Central Diabetes Insipidus (CDI) is a rare condition where the body can’t control fluids. This happens because of a lack of arginine vasopressin (AVP), also known as antidiuretic hormone (ADH). It’s caused by problems with making and releasing AVP.
Learn the essential management steps for central diabetes insipidus using vasopressin (Desmopressin). Understand the role of ADH effectively.
To manage CDI well, we need to know how it affects our body’s fluid balance. We also need to understand the importance of vasopressin in replacing what’s missing. Vasopressin helps control how much urine we make and keeps us from getting dehydrated.
Learning about CDI and how to treat it with vasopressin can really help patients. It can make their lives better and improve their health.
Key Takeaways
- CDI is a rare condition caused by arginine vasopressin deficiency.
- Vasopressin replacement therapy is essential for managing CDI.
- Effective management improves patient outcomes and quality of life.
- Understanding CDI’s impact on fluid balance is important.
- Vasopressin controls urine production and prevents dehydration.
What Is Central Diabetes Insipidus?
CDI, or neurogenic diabetes insipidus, is when the body can’t make enough vasopressin. This hormone is key for keeping water balance right. Vasopressin, also called antidiuretic hormone (ADH), helps control water in the body by working on the kidneys.
Definition and Terminology Evolution
Central Diabetes Insipidus is when you don’t have enough vasopressin. This makes it hard to keep fluids in balance. The name for this condition has changed over time. Now, some doctors call it “arginine vasopressin deficiency” to better describe it.
About 85% of CDI patients like this name change. They say it’s more accurate for their condition. This change shows how important clear language is in healthcare.
Key aspects of CDI include:
- Insufficient production of vasopressin
- Impaired ability to regulate body fluids
- Potential for more accurate diagnosis with evolving terminology
Prevalence and Demographics
CDI is rare, affecting a small number of people. Its prevalence varies based on the cause. Causes can range from genetics to injuries or tumors affecting the brain.
CDI can happen to anyone, but some causes are more common in certain ages. For example, genetic causes often show up in children.
Distinguishing from Diabetes Mellitus and Nephrogenic DI
Diagnosing CDI can be tricky because it’s similar to other conditions like diabetes mellitus and nephrogenic diabetes insipidus (NDI). Diabetes mellitus is about high blood sugar. CDI and NDI deal with water balance issues.
The main differences between CDI and other similar conditions are:
| Condition | Primary Issue | Key Characteristics |
|---|---|---|
| Central Diabetes Insipidus (CDI) | Vasopressin deficiency | Inability to regulate water, excessive thirst and urination |
| Diabetes Mellitus | Insulin deficiency or resistance | High blood sugar, possible ketoacidosis |
| Nephrogenic Diabetes Insipidus (NDI) | Kidney insensitivity to vasopressin | Similar symptoms to CDI, but with normal or elevated vasopressin levels |
Getting the right diagnosis is key for the right treatment. Knowing how CDI is different from other conditions helps doctors create better care plans.
Pathophysiology of Arginine Vasopressin Deficiency
Central diabetes insipidus is caused by a lack of arginine vasopressin, a hormone that helps control water in the body. This hormone, also known as antidiuretic hormone (ADH), is vital for keeping the body’s water balance right. It does this by helping the kidneys reabsorb water.
Normal AVP Function and Water Regulation
AVP is made in the hypothalamus and released by the posterior pituitary gland. It helps concentrate urine and reduce water loss by making the kidneys reabsorb more water. This process is controlled by the body’s blood osmolality and volume.
When AVP binds to its receptors in the kidneys, it starts a chain of events. This leads to more water channels in the collecting duct cells. This makes the kidneys more permeable to water, helping to reabsorb it.
Mechanisms of AVP Deficiency
In central diabetes insipidus, the lack of AVP is due to damage to the hypothalamic-pituitary axis. This damage can be from trauma, tumors, or inflammatory diseases. It disrupts AVP production, transport, or release, leading to low hormone levels.
