Last Updated on December 2, 2025 by Bilal Hasdemir
CHB Medical Abbreviation MeaningCarotid artery blockage is a serious issue that can cause stroke. Carotid endarterectomy (CEA), a surgery, is often suggested for those with big blockages. About 10% to 15% of strokes are due to carotid artery disease. Studies show CEA can help those with big blockages, lowering stroke risk. Many worry about blocked carotid artery operation. But, CEA, or carotid endarterectomy, is a proven method to treat blockages in the carotid arteries. Get the definitive answer: can surgery be done on a 100% blocked carotid artery? Understand the cea medical abbreviation clearly.
Key Takeaways
- Carotid artery blockage is a serious condition that can lead to stroke.
- CEA is a surgical procedure used to remove plaque buildup in the carotid arteries.
- Research supports the benefits of CEA for patients with significant carotid stenosis.
- Approximately 10% to 15% of ischemic strokes are caused by carotid artery disease.
- CEA can potentially reduce the risk of stroke in patients with substantial blockage.
Understanding Carotid Artery Disease and Blockages

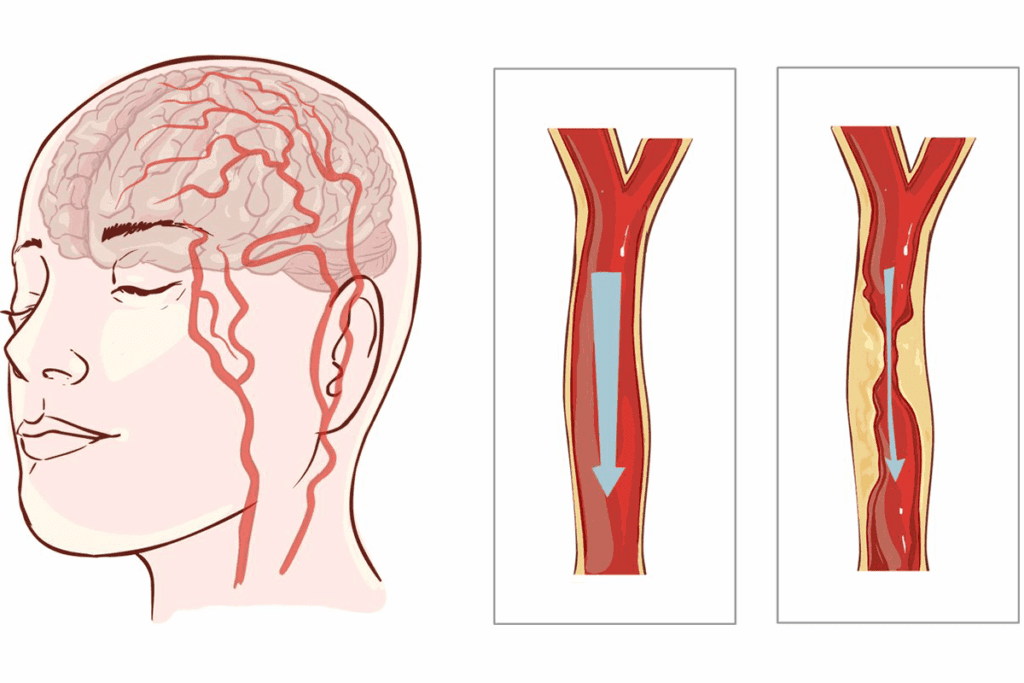
Carotid artery blockages are a big risk for stroke. It’s important to know why they happen and what they can do to your health. The carotid arteries carry blood to the brain. Any blockage or narrowing can harm your health a lot.
Anatomy of the Carotid Arteries
The carotid arteries are two big blood vessels in the neck. They bring oxygenated blood to the brain, neck, and face. They start from the aortic arch and split into the internal and external carotid arteries. The internal carotid artery goes straight to the brain. The external carotid artery goes to the neck and face.
Causes of Carotid Artery Blockage
Carotid artery blockage, or stenosis, is mainly caused by plaque buildup. This buildup is a mix of cholesterol, fat, and other substances on the artery walls. High blood pressure, smoking, high cholesterol, diabetes, and a family history of heart disease can lead to this buildup.
Progression of Carotid Stenosis to Complete Occlusion
The process of carotid stenosis turning into complete occlusion is complex and dangerous. As plaque grows, it can burst, causing blood clots. These clots can narrow or block the artery. Complete blockage can lead to a stroke or a “mini-stroke.”
| Stage | Description | Potential Consequences |
| Mild Stenosis | Less than 50% blockage | Often asymptomatic, but may require monitoring |
| Moderate Stenosis | 50-69% blockage | Increased risk of stroke, may require medical intervention |
| Severe Stenosis | 70-99% blockage | High risk of stroke, often requires surgical intervention |
| Complete Occlusion | 100% blockage | High risk of stroke, potentially life-threatening |
It’s key to understand carotid artery disease to prevent its serious effects. Knowing the causes and stages of carotid stenosis helps. This knowledge lets people work with their doctors to find the best treatments.
