We are seeing a big change in treating brain aneurysms and vascular disorders. This change comes with minimally invasive endovascular procedures. One such advanced method is brain embolization. It aims to block abnormal or problematic blood vessels in the brain.
This new procedure helps treat many conditions. These include brain aneurysms, arteriovenous malformations (AVMs), and tumors. It does so with several benefits. These include shorter recovery times and less trauma to the patient.
Key Takeaways
- Minimally invasive procedure for treating brain aneurysms and vascular disorders.
- Blocks abnormal or problematic blood vessels in the brain.
- Used to treat conditions such as brain aneurysms, AVMs, and tumors.
- Offers benefits like shorter recovery times and less trauma.
- Cutting-edge technique with international standards and patient-centered care.
Understanding Cerebral Embolization: Definition and Purpose
Cerebral embolization is a cutting-edge medical procedure. It has changed how we treat brain problems. This method uses materials like coils to stop blood flow in specific brain areas.
What Exactly Is Cerebral Embolization?
Cerebral embolization, or endovascular embolization, is a precise procedure. An expert uses a catheter to place embolic materials in the brain’s blood vessels. The aim is to block blood flow to certain areas, treating brain issues.
Key Conditions Treated with This Procedure
This procedure helps with many conditions, like brain aneurysms and tumors. It stops the blood flow to these problems. This can prevent rupture, lessen symptoms, and improve health outcomes.
| Condition | Description | Treatment Goal |
| Brain Aneurysm | A weak or thin spot on an artery wall that can rupture | Prevent rupture by occluding the aneurysm |
| Arteriovenous Malformation (AVM) | Abnormal connection between arteries and veins | Reduce blood flow to the AVM, preventing hemorrhage |
| Tumors | Certain types of brain tumors require reduced blood flow | Decrease tumor size and reduce symptoms |
Evolution of Endovascular Techniques
The field of endovascular embolization has grown a lot. New materials and better catheters have made it safer and more effective. Now, it’s a key part of treating brain problems, a less invasive option than surgery.
It can be used alone or with other treatments like radiosurgery. This gives a full approach to managing complex brain conditions.
The Science Behind Brain Embolization

Brain embolization is a medical procedure that blocks blood vessels to treat neurovascular conditions. It works by using precise embolic materials.
How Blood Vessel Occlusion Works
Blood vessel occlusion in brain embolization uses embolic agents to block blood flow. This is done to stop bleeding from an aneurysm or reduce blood flow to a malformation.
A catheter is guided through the vascular system to the target site. There, the embolic material is released. The type of embolic material depends on the condition and the blood vessel anatomy.
Types of Embolic Materials Used
There are many embolic materials used in brain embolization, each with its own use.
| Embolic Material | Description | Common Use |
| Coils | Small, helical devices made of metal | Aneurysm treatment for small aneurysms |
| N-butyl cyanoacrylate (NBCA) | Liquid adhesive that polymerizes upon contact with blood | Treating arteriovenous malformations (AVMs) |
| Ethylene-vinyl alcohol copolymer (EVOH) | Precipitates to form a solid cast within the vessel | Used for AVMs and other vascular malformations |
The table shows that choosing the right embolic material is key, based on the condition being treated.
“The development of new embolic materials has significantly expanded the treatment options for patients with complex neurovascular conditions.”
—Neurovascular specialists highlight.
In conclusion, brain embolization science relies on blocking blood vessels with various materials. Knowing how these materials work and their uses is vital for treating neurovascular conditions.
Aneurysms vs. Embolisms: Understanding the Difference
It’s important to know the difference between aneurysms and embolisms for better treatment. Both affect blood vessels in the brain, but in different ways. This means they need different treatments.
Brain Aneurysm Characteristics
A brain aneurysm occurs when a blood vessel in the brain gets too big. It can burst and cause bleeding in the brain. Most of the time, aneurysms don’t show symptoms until they burst.
Things like family history, high blood pressure, and smoking can increase your risk of getting an aneurysm.
Understanding Cerebral Embolism
A cerebral embolism happens when something blocks a blood vessel in the brain. This blockage can cause a stroke by cutting off oxygen and nutrients. Things like blood clots, plaque, and fat can cause this blockage.
Why Distinguishing Between Aneurysms and Embolisms Matters
Knowing the difference between aneurysms and embolisms is key because their treatments are different. Aneurysms might need clipping or coiling to stop them from bursting. Embolisms, on the other hand, need quick action to get blood flowing again, often through drugs or a mechanical device.