This results in the kidneys not reabsorbing enough water. Patients with central DI then produce a lot of diluted urine. This can cause hypernatremia and dehydration if not treated properly.
Hypothalamic-Pituitary Axis Involvement
The hypothalamus and posterior pituitary gland are key in AVP regulation. Damage to these areas can cause AVP deficiency. The hypothalamus makes AVP, which is then stored and released by the posterior pituitary.
Any problem in this pathway can lead to central DI. This can be due to congenital issues, acquired conditions, or other causes.
| Condition | Effect on AVP | Clinical Outcome |
|---|---|---|
| Normal | AVP produced and released normally | Proper water balance |
| Central DI | AVP deficiency due to hypothalamic-pituitary axis damage | Polyuria, hypernatremia, dehydration |
| Nephrogenic DI | AVP produced normally but kidneys are resistant to AVP action | Polyuria, hypernatremia, dehydration |
Understanding how arginine vasopressin deficiency works is key to treating central diabetes insipidus. By knowing the causes and how AVP deficiency happens, doctors can find better ways to manage the condition. This helps improve patient care and outcomes.
Causes and Risk Factors of Central Diabetes Insipidus
Central Diabetes Insipidus can come from many causes, like genetic or acquired factors. Knowing these causes helps in diagnosing and treating the condition.
Congenital Causes
Congenital Central Diabetes Insipidus is linked to genetic mutations. These affect the production of vasopressin, or antidiuretic hormone (ADH). These genetic issues can be passed down in an autosomal dominant or recessive pattern.
Genetic Conditions Associated with CDI:
- Autosomal dominant neurohypophyseal diabetes insipidus
- Autosomal recessive neurohypophyseal diabetes insipidus
- Septo-optic dysplasia
Acquired Causes
Acquired Central Diabetes Insipidus happens when the hypothalamus or pituitary gland gets damaged. This disrupts vasopressin production or release.
Common Acquired Causes:
| Cause | Description |
|---|---|
| Brain Tumors | Tumors near the pituitary gland or hypothalamus can cause CDI by damaging vasopressin-producing neurons. |
| Surgical Interventions | Surgery in the pituitary region can lead to CDI due to damage to the vasopressin-producing cells or their pathways. |
| Traumatic Brain Injury | Head trauma can cause damage to the hypothalamic-pituitary axis, resulting in CDI. |
| Infections | Infections affecting the brain, such as meningitis or encephalitis, can lead to CDI. |
Idiopathic Central DI
In some cases, Central Diabetes Insipidus is classified as idiopathic. This means the cause is unknown. Idiopathic CDI might be due to autoimmune processes that destroy vasopressin-producing cells.
Knowing the cause of Central Diabetes Insipidus is key. It helps in choosing the right treatment and managing the condition well.
Recognizing Symptoms and Clinical Presentation
It’s important to know the signs of Central Diabetes Insipidus to get the right treatment. This condition makes it hard for the body to keep fluids because of a lack of antidiuretic hormone (ADH), also known as vasopressin.
Cardinal Symptoms
The main signs of CDI are too much thirst (polydipsia) and too much urine (polyuria). People with CDI often want to drink a lot of water. This can cause them to go to the bathroom a lot and make a lot of diluted urine.
These symptoms can really mess up daily life. Patients might have to go to the bathroom a lot during the day and night. Their urine is usually pale and diluted because their body can’t make it more concentrated.
Complications of Untreated Central DI
If CDI isn’t treated, it can cause serious dehydration and imbalances in electrolytes. Dehydration happens because the body loses too much water in urine. Electrolyte imbalances can occur because of losing important salts.
Not treating CDI can lead to even worse problems. These include:
- Severe dehydration
- Electrolyte imbalances (e.g., hypernatremia)
- Potential kidney damage due to prolonged polyuria
Quality of Life Impact
The symptoms of CDI can really affect a person’s life. Always needing to drink and go to the bathroom can be embarrassing and disrupt daily activities. It might even make people feel isolated and less productive.
