Last Updated on November 27, 2025 by Bilal Hasdemir

Getting a brain tumor diagnosis can be scary. But new surgical methods have made treatments better. At Liv Hospital, we focus on you, giving trusted care for brain cancer surgery.
We aim to give you a full guide on brain mass surgery. We’ll cover everything from getting ready to healing. You’ll learn about the surgery steps, the techniques used, and what to expect when you’re recovering. This way, you’ll feel informed and supported every step of the way.
Key Takeaways
- Advanced surgical techniques improve treatment outcomes for brain tumor patients.
- A patient-focused approach is key in cerebral tumor surgery.
- Knowing the surgery process helps with better preparation and recovery.
- Liv Hospital offers trusted care for complex surgeries.
- Recovery guidance is vital for post-surgery support.
Understanding Brain Tumors and Their Impact

It’s important for patients and doctors to understand brain tumors. These tumors can be either benign or malignant. Their impact on a person’s life depends on their type, size, and where they are in the brain.
Types of Brain Tumors: Malignant vs. Non-Malignant
Brain tumors are divided into two main types: malignant and non-malignant (benign). Malignant tumors are cancerous and can spread to other parts of the brain. Benign tumors, on the other hand, are not cancerous and grow more slowly. Knowing the difference is key to choosing the right treatment.
Common Symptoms and Diagnosis Methods
The symptoms of brain tumors can vary a lot. They might include headaches, seizures, and changes in thinking. Doctors use MRI or CT scans to diagnose them. Finding and treating tumors early is very important.
When Surgical Intervention Is Necessary
Surgery is often needed for brain tumors that cause big problems or are thought to be malignant. Doctors consider many things before deciding on surgery. These include where the tumor is, how big it is, and the patient’s health.
Can You Remove a Brain Tumor? Factors Affecting Surgical Decisions
Whether a brain tumor can be removed surgically depends on several things. These include the tumor’s type, where it is, and the patient’s brain health. Thanks to new imaging and surgery methods, more tumors can be removed. But, some tumors are too hard to reach or too big to remove safely.
Pre-Surgical Evaluation and Planning

Before surgery, we do a detailed check-up to make sure everything is ready for a safe and successful operation. This time can be tough for patients and their families. So, we make sure to do a full check-up to find the best way to help.
Imaging Techniques for Tumor Assessment
We use advanced imaging to look at the tumor’s size, where it is, and how it affects the brain. We use:
- MRI (Magnetic Resonance Imaging): Gives us clear pictures of the brain and tumor. This helps us see how big the tumor is and its impact on the brain.
- CT (Computed Tomography) scans: Quick and useful in emergencies. They show us if there’s bleeding or other problems.
- Functional MRI (fMRI): Maps brain functions. This is key when planning surgery near important brain areas.
The Multidisciplinary Tumor Board Approach
Our team, including neurosurgeons, oncologists, and radiologists, comes together to plan treatment. This team effort makes sure we cover all bases, leading to a better plan for treatment.
“The tumor board’s multidisciplinary approach is key in making informed decisions. It ensures we look at all options and use our expertise.” “ A neuro-oncologist
Patient Preparation for Brain Surgery
Getting ready for brain surgery means getting both physically and emotionally ready. We tell patients to:
- Follow pre-surgical instructions, like any changes in medication or lifestyle.
- Attend pre-surgical consultations to talk about any worries or questions.
- Plan for post-surgical care, making sure they have support after surgery.
By carefully checking the tumor and planning the surgery, we can greatly improve patient outcomes. Our aim is to give the best care, from start to finish.
Brain Tumor Removal Techniques
Removing brain tumors requires different surgical methods. Each method has its own benefits and challenges. We will look into these techniques closely, discussing their uses and advantages.
Craniotomy: The Standard Approach
Craniotomy is the most common surgery for brain tumors. It involves temporarily removing a part of the skull to reach the brain. This method lets neurosurgeons see and remove the tumor directly.
