Last Updated on November 26, 2025 by Bilal Hasdemir

A CEA vascular procedure, also known as carotid endarterectomy, is a vital surgery that cleans plaque buildup from the carotid arteries. This improves blood flow to the brain and greatly lowers the risk of stroke.
The CEA vascular procedure is considered one of the most effective treatments for carotid artery stenosis—a condition where fatty deposits narrow the arteries that supply blood to the brain. By removing this plaque, the surgery restores healthy circulation and helps prevent future strokes.
This life-saving CEA vascular procedure not only reduces stroke risk but also supports long-term brain health. For patients diagnosed with significant carotid artery narrowing, it remains a key treatment option to prevent serious complications.
At Liv Hospital, expert surgeons perform the CEA vascular procedure using advanced medical technology and safety protocols. Their focus on precision and patient care ensures optimal recovery and the best possible outcomes.
Key Takeaways
- Carotid endarterectomy removes plaque buildup from the carotid arteries.
- The surgery improves blood flow and reduces stroke risk.
- Carotid endarterectomy is effective for patients with carotid artery stenosis.
- The operation restores normal blood flow to the brain.
- Carotid endarterectomy is a proven treatment for stroke prevention.
The Critical Link Between Carotid Artery Disease and Stroke

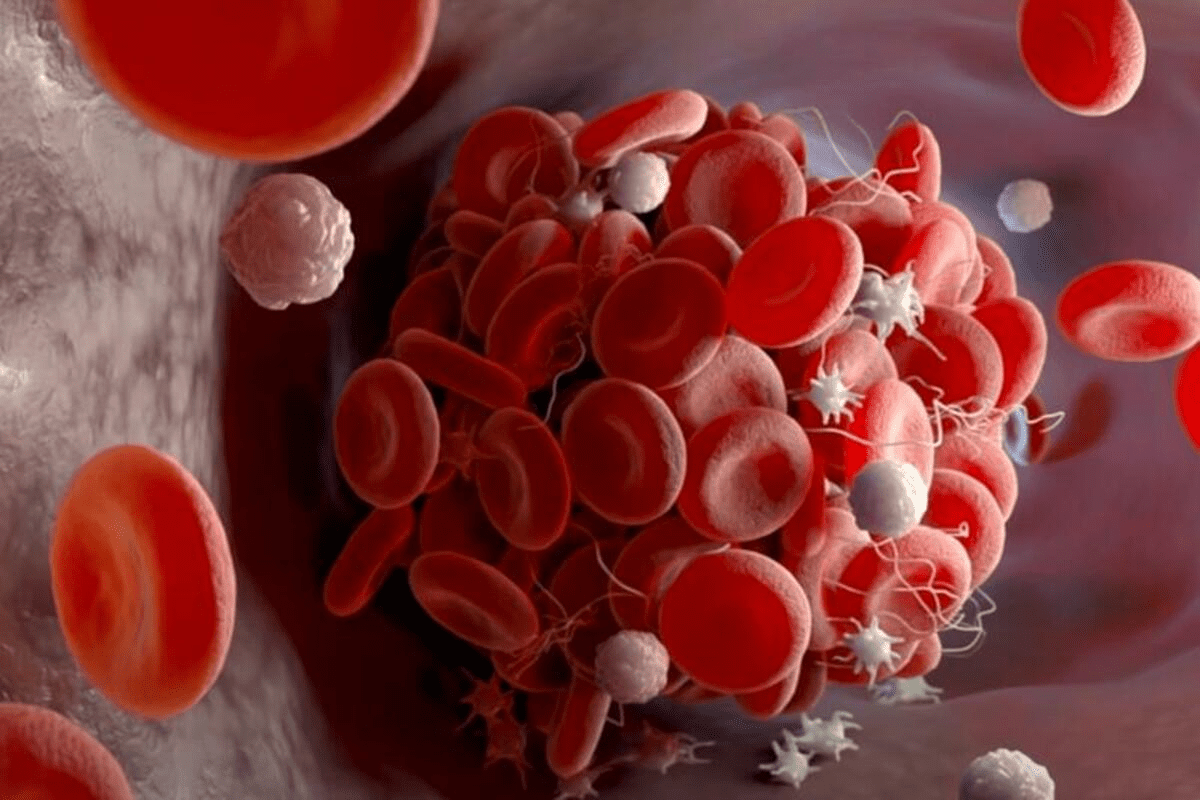
It’s important to know how carotid artery disease and stroke are connected. Carotid artery disease happens when the main blood vessels to the brain get narrowed or blocked. This is due to a buildup of plaque, a condition called atherosclerosis.
