Last Updated on November 27, 2025 by Ugurkan Demir

Central sleep apnea vs OSA: A comprehensive look at the differences between Central Sleep Apnea and Obstructive Sleep Apnea.
It’s important to know the difference between central sleep apnea and obstructive sleep apnea. At Liv Hospital, we focus on treating sleep disorders well. We aim to give our patients the best care.
Obstructive sleep apnea (OSA) happens when the throat muscles relax too much during sleep. This blocks the airway. On the other hand, central sleep apnea is when the brain can’t tell the breathing muscles to work right.
Knowing the difference between these two is key to finding the right treatment. We’re all about top-notch healthcare. We also offer support for patients from around the world.
Key Takeaways
- Central sleep apnea is a neurological disorder, not caused by airway blockage.
- Obstructive sleep apnea results from physical obstruction of the airway during sleep.
- Proper diagnosis is critical for effective treatment of sleep apnea.
- Liv Hospital offers complete care for sleep disorders.
- Understanding the differences between CSA and OSA is vital for targeted treatment.
Understanding Sleep Apnea Disorders
It’s key to understand sleep apnea to tackle its health effects. Sleep apnea disorders affect breathing while sleeping. They impact heart health, brain function, and life quality.
The Prevalence and Impact of Sleep Apnea
Sleep apnea is more common than many think. Obstructive Sleep Apnea (OSA) hits about 38% of people. Central Sleep Apnea (CSA) affects about 0.9% of those over 40. Both types can harm health if not treated.
Sleep apnea’s effects go beyond bad sleep. It raises the risk of heart disease, high blood pressure, and stroke. It also causes daytime tiredness, lowers productivity, and hurts brain function. This greatly affects a person’s life quality.
The Importance of Proper Diagnosis
Getting a proper diagnosis is key. It helps figure out the sleep apnea type and plan treatment. Central sleep apnea is when breathing pauses due to lack of effort, not airway blockage.
Accurate diagnosis comes from sleep studies like polysomnography. It tells the difference between OSA and CSA. It also finds the sleep apnea cause.
Knowing the exact sleep apnea type helps doctors create the right treatment. This could be lifestyle changes, CPAP therapy, or other methods. Understanding the patient’s sleep apnea helps improve treatment and overall health.
Central Sleep Apnea vs OSA: Fundamental Differences

Central Sleep Apnea and Obstructive Sleep Apnea are two different sleep disorders. They have different causes and signs. Knowing these differences helps doctors diagnose and treat them right.
Defining Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) happens when the throat muscles relax too much at night. This blocks the airway, stopping air from getting to the lungs. It messes up breathing patterns.
Key characteristics of OSA include:
- Physical obstruction of the airway
- Relaxation of throat muscles during sleep
- Disrupted breathing patterns
The American Academy of Sleep Medicine says, “OSA is when the airway gets blocked during sleep.”
Defining Central Sleep Apnea
Central Sleep Apnea (CSA) happens when the brain can’t send the right signals to the breathing muscles. It’s not because of a blockage, but because of a brain problem.
The main features of CSA are:
- Neurological control issue
- Failure of the brain to signal breathing muscles
- Absence of physical airway obstruction
Key Distinguishing Features
The main difference between CSA and OSA is their cause. OSA is about a blockage in the airway. CSA is about a brain problem with breathing control.
Characteristics | Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) |
Cause | Physical obstruction of the airway | Neurological control issue |
Primary Mechanism | Relaxation of throat muscles | Failure of brain signals to breathing muscles |
Key Features | Disrupted breathing due to airway blockage | Disrupted breathing due to lack of brain signals |
It’s key for doctors to know these differences. This helps them diagnose and treat sleep apnea better.
The Pathophysiology of OSA
Obstructive sleep apnea (OSA) is a complex disorder. It happens when the upper airway collapses during sleep. This leads to poor sleep quality and serious health problems if not treated.