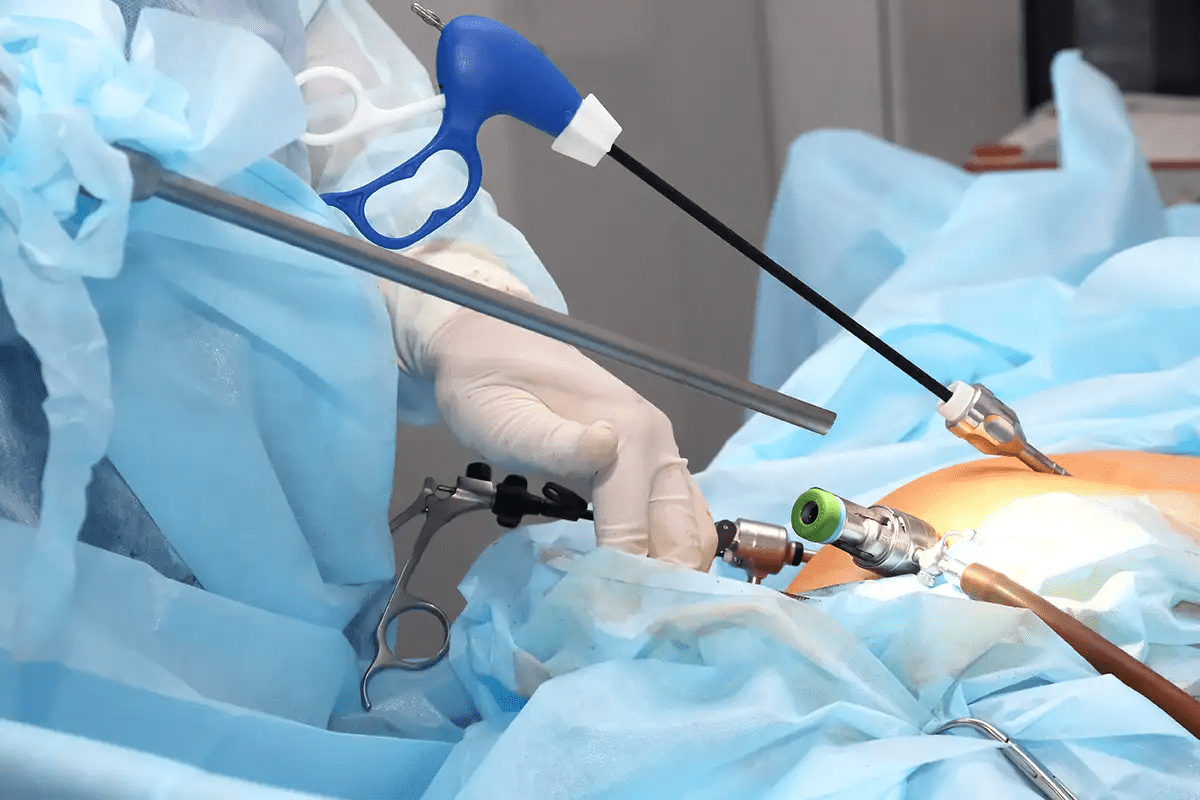
Minimally Invasive Procedures
Minimally invasive surgeries are also used for brain tumors. These methods use smaller cuts and disturb less brain tissue. Minimally invasive brain surgery is great for tumors in hard-to-reach or sensitive areas.
Awake Craniotomy for Functional Areas
Awake craniotomy is used for tumors in critical brain areas. These areas control important functions like speech or movement. During this surgery, the patient stays awake. This lets the team watch brain function as they work.
| Technique | Invasiveness | Recovery Time | Application |
| Craniotomy | High | Several weeks | General brain tumor removal |
| Minimally Invasive | Low | Less than a week | Tumors in sensitive areas |
| Awake Craniotomy | High | Several weeks | Tumors in functional areas |
The choice of surgery for brain tumors depends on many factors. These include the tumor’s location, size, and the patient’s health. Knowing about these methods helps in making informed treatment choices.
Step-by-Step Process of Brain Mass Surgery
Removing a brain tumor is a detailed and precise process. It needs a lot of skill and knowledge. We will explain the main steps of this complex surgery.
Anesthesia and Positioning
The first step is giving anesthesia to keep the patient comfortable and pain-free. We use general anesthesia to make the patient sleep. Then, we place the patient on the operating table in the best position for the surgery.
Patient positioning is very important. We use special equipment to keep the head stable and in the right position.
Accessing the Brain
To get to the brain tumor, we do a craniotomy. This means we temporarily remove a part of the skull. It helps us reach the tumor without harming the brain too much.