It’s very important to manage CDI well to lessen these effects and improve the patient’s quality of life.
| Symptom | Description | Impact on Patient |
|---|---|---|
| Polydipsia | Excessive thirst | Increased fluid intake, frequent drinking |
| Polyuria | Excessive urine production | Frequent urination, nocturia |
| Dehydration | Excessive water loss | Potential for severe dehydration if untreated |
Diagnostic Approach and Evaluation
Diagnosing Central Diabetes Insipidus (CDI) needs a detailed process. This includes clinical checks, lab tests, and sometimes imaging. We’ll explain how to diagnose CDI and find its causes.
Clinical Assessment
The first step is a thorough clinical check. We look at the patient’s symptoms, medical history, and physical exam. Key symptoms are polyuria (too much urine) and polydipsia (too much thirst). We also check for dehydration and electrolyte imbalances.
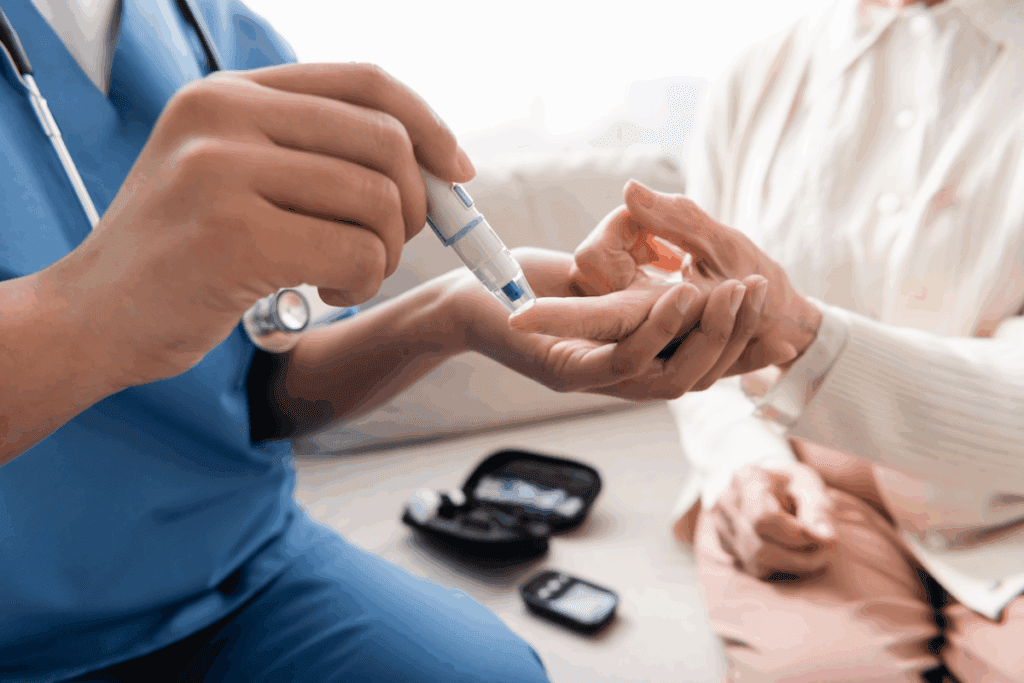
Laboratory Testing
Labs are key in diagnosing CDI. They help us:
- Check urine osmolality and specific gravity to see urine concentration.
- Look at serum osmolality and sodium levels to see hydration status.
- Do a water deprivation test to see urine concentration ability.
Water Deprivation Test Protocol
The water deprivation test is vital for CDI diagnosis. It involves:
- Not giving fluids to see urine concentration ability.
- Checking urine osmolality and serum sodium regularly.
- Using desmopressin (DDAVP) to tell CDI from nephrogenic DI.
Imaging Studies and Interpretation
Imaging, like MRI, checks the hypothalamic-pituitary area for problems. We look for tumors, diseases, or structural issues. The findings help us understand CDI’s cause and plan treatment.