Physical Obstruction Mechanisms
The collapse of throat tissues blocks airflow in OSA. This happens because the muscles in the throat relax too much during sleep. Factors like anatomical characteristics, muscle tone, and neurological control play a role.
Risk Factors for Developing OSA
People who are heavier, have larger necks, and are older and male are more likely to have OSA. Risk factors can be divided into modifiable and non-modifiable ones. Modifiable factors include obesity, smoking, and alcohol use. Non-modifiable factors include age, gender, and genetics.
Risk Factor | Description | Modifiability |
Obesity | Increased fat around the upper airway can obstruct breathing. | Modifiable |
Age | OSA prevalence increases with age. | Non-modifiable |
Smoking | Smoking can increase inflammation and fluid retention in the airway. | Modifiable |
Gender | Males are more likely to develop OSA. | Non-modifiable |
Knowing the risk factors and how OSA works is key to treating it. Healthcare providers can help by identifying at-risk individuals and addressing modifiable factors. This leads to effective treatment plans.
The Pathophysiology of Central Sleep Apnea
Central sleep apnea happens when the brain can’t send signals to the diaphragm and other muscles needed for breathing. This causes breathing to stop for short times. It’s different from obstructive sleep apnea, which is caused by something blocking the airways. Knowing how CSA works is key to finding good treatments.
Neurological Control of Breathing
The brain controls breathing through many centers in the brainstem. The pre-Bötzinger complex is very important for making the breathing rhythm. But in CSA, this complex gets messed up, causing breathing to be irregular. The brain’s control over breathing is affected by things like CO2 levels, oxygen levels, and sleep stage.
Primary Central Sleep Apnea
Primary central sleep apnea happens without a known reason. It’s linked to idiopathic CSA, where the cause is not clear. Studies show that it might be due to problems in the brain’s breathing control centers.
Secondary Central Sleep Apnea Causes
Secondary CSA is caused by other health issues or factors. These include:
- Heart Failure: People with heart failure often have CSA, often with Cheyne-Stokes respiration.
- Neurological Disorders: Conditions like stroke, multiple system atrophy, and Parkinson’s disease can mess with breathing control.
- High-Altitude Periodic Breathing: Being at high altitudes can cause breathing patterns to change, including CSA.
- Opioid Use: Long-term use of opioids can slow down the brain’s breathing centers, causing CSA.
Knowing these causes is important for treating CSA. Treatments usually aim to fix the underlying issue causing CSA.
Clinical Presentations and Symptoms
It’s key to know the signs of OSA and CSA to help patients. We’ll look at the symptoms of each and how they show up in different ways.
Characteristic Symptoms of OSA
OSA shows up with signs of bad sleep. You might hear loud snoring, wake up a lot at night, and feel excessively sleepy during the day. People with OSA might also have morning headaches and trouble focusing because they don’t sleep well.
Characteristic Symptoms of CSA
CSA has more subtle signs, linked to breathing control. Those with CSA might wake up suddenly with shortness of breath, have breathing pauses at night, and struggle with insomnia. It can also lead to anxiety and panic disorders.
How Symptoms Differ in Clinical Settings
The signs of sleep apnea can look very different between OSA and CSA. Knowing these differences helps doctors diagnose and treat better. Here’s a table showing the main symptom differences:
Symptom | Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) |
Snoring | Common, often loud | Less common |
Awakenings | Repeated awakenings, often with choking or gasping | Sudden awakenings, sometimes with shortness of breath |
Daytime Sleepiness | Excessive daytime sleepiness common | Excessive daytime sleepiness can occur, but less consistent |
Breathing Pauses | Pauses in breathing due to obstruction | Pauses in breathing due to neurological control issues |
Understanding these differences helps doctors diagnose and treat sleep apnea better. This leads to better health outcomes for patients.