What is CEA (Carotid Endarterectomy)?
Carotid endarterectomy, or CEA, is a surgery to treat carotid artery stenosis. This happens when the carotid arteries, which carry blood to the brain, narrow or block due to plaque.
Definition and Purpose of the Procedure
CEA is a surgery to remove plaque from the carotid arteries. This improves blood flow to the brain and lowers stroke risk. The main goal is to widen the artery and boost blood flow. This procedure is very effective for those with severe carotid stenosis, whether they have symptoms or not. By clearing the plaque, CEA prevents strokes and improves patients’ lives.
Types of Carotid Endarterectomy Techniques
There are two main types of carotid endarterectomy: conventional and eversion endarterectomy.
| Technique | Description | Advantages |
| Conventional Endarterectomy | This involves making a longitudinal incision in the carotid artery to remove the plaque. | Allows for direct visualization and removal of plaque; widely practiced and studied. |
| Eversion Endarterectomy | In this method, the carotid artery is everted (turned inside out) to remove the plaque. | May reduce the risk of restenosis; can be less invasive in some cases. |
Both methods are chosen based on the patient’s condition, the surgeon’s preference, and other factors.
Diagnosing Carotid Artery Blockages
Diagnosing carotid artery blockages requires a mix of clinical checks and advanced imaging. It’s key to get a correct diagnosis. This helps figure out how serious the disease is and what treatment is best.
Symptoms of Carotid Artery Disease
Carotid artery disease often shows symptoms like reduced blood flow to the brain. Common carotid artery blockage symptoms include transient ischemic attacks (TIAs or “mini-strokes”), stroke, and sometimes, sounds heard over the artery with a stethoscope. Spotting these symptoms early is important for quick medical help.
Diagnostic Tests and Imaging
There are several diagnostic tests for carotid stenosis to check the carotid arteries. These include:
- Carotid Ultrasound: A non-invasive test that uses sound waves to create images of the carotid arteries, assessing blood flow and possible blockages.
- Computed Tomography Angiography (CTA): A CT scan that uses contrast dye to see the carotid arteries and measure stenosis.
- Magnetic Resonance Angiography (MRA): An MRI scan that checks blood flow and stenosis in the carotid arteries without contrast dye.
- Digital Subtraction Angiography (DSA): An invasive test seen as the top choice for diagnosing carotid stenosis, giving detailed images of the arteries.
Determining the Degree of Stenosis
The degree of stenosis is key in figuring out stroke risk and treatment. Imaging helps measure stenosis percentage. This is vital for deciding on treatment options.
| Degree of Stenosis | Description | Typical Management |
| 0-29% | Mild Stenosis | Medical Management |
| 30-69% | Moderate Stenosis | Medical Management or Carotid Endarterectomy |
| 70-99% | Severe Stenosis | Carotid Endarterectomy or Carotid Artery Stenting |
| 100% | Total Occlusion | Medical Management or Surgical Intervention |
Getting a correct diagnosis and understanding carotid artery blockages is key to preventing stroke. By knowing symptoms, using the right tests, and figuring out the stenosis degree, doctors can create effective treatment plans for each patient.
Indications for Carotid Endarterectomy (CEA)
Carotid endarterectomy is mostly suggested for patients with severe carotid stenosis, usually when the narrowing is between 70% and 99%.
It may also be considered for those with moderate stenosis (50–69%) if they have symptoms like transient ischemic attacks (TIAs) or stroke.
| Degree of Stenosis | Symptomatic Patients | Asymptomatic Patients |
| <50% | CEA not typically recommended | CEA not typically recommended |
| 50-69% | CEA considered based on individual risk factors | CEA may be considered in selected cases |
| 70-99% | CEA strongly recommended | CEA considered based on surgical risk and life expectancy |
The Surgical Process of CEA
Preoperative Preparation
Before the surgery, patients are carefully evaluated to check their overall health and anesthesia risk. Blood tests, imaging, and medication adjustments are common steps. Doctors also discuss procedure details, expected outcomes, and possible complications with patients and families.
Surgical Steps
During the procedure, an incision is made on the side of the neck where the blockage exists. The surgeon then opens the carotid artery, removes the plaque buildup, and closes it using a patch or by suturing.
The operation typically lasts 1–2 hours and is performed under general or local anesthesia depending on patient health and preference.
Postoperative Care
After the procedure, patients are moved to a recovery unit or intensive care for close monitoring. Blood pressure is controlled to prevent strain on the newly cleared artery. Most patients can return home within 1–2 days after surgery, following proper recovery instructions.