Getting the right treatment depends on knowing the difference. This helps doctors give better care and improve patient results.
The Complete Cerebral Embolization Procedure
Patients going through cerebral embolization face a detailed process. It starts with preparation, moves to the procedure itself, and ends with monitoring. We aim to make this complex process clear and caring for you.
Pre-Procedure Preparation
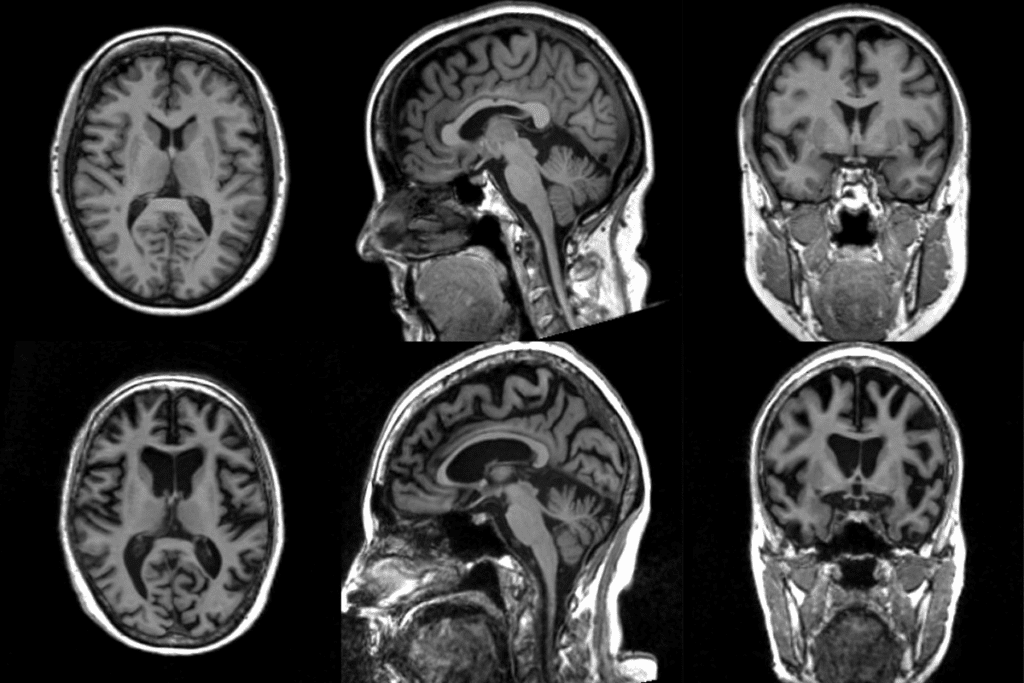
Before starting, patients go through many steps to ensure safety and success. This includes a full medical check-up, imaging tests like angiography or MRI, and talks with our neurovascular experts. They discuss the procedure’s risks and benefits.
Preparation Checklist:
- Medical history review
- Imaging studies (e.g., angiography, MRI)
- Medication adjustment
- Informed consent discussion
Step-by-Step Procedure Walkthrough
The cerebral embolization procedure has several key steps:
- Administration of local anesthesia and conscious sedation
- Insertion of a microcatheter into the femoral artery and navigation to the target site
- Deployment of embolic materials (e.g., coils, liquid embolic agents)
- Real-time monitoring of the embolization process using angiography
Immediate Post-Procedure Monitoring
After the procedure, patients are watched closely in a neuro-intensive care unit. This is to catch any complications or bad reactions early. It’s key for the patient’s safety and treatment success.
| Monitoring Parameter | Description | Duration |
| Vital Signs | Continuous monitoring of blood pressure, heart rate, and oxygen saturation | Several hours post-procedure |
| Neurological Status | Regular assessments of consciousness, pupil response, and limb strength | Ongoing during the hospital stay |
| Imaging Studies | Follow-up angiography or MRI to assess the embolization outcome | Typically performed before discharge |
Knowing the cerebral embolization procedure helps patients prepare better. Our team is dedicated to giving personalized care and support at every step.
7 Key Facts About Aneurysm Embolization Techniques
The success of aneurysm embolization depends on several factors, including the technique used. Different techniques are employed based on the aneurysm’s characteristics, such as its size, location, and morphology.
