodegradable stents even better. Early tests look promising.
Radiation Reduction Techniques
Reducing radiation in cardiac procedures is important. It helps both patients and doctors. Ways to do this include:
- Low-Dose Protocols: Using less radiation without losing image quality.
- Advanced Shielding: Protecting everyone from radiation with new shielding.
- Real-Time Monitoring: Keeping an eye on radiation levels to cut down exposure.
Same-Day Discharge Protocols
Now, some patients can go home the same day as their procedure. This change focuses on the patient. It:
- Reduce Hospital Stay: Shorter hospital stays mean less chance of getting sick from the hospital.
- Enhance Patient Satisfaction: Being at home sooner makes patients happier and more comfortable.
- Require Careful Patient Selection: Only certain patients can go home right away to ensure they’re safe and will recover well.
As we keep improving cardiac care, these new steps will make things better for everyone. By using the latest tech, improving stents, cutting down on radiation, and making discharge easier, we’re heading towards a safer, more effective future for heart care.
Conclusion: Making Informed Decisions About Cardiac Care
It’s key for patients to know the difference between cardiac catheterization and stenting. This knowledge helps them make better choices about their heart health. We’ve looked at how these two treatments work and what they mean for patients.
Understanding these treatments lets patients talk better with their doctors. This way, they can get care that fits their needs. It makes their treatment more personal and effective.
As cardiology advances, staying up-to-date is important. We suggest patients look for trusted sources and talk to their doctors. This helps them make the best choices for their heart care.
Choosing the right heart care is a team effort. Patients, doctors, and families working together can lead to better health. This teamwork improves lives for those with heart disease.
FAQ
What is the main difference between cardiac catheterization and stenting?
Cardiac catheterization is a test to see the heart’s arteries. Stenting is a treatment to keep arteries open.
What is cardiac catheterization used for?
It’s used to find heart problems. A catheter is put into the heart. Then, contrast dye is used to see the arteries.
What are the different types of stents used in stenting procedures?
There are bare metal, drug-eluting, and bioresorbable stents. Each has its own benefits and risks.
How is a stent placed in the artery?
A stent is placed with a catheter. The catheter puts the stent in the artery. Then, it’s expanded to keep it open.
What is the difference between angioplasty and stenting?
Angioplasty uses a balloon to widen the artery. Stenting uses a stent to keep it open. Angioplasty often prepares the artery for stenting.
Can angioplasty be performed without stenting?
Yes, it can be done alone. But, it’s often used with stenting for better results.
What are the risks associated with cardiac catheterization and stenting?
Risks include bleeding and infection. There are also risks from the catheter or stent, like clotting or narrowing.
How long does recovery take after cardiac catheterization and stenting?
Recovery times vary. But, most people can get back to normal in a few days to a week. They’ll get specific advice on what to do and what not to do.
What is dual antiplatelet therapy, and why is it necessary after stenting?
It’s taking two medicines to stop platelets from sticking together. This is important to prevent clots on the stent. It’s needed for a few months to a year after stenting.
Are there any long-term lifestyle changes required after cardiac procedures?
Yes, you need to make long-term changes to stay healthy. This includes eating right, exercising, quitting smoking, and managing conditions like high blood pressure and diabetes.
What are the latest advances in cardiac catheterization and stenting?
There are new technologies, biodegradable stents, and ways to reduce radiation. There are also plans for same-day discharge. All these aim to improve patient care and experience.
What is the difference between cardiac catheterization vs angioplasty?
Cardiac catheterization is a test. Angioplasty is a treatment to widen narrowed arteries.
How does stent placement compare to cardiac catheterization?
Stent placement is a treatment after a test. It’s often done after cardiac catheterization to treat narrowed arteries.
What are the clinical indications for cardiac catheterization and stenting?
Cardiac catheterization is for diagnosing heart disease. Stenting is for treating blockages. The choice depends on symptoms, how severe the condition is, and other factors
Reference
- MedlinePlus. (2024). Angioplasty and stent placement – heart. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/007473.htm