Diagnostic Criteria and Testing Methods
Diagnosing sleep apnea involves measuring the apnea-hypopnea index (AHI) through polysomnography. This method is key to figuring out how severe sleep apnea is. It also helps doctors decide on the best treatment.
Polysomnography Testing Procedures
Polysomnography (PSG) is a detailed sleep study. It tracks brain waves, eye movements, muscle activity, heart rate, and breathing. This test is usually done overnight in a lab or at home with a portable device.
During the test, several things are monitored. These include brain activity, eye movements, muscle tone, heart rate, and breathing. These help spot sleep disorders like sleep apnea by looking for breathing pauses or shallow breathing.
The Apnea-Hypopnea Index (AHI) Explained
The Apnea-Hypopnea Index (AHI) is a key number from PSG data. It shows how many times breathing stops or gets shallow per hour of sleep. The AHI shows how bad sleep apnea is.
AHI Score | Sleep Apnea Severity |
0-4 | Normal |
5-14 | Mild |
15-29 | Moderate |
30 or more | Severe |
Central Apnea Index and Other Measurements
The Central Apnea Index (CAI) counts central apneic events per hour of sleep. Central apneas happen when the brain forgets to tell the breathing muscles to work. Other important numbers include the obstructive apnea index and the mixed apnea index. They help figure out what kind of sleep apnea someone has.
Knowing these numbers is important for finding out the exact type of sleep apnea. It helps doctors create the right treatment plan.
Cheyne-Stokes Breathing Patterns
Cheyne-Stokes respiration is a breathing pattern with deep and shallow breaths. It’s often seen in people with heart failure or brain disorders. Spotting this breathing pattern is key to diagnosing and treating sleep apnea.
By using these testing methods and understanding the diagnostic criteria, doctors can make effective treatment plans. This helps improve patient outcomes.
Treatment Approaches for OSA
Managing Obstructive Sleep Apnea (OSA) requires different treatments for each person. We’ll look at various options, from devices to lifestyle changes, to help those with OSA manage their condition well.
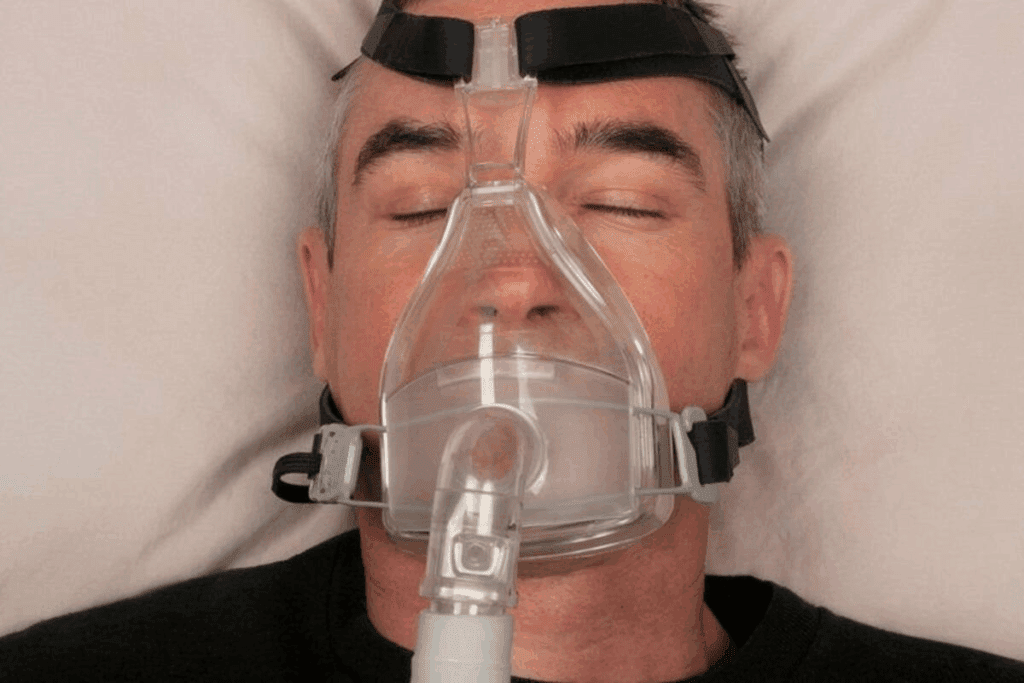
CPAP and Other Positive Airway Pressure Therapies
Continuous Positive Airway Pressure (CPAP) therapy is a common treatment for OSA. It uses a mask over the nose and/or mouth connected to a machine. This machine delivers air to keep the airway open. CPAP therapy is highly effective in reducing apneic events and improving sleep quality.