Fact 1: Coil Embolization Success Rates Exceed 80% for Small Aneurysms
Coil embolization is a widely used technique for treating aneurysms. Studies have shown that for small aneurysms, coil embolization success rates exceed 80%. This technique involves filling the aneurysm with coils to prevent further blood flow into it.
Fact 2: Flow Diversion Devices Revolutionized Treatment of Large Aneurysms
Flow diversion devices have revolutionized the treatment of large and complex aneurysms. These devices are designed to divert blood flow away from the aneurysm, promoting clotting and eventual exclusion of the aneurysm from the circulation.
Fact 3: Liquid Embolic Agents Offer Alternative Solutions
Liquid embolic agents provide an alternative solution for aneurysm treatment. These agents can be used alone or in combination with other techniques, such as coiling. They offer a flexible approach to treating aneurysms with complex morphologies.
Facts 4-7: Critical Considerations for Technique Selection
When selecting an aneurysm embolization technique, several factors must be considered. These include the aneurysm’s size, location, and morphology, as well as the patient’s overall health and medical history.
| Technique | Aneurysm Size | Success Rate |
| Coil Embolization | Small | >80% |
| Flow Diversion | Large/Complex | 70-90% |
| Liquid Embolic Agents | Varies | 60-80% |
Understanding these factors and the characteristics of different embolization techniques is critical for achieving optimal outcomes in aneurysm treatment.
Arteriovenous Malformation (AVM) Embolization
Embolization of arteriovenous malformations (AVMs) is key in modern neurovascular therapy. It offers both cure and relief. AVMs are complex and can cause serious problems like bleeding, seizures, or other symptoms. Thanks to advancements, embolization now plays a big role in treating these issues.
Pre-Surgical Embolization Approaches
Before surgery, embolization helps shrink the AVM. This makes it easier to remove or treat with radiosurgery. By blocking the arteries that feed the AVM, we lower the risk of bleeding during treatment. This step makes the final treatment safer and more effective.
We use different materials for embolization, like liquid embolic agents or coils. The choice depends on the AVM’s size, the arteries it affects, and the treatment plan.
Standalone Curative Embolization
Embolization can sometimes cure AVMs without needing more treatments. This works best for smaller AVMs with the right anatomy. The goal is to block the AVM and veins completely, stopping future bleeding.
For standalone treatment, we need precise planning and execution. We use advanced imaging to guide the procedure. This ensures the embolic material reaches the right spot.
Palliative Embolization for Symptom Control
For big or complex AVMs, palliative embolization can help manage symptoms. It reduces blood flow to the AVM, easing symptoms like headaches or seizures. This improves the patient’s quality of life.
Palliative embolization is done in stages. We aim to control symptoms while avoiding complications.
| Treatment Approach | Goals | Embolic Materials |
| Pre-Surgical Embolization | Reduce AVM size, facilitate surgery or radiosurgery | Liquid embolic agents, coils, particles |
| Standalone Curative Embolization | Complete occlusion of an AVM eliminates hemorrhage risk | Liquid embolic agents, coils |
| Palliative Embolization | Symptom control, improve quality of life | Liquid embolic agents, particles |
Major Benefits of Cerebral Embolization Procedures
Cerebral embolization has changed how we treat neurovascular conditions. It’s a big win for patients because it’s less invasive. This method offers many benefits.
Minimally Invasive Nature and Reduced Trauma
Cerebral embolization is a small procedure compared to open surgery. It only needs a small puncture in the groin. This means less trauma to the patient.
This method also means patients feel less pain and discomfort. It’s great for people with health issues that make surgery risky.
Shorter Hospital Stays and Recovery Times
Cerebral embolization means patients can leave the hospital sooner. They might go home the same day or a few days later. It depends on their health and the procedure’s complexity.
The reduced recovery time is a big plus. It lets patients get back to their lives faster. This is good for people with busy lives or those caring for others.
Treatment Options for Previously Inoperable Conditions
Cerebral embolization now treats once-untreatable conditions. It can handle aneurysms and arteriovenous malformations (AVMs). This is a big step forward in neurovascular treatment.
It gives patients new hope and better outcomes. This has greatly improved their quality of life.
Improved Quality of Life Outcomes
The effects of cerebral embolization last long after treatment. It leads to improved quality of life outcomes. It reduces symptoms and prevents complications, making patients feel better overall.