This blockage can cut down blood flow to the brain, raising the chance of stroke. The buildup of plaque in these arteries is a big risk factor for stroke. If the plaque ruptures, it can block blood flow in the brain.
How Atherosclerotic Plaque Increases Stroke Risk
Atherosclerotic plaque is made of cholesterol, fat, and calcium. Over time, it can become unstable and rupture. This releases emboli that can travel to the brain and cause a stroke.
Other factors like high blood pressure, diabetes, and smoking also increase stroke risk. The type of plaque matters too. For example, soft, lipid-rich plaques are more likely to rupture than hard, calcified ones.
Identifying High-Risk Patients for Intervention
Finding patients at high risk for stroke is key. These patients usually have a big narrowing of the artery, often over 50%.
Other signs include a history of transient ischemic attack (TIA) or stroke, symptoms like amaurosis fugax, and how much the other artery is narrowed. By spotting these high-risk patients, doctors can offer timely treatments like carotid endarterectomy to lower stroke risk.
CEA Vascular Procedure: Definition and Purpose
The CEA vascular procedure is a key surgery. It aims to clear plaque from the carotid arteries. This improves blood flow to the brain and lowers stroke risk.
Carotid endarterectomy, or CEA, is a surgery for those with narrowed carotid arteries. This narrowing is caused by plaque buildup.
Understanding Carotid Endarterectomy Meaning
“Carotid endarterectomy” means removing the diseased inner layer of the carotid artery. This surgery helps restore normal blood flow. It’s vital for those at high risk of stroke.
Key aspects of CEA include:
- Removal of atherosclerotic plaque
- Restoration of the normal carotid artery lumen
- Reduction of stroke risk
The CEA Medical Abbreviation Explained
“CEA” stands for carotid endarterectomy. It’s a term known well in medicine. Knowing this abbreviation is key for doctors and patients, as it’s a major surgery for preventing strokes.
Historical Development of the Procedure
Carotid endarterectomy started in the 1950s. It was created to treat narrowed carotid arteries. Over time, CEA has improved a lot. This is thanks to better surgery, imaging, and care for patients.
The evolution of CEA has been marked by:
- Initial development in the 1950s
- Refinements in surgical techniques over the decades
- Advances in imaging and diagnostic modalities
- Improved perioperative care and patient selection
Key Fact #1: CEA Reduces Stroke Risk by Up to 70%
Carotid Endarterectomy is a key surgery that lowers stroke risk by up to 70%. It removes plaque from the carotid arteries. This improves blood flow to the brain and cuts down stroke chances.
Clinical Evidence from Major Trials
Many big clinical trials have looked into CEA’s role in preventing strokes. The ACAS and NASCET trials are among the most important. They show CEA’s benefits for both those with and without symptoms of carotid stenosis.
These trials have helped shape how doctors treat carotid stenosis. They prove that CEA can greatly lower stroke risk when done by skilled surgeons on the right patients.
Statistical Benefits for Different Patient Groups
CEA’s benefits vary among patients. Symptomatic patients with severe stenosis see a big drop in stroke risk. Asymptomatic patients also benefit, but the risk reduction is less.
The ACAS trial found CEA cuts the 5-year stroke risk by about 50% in asymptomatic patients with 60% or more stenosis. Symptomatic patients see even bigger risk reductions, as shown by trials like NASCET.
Long-term Effectiveness Data
Long-term data on CEA’s effectiveness is key. Studies show CEA’s stroke risk reduction lasts for years. This is true if patients get good post-op care and manage their risk factors well.