In summary, diagnosing CDI needs a detailed approach. This includes clinical checks, lab tests, and imaging. By understanding this process, we can accurately diagnose CDI and its causes. This helps us manage and treat it properly.
Vasopressin Therapy: Implementation and Management
Starting vasopressin therapy is a big step in treating Central Diabetes Insipidus. It tackles the root cause of vasopressin deficiency. Desmopressin, a synthetic vasopressin, is often used as the main treatment for CDI.
Types of Vasopressin Preparations
Vasopressin treatments come in different forms to meet various needs. Desmopressin (DDAVP) is a synthetic version of vasopressin. It lasts longer and has fewer side effects than natural vasopressin.
Desmopressin comes in tablets, nasal spray, solution, and injectable forms. The choice depends on the patient’s situation, age, and what they prefer.
Desmopressin (DDAVP) Administration Routes
How desmopressin is given can affect how well it works and how easy it is for the patient to take. The options are:
- Oral tablets: Good for long-term use.
- Nasal spray: Easy and fast-acting.
- Nasal solution: Offers flexible dosing.
- Injectable forms: Used in emergencies or when other methods can’t be used.
Dosing Strategies and Titration
Desmopressin dosing is tailored to each patient. It’s all about finding the right balance to help and avoid hyponatremia.
The starting dose and any changes are based on how the patient responds. This is checked through urine output, osmolality, and serum sodium levels.
| Formulation | Initial Dose | Monitoring Parameters |
|---|---|---|
| Oral Tablets | 0.1 mg twice daily | Urine output, serum sodium |
| Nasal Spray | 10 mcg (1 spray) at bedtime | Urine osmolality, serum sodium |
| Injectable | 1-2 mcg subcutaneously or IV | Urine output, serum sodium, osmolality |
Monitoring Treatment Efficacy
It’s important to keep an eye on how well vasopressin therapy is working. This includes checking urine output, serum sodium, and osmolality.
Regular check-ups are key to seeing how the patient is doing. This helps adjust the treatment as needed.
Alternative and Adjunctive Treatment Approaches
Managing Central Diabetes Insipidus often needs a mix of treatments. Vasopressin is key for symptom control. But other treatments can tackle the underlying causes and boost patient results.
Non-Vasopressin Medications
Non-vasopressin meds can help with symptoms or underlying issues in Central Diabetes Insipidus. These include:
- Thiazide diuretics: They can surprisingly lower urine output in CDI patients.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can cut down urine production by blocking prostaglandin synthesis.
- Amiloride: Used with thiazides, it boosts their effect on reducing urine.
These drugs are helpful for those who can’t manage CDI with vasopressin alone or face vasopressin side effects.
Emerging Therapies
New treatments for Central Diabetes Insipidus are being researched. Several promising therapies are emerging:
- Gene therapy: It’s being looked into for congenital CDI caused by genetic issues.
- Stem cell therapy: Studies are checking if stem cells can fix damaged hypothalamic neurons in CDI.
- Novel vasopressin analogs: New vasopressin forms are being made to work better and have fewer side effects.
These new therapies bring hope for better treatments in the future. They aim to overcome current CDI management limits.
Addressing Underlying Causes
Treating the cause of Central Diabetes Insipidus is key when possible. This might include:
- Tumor treatment: For CDI caused by tumors, treatments like surgery, radiation, or chemotherapy might be needed.
- Managing head trauma: Proper care for head trauma is vital for CDI caused by it.
- Addressing infections or inflammatory conditions: Treating infections or inflammation that may cause CDI can help symptoms.
By tackling the root cause, we can better manage CDI and improve patient results.
Daily Management and Lifestyle Considerations
Living with Central Diabetes Insipidus (CDI) means more than just taking medicine. It’s about how you handle fluids and your lifestyle. To manage CDI well, you need to balance your fluid intake, handle special situations, and carry medical ID.