Patients often say they feel healthier and enjoy life more. They can do things they love and stay independent.
Potential Risks and Brain Embolization Side Effects
Cerebral embolization can have risks and side effects. We aim to make it safe, but knowing the possible complications is key. This helps patients make informed choices.
Procedure-Related Complications
Complications can happen during or after cerebral embolization. These include ischemic events, hemorrhage, and neurological deficits. We do our best to avoid these, but patients need to know about them.
Vasospasm, a temporary blood vessel narrowing, can also occur. Our team watches patients closely to handle any problems quickly.
Device and Material Complications
Complications can also come from the materials used, like coils or glues. These might include device migration or adverse reactions. We use the latest technology and materials to reduce these risks. Our team is ready to handle any issues that come up.
- Coil compaction or migration
- Recanalization of previously embolized vessels
- Allergic reactions to embolic materials
Following post-procedure instructions is key to avoiding complications from devices and materials.
Long-Term Considerations and Follow-up
After cerebral embolization, there are long-term things to think about. These include recurrence of the condition and new vascular lesions. We stress the importance of follow-up care to watch the treated area and handle new problems fast.
We create a personalized follow-up plan for each patient. This might include regular imaging and clinical checks. This ongoing care is vital for the best outcomes and managing long-term side effects or complications.
Recovery After Brain Embolization Surgery
The recovery after brain embolization surgery is complex. It involves immediate care, short-term healing, and long-term follow-up. Understanding what to expect at each stage is key to a smooth recovery.
Immediate Post-Procedure Period
Right after surgery, patients are watched closely in a recovery room or intensive care unit. We manage any complications and make sure they’re comfortable. This time is critical for checking if the surgery was successful and for addressing any immediate issues.
Key aspects of immediate post-procedure care include:
- Monitoring of vital signs and neurological status
- Managing pain and discomfort
- Observing for signs of possible complications
Short-Term Recovery (First Few Weeks)
In the first few weeks, patients may feel tired and have some discomfort as they heal. We tell them to rest and avoid hard activities. Regular check-ups are important to track their healing and answer any questions.
Common experiences during short-term recovery include:
- Fatigue and mild discomfort
- Possible headache or nausea
- Gradual return to normal activities
Long-Term Follow-up and Monitoring
Long-term follow-up is key to the success of brain embolization. We schedule regular visits to check on the treated area and watch for any long-term effects. This ongoing care helps keep the patient healthy and addresses any future concerns.
The table below shows a typical follow-up schedule and what patients can expect during these visits:
| Follow-up Timeframe | Assessment Focus | Typical Procedures |
| 1-3 months | Initial healing, symptom resolution | Clinical evaluation, imaging studies |
| 6-12 months | Treated area stability, long-term efficacy | Imaging studies, clinical assessment |
| 1-2 years and beyond | Long-term outcomes, possible recurrence | Periodic imaging, clinical follow-up |
Following this follow-up schedule helps ensure the best outcomes for patients after brain embolization.
Comparing Endovascular Embolization to Traditional Surgery
Endovascular embolization and traditional surgery are two ways to treat brain conditions. Each has its own benefits and risks. Knowing these differences helps in making the right treatment choice.
Invasiveness and Recovery Differences
Endovascular embolization is less invasive than traditional surgery. It uses a small puncture in the groin to access blood vessels. Traditional surgery, on the other hand, requires a craniotomy to directly access the brain.
Recovery times also differ. Patients with endovascular embolization usually have shorter hospital stays and faster recovery. This is because it causes less tissue damage and avoids open brain surgery.
Risk Profile Comparison
The risks of endovascular embolization and traditional surgery are different. Traditional surgery risks include infection and brain swelling. Endovascular embolization risks include vessel perforation or incomplete embolization.
Yet, endovascular embolization often has fewer complications. It’s a good choice for those at high risk for surgery or with hard-to-reach conditions.
When Open Surgery May Be Preferred
Traditional surgery might be better for some cases. Large aneurysms or complex AVMs need a direct approach. Also, when endovascular access is hard, surgery might be the better option.
Combined Approach Benefits
Using both endovascular embolization and traditional surgery can be the best choice. This hybrid method is great for complex cases. It can reduce risks by decreasing blood flow before surgery.
Understanding the differences helps doctors choose the best treatment for each patient. This leads to better outcomes.