Follow-up data from major trials confirm CEA’s long-term stroke prevention benefits. This makes it a valuable option for stroke prevention in certain patients.
Key Fact #2: Patient Selection Criteria for Optimal Outcomes
Picking the right patients is key for Carotid Endarterectomy success. The procedure works best when the right candidates are chosen based on certain criteria.
Symptomatic vs. Asymptomatic Carotid Stenosis
Choosing patients depends on whether they have symptoms or not. Symptomatic carotid stenosis means patients have had TIAs or strokes. On the other hand, asymptomatic carotid stenosis means no symptoms, even with artery narrowing.
Research shows CEA helps more with symptomatic stenosis. For asymptomatic patients, CEA is considered based on stenosis degree and other factors.
Degree of Artery Narrowing That Warrants Intervention
The level of artery narrowing is key for CEA. Patients with 50% or more stenosis and a history of stroke or TIA are usually recommended for surgery.
Doctors use imaging like duplex ultrasound to check artery narrowing. This helps decide if surgery is needed.
Age and Comorbidity Considerations
Age and comorbidities also matter in choosing patients for CEA. Older patients or those with many health issues face higher risks. These risks must be balanced against the surgery’s benefits.
Guidelines suggest CEA for those who might live long enough to benefit. Each case is evaluated based on the patient’s health and risks.
Key Fact #3: The Surgical Process of Carotid Artery Cleaning
The carotid endarterectomy (CEA) surgery is a detailed process. It needs careful planning and exact technique. This surgery aims to clear plaque from the carotid arteries. It helps improve blood flow to the brain and lowers stroke risk.
Preoperative Assessment and Preparation
Before CEA surgery, patients get a detailed check-up. This includes looking at their health history and doing tests like ultrasound. These steps help understand the carotid artery disease’s severity.
Doctors also work to improve the patient’s health before surgery. This might mean managing conditions like high blood pressure or diabetes. Patients are told to stop certain medications to reduce bleeding risks during the surgery.
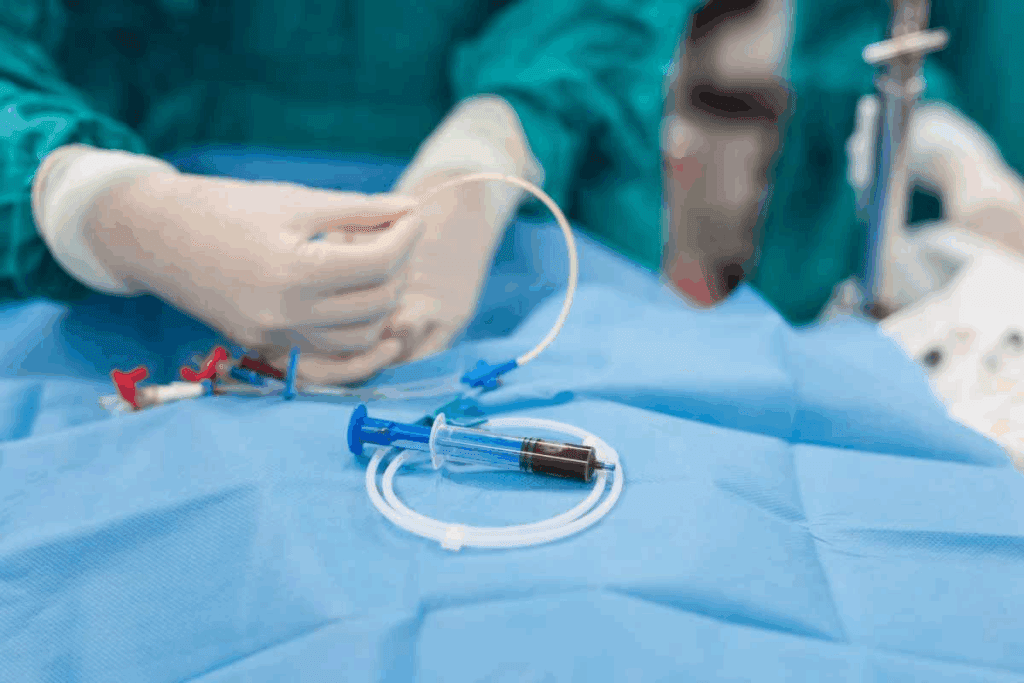
Step-by-Step Surgical Technique
The CEA surgery involves several important steps. First, the patient is given anesthesia to stay comfortable during the procedure.