Recovery and Follow-Up After CEA
Short-Term Recovery
Immediately after surgery, some swelling or mild discomfort at the incision site is common. The hospital stay usually lasts 24–48 hours, depending on patient condition and the surgery’s complexity.
Patients are advised to avoid strenuous activities for at least two weeks and take prescribed blood-thinning medications as directed.
Long-Term Care
After discharge, long-term follow-up is essential. Follow-up ultrasound scans are often scheduled to monitor for restenosis (re-narrowing of the artery).
Lifestyle changes — such as quitting smoking, managing blood pressure, and maintaining healthy cholesterol levels — are vital to prevent future blockages.
| Recovery Phase | Timeline | Focus Areas |
| Immediate | 1–3 days | Pain management, wound care |
| Short-term | 2–4 weeks | Medication adherence, light activity |
| Long-term | 3+ months | Lifestyle modification, follow-up imaging |
Risks and Complications
While carotid endarterectomy is generally safe and effective, every surgery carries some risk.
Possible complications include bleeding, infection, nerve injury, or stroke. These risks are minimized when performed by an experienced vascular surgeon using modern techniques and technology.
Long-term outcomes are generally excellent, especially when combined with lifestyle improvements and regular follow-ups.
| Potential Complication | Frequency | Preventive Measures |
| Bleeding or hematoma | Rare | Careful surgical technique, monitoring |
| Infection | Rare | Antibiotic prophylaxis |
| Stroke | <3% in experienced centers | Proper patient selection, intraoperative monitoring |
| Nerve injury | Occasional | Precise dissection techniques |
Exercise and Lifestyle After CEA
Lifestyle changes are key to improving long-term outcomes after surgery. Regular exercise, balanced nutrition, and avoiding smoking can dramatically reduce the chance of new blockages.
| Exercise Type | Benefits | Frequency |
| Resistance Training | Improves muscle mass, bone density | 2–3 times per week |
| Weightlifting | Enhances metabolic health | 2–3 times per week |
| Bodyweight Exercises | Improves flexibility, strength | 2–3 times per week |
These activities should be approved by your healthcare provider and started gradually after full recovery.
Conclusion
Carotid endarterectomy (CEA) is a proven, effective, and safe surgical option for preventing strokes caused by carotid artery disease.
Through early diagnosis, precise surgical intervention, and long-term lifestyle management, patients can enjoy improved blood flow, reduced stroke risk, and a better quality of life.
For individuals diagnosed with carotid stenosis, consulting an experienced vascular surgeon and adopting preventive habits can make all the difference in long-term health.
FAQs
What is carotid endarterectomy?
Carotid endarterectomy is a surgery. It removes plaque from the carotid arteries. These arteries carry blood to the brain. The goal is to prevent stroke and improve blood flow.
What kind of doctor performs a carotid endarterectomy?
Doctors like vascular surgeons, neurosurgeons, and cardiac surgeons do this surgery. Vascular surgeons usually lead the way.
What are the symptoms of carotid artery disease?
Symptoms include transient ischemic attacks (TIAs) and mini-strokes. They also include stroke symptoms like weakness and numbness. Some people don’t show symptoms until a blockage is severe.
How is carotid artery disease diagnosed?
Doctors use physical exams and imaging tests like ultrasound and CT angiography. MRI angiography and angiography might also be used to check the artery’s condition.
What is the purpose of carotid endarterectomy?
The main goal is to remove plaque from the artery. This improves blood flow to the brain. It also lowers the risk of future strokes.
How do I prepare for a carotid endarterectomy?
You’ll have pre-surgery talks and adjust your meds. Stop smoking and follow your surgeon’s instructions about eating, drinking, and meds before surgery.
What happens during a carotid endarterectomy?
The surgeon makes an incision in your neck. They open the artery, remove the plaque, and then close it. You’ll be comfortable thanks to anesthesia.
What is the recovery process like after carotid endarterectomy?
You’ll get immediate care after surgery. You’ll stay in the hospital for a bit, then follow activity restrictions. You’ll also have follow-up visits to check on your healing.
What are the possible risks and complications of carotid endarterectomy?
Risks include pain, swelling, and serious issues like stroke or heart attack. Doctors work hard to avoid these problems.
Are there alternative treatments to carotid endarterectomy?
Yes, options include carotid artery stenting and medical management. Transcarotid artery revascularization (TCAR) is another choice. The best option depends on your situation.
Will insurance cover carotid endarterectomy?
In the U.S., Medicare and many private plans cover it when it’s needed. But, details and costs can vary.
What are the success rates and long-term outcomes of carotid endarterectomy?
It’s very effective in preventing stroke and improving outcomes for those with severe stenosis. Success varies based on stenosis severity and overall health.
How does carotid endarterectomy impact quality of life?
It greatly improves life by reducing stroke risk. Many patients can return to normal activities with less fear of future heart problems.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S1078588417304418