Fluid Intake Guidelines
Fluid management is key for CDI patients. Without enough antidiuretic hormone (ADH), the body can’t control fluids. This means you must watch your fluid intake to avoid dehydration or too much water.
- Check your urine output to keep it normal.
- Change how much fluid you drink based on your activity, the weather, and other factors.
- Keep a diary to track your fluid intake and output.
Managing Special Situations
CDI patients must be ready for unexpected situations. This includes getting sick, having surgery, or traveling.
| Situation | Management Strategy |
|---|---|
| Illness | Adjust desmopressin dosage as needed; monitor fluid balance closely. |
| Surgery | Tell your healthcare team about CDI; adjust medication and fluid management as needed. |
| Traveling | Bring extra medication; find out about medical facilities at your destination. |
Medical Alert Identification
It’s important for CDI patients to wear or carry medical alert ID. This way, in emergencies, doctors will know about your condition and can help you better.
Patient Education Resources
Learning about CDI is essential for managing it. Patients and caregivers should find reliable sources to understand the condition, its management, and emergency care.
- Look for trustworthy health websites and patient groups.
- Regularly talk to your healthcare team to learn about new management strategies.
- Keep a record of your medication, fluid intake, and any changes in symptoms or condition.
By following these tips and staying informed, people with CDI can live full and active lives. They can manage their condition well.
Conclusion: Optimizing Long-Term Care for Central DI
Managing central diabetes insipidus (CDI) well is key to better life quality for those affected. A full approach is needed. This includes vasopressin therapy, lifestyle changes, and regular checks.
Those with arginine vasopressin deficiency need a team effort to manage CDI well. Doctors, patient education, and a patient-centered approach are vital. Vasopressin helps control fluid balance and avoid problems.
By focusing on the patient, we can make treatment work better. Regular checks and treatment tweaks are key. With the right care, people with CDI can live full and happy lives.
FAQ
What is Central Diabetes Insipidus (CDI) and how is it different from diabetes mellitus?
Central Diabetes Insipidus (CDI) is a rare condition where the body can’t control fluids. This is because it lacks a hormone called arginine vasopressin (AVP), also known as antidiuretic hormone (ADH). It’s different from diabetes mellitus, which deals with insulin and blood sugar.
What are the symptoms of Central Diabetes Insipidus?
Symptoms of CDI include drinking a lot of water and making a lot of urine. If not treated, it can cause dehydration and imbalances in electrolytes.
How is Central Diabetes Insipidus diagnosed?
Doctors use a few methods to diagnose CDI. They look at symptoms, do lab tests, and use a water deprivation test. They also use imaging studies to find the cause.
What is the role of vasopressin in managing Central Diabetes Insipidus?
Vasopressin, or desmopressin (DDAVP), helps manage CDI. It replaces the missing AVP hormone, helping the body balance fluids.
How is vasopressin therapy administered and monitored?
Vasopressin therapy comes in different forms, like pills, nasal sprays, or injections. Doctors adjust the dose based on the patient’s needs. They check how well it’s working by looking at urine, blood tests, and symptoms.
Are there alternative treatments for Central Diabetes Insipidus beside vasopressin?
Yes, there are other treatments for CDI. These include medicines other than vasopressin and new therapies. It’s also important to treat the cause of CDI.
How can patients with Central Diabetes Insipidus manage their condition on a daily basis?
Managing CDI daily means following fluid intake rules. Patients should also know what to do in special situations. Wearing medical alert tags and using educational resources can help.
What is arginine vasopressin deficiency, and how does it relate to Central Diabetes Insipidus?
Arginine vasopressin deficiency (AVP-D) is another name for the lack of ADH hormone in CDI. It highlights the hormonal issue at the heart of the condition.
Can Central Diabetes Insipidus be cured, or is it a lifelong condition?
While some CDI cases can be well-managed, it’s often a lifelong condition. Patients need ongoing care and treatment adjustments to improve their quality of life.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9516129/