The surgeon then makes a small incision in the neck. This is done to access the carotid artery without leaving big scars. The incision is planned carefully for better healing.
Next, the surgeon finds and removes the plaque from the artery. The artery is clamped to stop blood flow during this step.
An arteriotomy is made, and the plaque is removed. After making sure the artery is clean, the arteriotomy is closed. The clamps are then removed to let blood flow again.
The CEA surgery requires a lot of skill and precision. It’s done under close watch to ensure safety and success. This careful approach helps avoid complications and ensures the best results.
Key Fact #4: Left CEA and Right CEA Procedural Differences
The difference between left CEA and right CEA is more than just where they are. It affects how the surgery is done and how you might feel after. Even though the goal of CEA is the same, the details can change because of how the left and right carotid arteries are different.
Anatomical Variations Between Left and Right Carotid Arteries
The left and right carotid arteries start from different places. The right one comes from the brachiocephalic trunk. The left one usually comes from the aortic arch. This can make the surgery a bit different, mainly because of how you get to the artery.
Both arteries split into two branches at about the fourth cervical vertebra (C4). But, how and where they split can vary. This can make the surgery more or less complicated.
Surgical Approach Adaptations
Surgeons might change their approach for left and right CEA based on what they see. For example, getting to the carotid sheath might be a bit different on each side. This is because of the way the artery is positioned and the surrounding structures.
Tools like EEG or stump pressure measurement help during surgery. They make sure the brain is safe, no matter which side is being worked on.
Recovery Considerations Based on Procedure Side
Recovering from left and right CEA has some common steps, but there are differences too. For instance, the risk of nerve damage can be different on each side. This is because of how the nerves and arteries are arranged.
After surgery, doctors watch for any problems closely. They look for signs of nerve damage, bleeding, and other issues. But, the specific risks and how well you were before surgery can affect how you’re cared for after.
Key Fact #5: CEA vs. Carotid Stenting – Choosing the Right Intervention
Patients with serious carotid artery stenosis face a big decision. They must choose between CEA and carotid artery stenting. Both aim to stop strokes by improving blood flow. But they use different methods.
Comparative Effectiveness for Stroke Prevention
Research has looked at how well CEA and carotid stenting prevent strokes. CEA is seen as more effective for some patients, like those with symptoms from carotid stenosis.
The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST) found both methods work well. But, CEA might lead to heart attacks more often. Carotid stenting, on the other hand, carries a higher stroke risk.
Why CEA Is Often Safer for Patients Over 70
Age plays a big role in choosing between CEA and carotid stenting. People over 70 face more risks with carotid stenting because of their vascular anatomy and health issues.
CEA is safer for older adults. It avoids the dangers of catheter-based procedures, like embolic events.
Individualized Treatment Decision Factors
The right choice between CEA and carotid stenting depends on many factors. These include the patient’s health, the severity of their stenosis, and their anatomy.
- Symptomatic vs. asymptomatic carotid stenosis
- Degree of artery narrowing
- Presence of comorbid conditions
- Anatomical variations that may affect the feasibility of one procedure over the other
The decision should be made for each patient individually. It should consider their unique needs and preferences.
Key Fact #6: Key Risks of Carotid Artery Surgery
It’s important to know the risks of carotid artery surgery before making a decision. Carotid Endarterectomy (CEA) is a common procedure to prevent strokes. But, it comes with some complications.
Perioperative Complications
Perioperative complications happen during or right after surgery. These can include heart attacks, hyperperfusion syndrome, and strokes. The risk of stroke right after surgery is a big concern, with rates between 2-5% in some studies.