Other positive airway pressure therapies include BiPAP and APAP. These offer different pressure levels to make treatment more comfortable and effective.
CPAP therapy is often the first choice for moderate to severe OSA. But, some people find it hard to use because of discomfort or claustrophobia. Advancements in CPAP technology, such as heated humidification and mask design improvements, have enhanced user comfort and adherence.
Oral Appliances and Surgical Options
For those who can’t use CPAP or have mild OSA, oral appliances are a good option. These custom-made devices help keep the airway open during sleep. Oral appliances are useful for patients with mild to moderate OSA or those who prefer a less invasive treatment.
Surgical options are for severe OSA cases that haven’t responded to other treatments. Procedures like uvulopalatopharyngoplasty (UPPP) or genioglossus advancement aim to remove or reposition tissue. These surgeries aim to remove or reposition tissue that obstructs the airway, reducing apneic events.
Lifestyle Modifications and Weight Management
Lifestyle changes are key in managing OSA. Losing weight is often recommended for those who are overweight or obese. A healthy diet and regular exercise not only aid in weight management but also improve overall sleep quality and reduce the severity of OSA.
Other lifestyle changes include avoiding alcohol and sedatives before bedtime, sleeping on one’s side instead of back, and quitting smoking. These changes can significantly impact the severity of OSA and improve treatment outcomes. By adopting a complete treatment plan, individuals with OSA can manage their condition and improve their quality of life.
Treatment Approaches for Central Sleep Apnea
Dealing with central sleep apnea (CSA) needs a mix of strategies. It’s not just about treating symptoms. We also need to find and fix the root causes. “The key to successful treatment lies in understanding the complex interplay between CSA and associated medical conditions,” say sleep experts.
Addressing Underlying Medical Conditions
First, we tackle any health issues that might be causing CSA. This could mean better managing heart failure or stopping opioid use. Fixing these problems can really help with CSA symptoms.
Key strategies include:
- Optimizing treatment for heart failure or other cardiovascular diseases
- Adjusting or discontinuing opioid medications under medical supervision
- Managing neurological conditions that may affect breathing
Medication Management Strategies
Sometimes, medicine is needed to manage CSA. Acetazolamide, for example, can help reduce apneas. But, we always tailor the treatment to each patient and watch it closely.
“Pharmacological interventions can play a critical role in managing CSA, when underlying conditions are well-controlled.” – Sleep Medicine Expert
Advanced Therapies: ASV and Phrenic Nerve Stimulation
For severe CSA, we might use advanced treatments. Adaptive Servo-Ventilation (ASV) helps keep breathing steady during sleep. Phrenic nerve stimulation involves a device that helps control breathing by stimulating the diaphragm.
ASV therapy is great for complex sleep apnea or when other treatments fail. Phrenic nerve stimulation is a more invasive but effective option for some patients.
By using these treatments together, we can give better care to those with CSA. This improves their life quality and lowers the risk of complications.
Complications and Long-term Health Consequences
Untreated sleep apnea can harm your health a lot. It can cause heart and metabolic problems. We will look at the long-term effects, like heart and metabolic issues, and how it affects your brain and daily life.