Patient Selection: Are You a Candidate for Cerebral Embolization?
Not everyone is a good fit for cerebral embolization. It’s important to pick the right patients. The success of the procedure depends on finding the right candidates.
Medical Criteria for Procedure Eligibility
To be eligible for cerebral embolization, several factors are considered. These include the type and location of the vascular condition, the patient’s health, and past treatments. We evaluate each patient individually, looking at the latest imaging and medical history.
The criteria include:
- The size and location of the aneurysm or AVM
- The patient’s age and health
- Any past surgeries or treatments
- Any other health issues
Contraindications and Limitations
Cerebral embolization is a valuable treatment, but it’s not for everyone. Those with severe kidney disease or allergies to contrast materials may not be good candidates. Also, patients with certain vascular anatomy or active infections might not be suitable.
It’s also important to know the procedure’s limitations. This includes the risk of complications and the chance of needing more treatments.
Questions to Ask Your Neurovascular Specialist
If you’re thinking about cerebral embolization, talk to your neurovascular specialist. Ask them:
- What are the benefits and risks of the procedure for my condition?
- What other treatments are available, and how do they compare?
- What’s the recovery time, and what follow-up care will I need?
Understanding the criteria, contraindications, and what to expect helps you decide if cerebral embolization is right for you.
Conclusion: The Future of Cerebral Embolization
The field of cerebral embolization is changing fast. New technology and techniques are leading the way. These changes will make treatments better and give patients more options.
New materials and devices, like advanced coils and flow diversion devices, are making procedures safer and more effective. Better imaging technologies also help plan treatments more accurately.
In the future, we’ll see more use of minimally invasive methods. This could mean shorter recovery times and better lives for patients. Research and innovation will keep improving how we manage brain issues.
We’re excited about the future of cerebral embolization. With ongoing improvements, patients can look forward to better outcomes and a higher quality of life.
FAQ
What is cerebral embolization?
Cerebral embolization is a procedure to treat brain conditions. It uses embolic materials to block blood vessels. This helps with aneurysms and arteriovenous malformations (AVMs).
What is the difference between an aneurysm and an embolism?
An aneurysm is a bulge in a blood vessel wall. An embolism is when something blocks a blood vessel. Knowing this helps doctors choose the right treatment.
How does cerebral embolization work?
It involves putting embolic materials into a blood vessel. This blocks the vessel. It treats conditions like aneurysms or AVMs.
What are the benefits of cerebral embolization?
It’s less invasive, which means less trauma. Recovery times are shorter. It can treat once untreatable conditions, improving life quality.
What are the risks associated with brain embolization?
Risks include complications from the procedure. There are also issues with devices and materials. Long-term effects are a concern, making follow-up care key.
What is the recovery process like after brain embolization surgery?
Recovery starts right after surgery. It includes a short-term recovery phase and long-term monitoring. Patients are told what to expect and how to recover.
How does endovascular embolization compare to traditional surgery?
Endovascular embolization is less invasive than traditional surgery. It has different recovery and risk profiles. It might be preferred in some cases, but a combined approach can also be beneficial.
What are the criteria for being a candidate for cerebral embolization?
Doctors choose patients based on medical criteria. They look at the condition’s type and severity. They also check for contraindications. Patients should ask their neurovascular specialist questions.
What advancements are being made in cerebral embolization?
New advancements are improving treatment outcomes. They’re expanding options for brain conditions. This is shaping the future of cerebral embolization.
What is coil embolization, and what are its success rates?
Coil embolization treats aneurysms by filling them with coils. It has success rates over 80% for small aneurysms. It’s a very effective treatment.
What is the role of flow diversion devices in aneurysm treatment?
Flow diversion devices have changed large aneurysm treatment. They offer an alternative to traditional coiling. They provide a new way to manage complex aneurysms.
What are liquid embolic agents used for?
Liquid embolic agents treat vascular conditions like aneurysms and AVMs. They offer a different approach to em
bolization.
References
- Sugiu, K., or others. (2008). Complications of embolization for cerebral arteriovenous malformations. Journal of Neurosurgery, 109(3), 463-468. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3522223/
- Ahmad, S. (2020). Clinical outcome of endovascular coil embolization for cerebral aneurysms in the Asian population in relation to risk factors: a 3-year retrospective analysis. BMC Surgery, 20, Article 104. https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-020-00756-1