Perioperative Complication Rates
| Complication | Rate (%) |
| Myocardial Infarction | 1-2 |
| Hyperperfusion Syndrome | 1-3 |
| Perioperative Stroke | 2-5 |
Nerve Injury and Functional Impacts
Nerve injury is a possible complication of CEA. The nerves in the neck can be damaged during surgery. This can lead to problems with speech, swallowing, and facial expressions.
Most nerve injuries are temporary. But, in some cases, they can be permanent.
Restenosis: Incidence and Management
Restenosis is when the carotid artery narrows again after CEA. It happens in about 5-10% of patients within a few years. Doctors use ultrasound to monitor it and may need to do more surgery.
Mortality Risk Assessment
The risk of death from CEA is a big concern. While it’s low, less than 1%, it’s not zero. The patient’s health, other health problems, and the surgeon’s experience all play a role.
Doctors carefully evaluate each patient to understand the risks and benefits of surgery.
Key Fact #7: Recovery and Long-term Outcomes After CEA
Recovery after carotid endarterectomy is more than just the immediate time after surgery. It also includes long-term results that greatly affect a patient’s quality of life. Knowing about recovery helps manage expectations and get the best results.
Typical Hospital Stay and Immediate Recovery
Patients usually stay in the hospital for 1 to 2 nights after CEA. This time is key for watching for any problems and making sure the patient is okay before they go home. A study in the Journal of Vascular Surgery found the average stay is about 1.5 days.
| Study | Average Hospital Stay | Complication Rate |
| Journal of Vascular Surgery | 1.5 days | 2.5% |
| Stroke Journal | 1.8 days | 3.1% |
Activity Restrictions and Return to Normal Life
After leaving the hospital, patients should avoid heavy lifting and bending for a few weeks. Most can get back to normal in 1 to 2 weeks. But it’s important to follow the doctor’s advice closely for a smooth recovery.
“The key to a successful recovery after CEA is not just the surgery itself, but also the careful management of post-operative care and follow-up.”
Medical Expert in Vascular Surgery
Follow-up Protocol and Monitoring
Follow-up care is vital for checking on the patient’s recovery and catching any problems early. This includes regular visits with the vascular surgeon and possibly imaging tests to check the carotid arteries.
- Initial follow-up within 2-4 weeks post-surgery
- Regular check-ups every 6-12 months
- Imaging tests as recommended by the surgeon
Quality of Life Improvements
CEA can greatly improve a patient’s life by lowering stroke risk and improving brain blood flow. Many patients feel better and have fewer symptoms after the surgery.
Long-term results of CEA are mostly good, with a big drop in stroke risk. By understanding the recovery process and following the doctor’s advice, patients can have a successful outcome.
Post-Surgical Care: Maximizing the Benefits of CEA
Good post-surgical care is key to getting the most from Carotid Endarterectomy (CEA). It helps avoid future stroke risks. After CEA, patients need to follow a detailed care plan. This includes managing medications, making lifestyle changes, and knowing when to seek urgent medical help.
Medication Management for Ongoing Prevention
Managing medications is a big part of caring for yourself after CEA. Doctors usually give patients antiplatelet therapy to stop blood clots. This might be aspirin or clopidogrel. Taking your medicine as directed is essential to keep the artery open and prevent stroke.
Key aspects of medication management include:
- Adhering to the prescribed dosage and schedule
- Monitoring for possible side effects
- Telling your doctor about all other medicines you take
Lifestyle Modifications to Prevent Recurrence
Changing your lifestyle can help stop carotid artery disease from coming back. It also lowers stroke risk. A healthy lifestyle includes:
- Quitting smoking, as smoking is a big risk factor for carotid artery disease
- Eating a healthy diet, full of fruits, veggies, and whole grains
- Staying active, like walking or other exercises
- Keeping blood pressure and cholesterol in check through diet, exercise, and medicine if needed
Warning Signs That Require Medical Attention
It’s important for patients to know the warning signs after CEA. These signs might mean a problem:
- Sudden weakness or numbness in the face or limbs
- Difficulty speaking or understanding speech
- Sudden vision changes or loss of vision
- Severe headache or dizziness
If you notice any of these symptoms, get help right away. Quick action can make a big difference if you have a stroke or other serious issue.