Cardiovascular and Metabolic Impacts
Sleep apnea can lead to heart disease. The breathing stops and starts, which can hurt your heart. This can cause hypertension, heart failure, and a higher risk of stroke.
It also raises the risk of metabolic syndrome. This includes high blood pressure, high blood sugar, and more. These conditions increase the risk of heart disease, stroke, and type 2 diabetes.
Sleep apnea can also make it hard to control blood sugar. This is because it disrupts sleep and lowers blood oxygen. This can lead to insulin resistance and type 2 diabetes.
Neurological and Quality of Life Effects
Sleep apnea can also hurt your brain. It can make it hard to focus, remember things, and make decisions. It can also cause depression and anxiety, which can really affect your life.
Living with sleep apnea can be tough. People often feel fatigued and sleepy during the day. This can make it hard to do everyday things and can hurt your work and personal life.
It’s important to know about these risks if you have sleep apnea. Working with your doctor can help manage the condition. This can reduce the chance of these serious health problems.
Conclusion: Navigating Diagnosis and Treatment Options
It’s key to know the difference between central and obstructive sleep apnea for better management. Getting a correct diagnosis is the first step. Treatment plans vary a lot between these two conditions.
Healthcare providers can create specific treatment plans by understanding each type’s unique traits. For obstructive sleep apnea, treatments might include CPAP therapy, oral appliances, and changes in lifestyle. Central sleep apnea, on the other hand, might need treatments for underlying health issues, medications, or advanced therapies like adaptive servo-ventilation.
Getting the right diagnosis and treatment can greatly improve life for those with sleep apnea. Good management not only boosts quality of life but also lowers risks of heart and metabolic problems. As sleep medicine advances, the need for personalized care in diagnosis and treatment grows.
FAQ
What is the main difference between central sleep apnea and obstructive sleep apnea?
Central sleep apnea happens when the brain can’t send the right signals to the breathing muscles. On the other hand, obstructive sleep apnea is caused by something blocking the airway.
What is central sleep apnea etiology?
Central sleep apnea’s cause is linked to how the brain controls breathing. It can be due to primary or secondary reasons, including other health issues.
How is central sleep apnea diagnosed?
Doctors use polysomnography testing to diagnose central sleep apnea. They also look at the central apnea index and other criteria.
What is the difference between central apnea index and apnea-hypopnea index?
The central apnea index counts central apneas per hour. The apnea-hypopnea index, on the other hand, counts all apneas and hypopneas per hour, including both types.
What are the treatment approaches for central sleep apnea?
Treatments for central sleep apnea include treating underlying health issues and using medications. Advanced therapies like adaptive servo-ventilation (ASV) and phrenic nerve stimulation are also used.
How does obstructive sleep apnea differ from central sleep apnea in terms of symptoms?
Obstructive sleep apnea often causes loud snoring and breathing pauses. Central sleep apnea might have less typical symptoms, like insomnia or morning headaches.
What are the potentially serious complications of untreated sleep apnea?
Untreated sleep apnea can harm the heart and metabolism. It can also affect the brain and quality of life, increasing the risk of heart disease and lowering cognitive function.
What is Cheyne-Stokes breathing pattern?
Cheyne-Stokes breathing is a pattern of breathing with cycles of deep and shallow breaths. It’s often seen in central sleep apnea and other health issues.
Can lifestyle modifications help manage sleep apnea?
Yes, making lifestyle changes like losing weight, exercising regularly, and avoiding sedatives can help manage sleep apnea, mainly obstructive sleep apnea.
What is the role of CPAP therapy in treating obstructive sleep apnea?
CPAP therapy is a common treatment for obstructive sleep apnea. It keeps the airway open and prevents breathing pauses during sleep.
References
- Morgenthaler, T. I., Kagramanov, V., Hanak, V., & Decker, P. A. (2006). Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep, 29(9), 1203-1209. https://academic.oup.com/sleep/article/29/9/1203/2708343