Advances in CEA Techniques and Technology
Medical technology has improved carotid endarterectomy (CEA) surgeries. These changes have made CEA safer and more effective. Now, more patients can benefit from this treatment.
Minimally Invasive Approaches
One big improvement is minimally invasive CEA techniques. These methods use smaller cuts and cause less damage. This means less pain and quicker healing for patients.
The eversion method is a popular choice. It helps lower the risk of complications during surgery.
Intraoperative Monitoring Improvements
Monitoring during surgery has gotten better. Neuromonitoring and cerebral oximetry are now used. These tools help doctors check the brain’s health in real-time.
This allows for quick changes if needed. It has made surgeries safer and improved results.
Enhanced Recovery Protocols
Enhanced Recovery After Surgery (ERAS) is used in many CEA surgeries. It includes pre-op advice, better nutrition, and specific pain and anesthesia plans. The aim is to reduce stress and speed up recovery.
Studies show ERAS can cut hospital stays and boost patient happiness.
These advances in CEA have changed vascular surgery. They offer safer and more effective treatments for carotid artery disease.
Conclusion: The Enduring Value of CEA in Stroke Prevention
Carotid endarterectomy (CEA) is key for preventing strokes. It keeps getting better thanks to new techniques and tech. The term CEA is now linked with a trusted way to lower stroke risk, mainly for those with serious carotid artery blockages.
CEA’s lasting importance comes from its ability to cut down stroke risk in both those who have had symptoms and those who haven’t. It removes plaque from carotid arteries, boosting patient health and life quality.
As medical tech improves, CEA is getting safer and more effective. New, less invasive methods, better monitoring during surgery, and faster recovery plans are some of the advancements. These help CEA keep being a success in preventing strokes.
Healthcare pros can make better choices about using CEA for stroke prevention by knowing its pros and cons. This leads to better results for patients. As CEA methods and tech keep getting better, it will keep being valuable in medicine.
FAQ
What is carotid endarterectomy (CEA) and its purpose?
Carotid endarterectomy (CEA) is a surgery to remove plaque from the carotid arteries. This helps lower the risk of stroke. The term CEA stands for ‘carotid endarterectomy.’
What is carotid artery stenosis?
Carotid artery stenosis is when the carotid arteries narrow due to plaque buildup. These arteries supply blood to the brain.
How effective is CEA in reducing stroke risk?
CEA can cut the risk of stroke in half for some patients. The Asymptomatic Carotid Artery Stenosis (ACAS) trials showed a big drop in stroke risk for those with severe stenosis.
Who is recommended to undergo CEA?
People with 50% or more stenosis and a history of stroke or TIA should get CEA.
What are the differences between left and right CEA procedures?
The left and right carotid arteries split into internal and external branches. The surgery may change based on the anatomy.
How does CEA compare to carotid stenting?
Carotid stenting (CAS) is better for some patients with severe stenosis and health issues. CEA is safer for those over 70.
What are the possible risks and complications of CEA?
Risks of CEA include heart attack, stroke, nerve damage, and death. Other complications include restenosis and hyperperfusion syndrome.
What is the typical recovery process after CEA?
Patients usually stay in the hospital for a day or two. They can return to daily activities in a week or two.
What is the importance of post-surgical care after CEA?
Patients should take antiplatelet therapy and follow medication instructions. Lifestyle changes and watching for warning signs are also key.
What advances have been made in CEA techniques and technology?
CEA techniques have improved, including less invasive methods and better monitoring. Recovery protocols have also been enhanced.
What is the long-term outcome after CEA?
CEA helps prevent strokes and improves patients’ health and quality of life.
References
- Zhang, L., et al. (2015). Systematic review and meta-analysis of carotid artery stenting versus endarterectomy for carotid stenosis: A chronological and worldwide study. Medicine, 94(26), e1060. https://journals.lww.com/md-journal/fulltext/2015/07010/systematic_review_and_meta_analysis_of_carotid.41.aspx