We use high-tech imaging to plan the best way to get to the tumor. This way, we avoid damaging important brain areas.
Tumor Identification and Removal
With access to the brain, we use different methods to find and remove the tumor. We might use intraoperative imaging to see the tumor clearly and check how much we’ve removed.
We carefully cut around the tumor to avoid harming the brain. Our goal is to take out as much of the tumor as we can safely.
Closure and Immediate Post-Op Care
After taking out the tumor, we close the craniotomy site. We put the bone flap back and secure it with plates or stitches. Then, we close the scalp with stitches or staples.
Right after surgery, we watch the patient closely in the ICU. We manage their pain and other symptoms to keep them comfortable.
| Step | Description | Key Considerations |
| Anesthesia and Positioning | Administering anesthesia and positioning the patient for optimal access. | Ensuring patient comfort and safety. |
| Accessing the Brain | Performing a craniotomy to access the tumor. | Minimizing damage to surrounding brain tissue. |
| Tumor Identification and Removal | Identifying and removing the tumor using advanced imaging techniques. | Preserving neurological function. |
| Closure and Immediate Post-Op Care | Closing the craniotomy site and monitoring the patient post-operatively. | Managing pain and monitoring for complications. |
Advanced Technologies in Brain Tumor Resection
Brain tumor surgery has become more precise and effective. Advanced technologies help us offer targeted and less invasive treatments. This improves patient outcomes and shortens recovery times.
Stereotactic Navigation Systems
Stereotactic navigation systems are key in brain tumor surgery. They use imaging and tracking to guide surgeons in real-time. This ensures accurate tumor removal, which is critical in complex brain surgeries.
Intraoperative Imaging (MRI, Ultrasound)
Intraoperative imaging, like MRI and ultrasound, gives surgeons real-time feedback. It lets them check the tumor removal progress and make adjustments. MRI, for example, can show how much tumor is left.
| Imaging Technique | Advantages | Limitations |
| Intraoperative MRI | High-resolution imaging, real-time feedback | High cost, limited availability |
| Intraoperative Ultrasound | Real-time imaging, cost-effective | Operator-dependent, limited depth penetration |
Fluorescence-Guided Surgery
Fluorescence-guided surgery uses fluorescent dyes to highlight tumors. This makes it easier to remove tumors accurately. We’ve seen great results using this technology for brain mass removal.
Laser Interstitial Thermal Therapy
Laser interstitial thermal therapy (LITT) uses laser heat to destroy tumors. It’s great for tumors that are hard to reach or in sensitive areas. LITT is a promising option for brain surgery for tumor removal.
These advanced technologies have changed neurosurgery for the better. They let us do more complex surgeries safely and precisely. As we keep improving these tools, we expect better results for our patients.
Inoperable Brain Tumors: When Surgery Isn’t an Option
An inoperable brain tumor is one that can’t be safely removed by surgery. This is because of its location, size, or how it affects important brain parts. It’s tough for patients and their families to hear this. But there are other ways to treat it.
Defining Inoperable Brain Masses
Inoperable brain masses are close to vital brain areas or spread out. This makes surgery too risky or not possible. Reasons a tumor might be inoperable include:
- Being near important brain spots
- Touching major blood vessels or nerves
- Spreading out or growing in many places
- The patient’s health and past medical issues
We help patients understand their situation and find the best treatment.
Alternative Treatment Approaches
When surgery isn’t an option, other treatments can help. These include:
- Radiation Therapy: Uses beams to shrink the tumor.
- Chemotherapy: Medications to kill or slow tumor cells.
- Targeted Therapy: Drugs that target cancer cells or their environment.
- Palliative Care: Helps with symptoms and stress of serious illness.
Each patient gets a treatment plan that fits their needs and tumor type.
Clinical Trials and Emerging Options
Some patients might be able to try new treatments in clinical trials. These new options could be:
- Immunotherapy: Uses the body’s immune system to fight cancer.
- Gene therapy: Changes genes to prevent or treat disease.
- Advanced radiation techniques, like stereotactic radiosurgery.
We suggest talking to a healthcare provider about these options. They can see if you’re a good fit for a clinical trial.
Non-Malignant Brain Tumor Surgery: Special Considerations
When dealing with non-malignant brain tumors, surgery needs to be carefully planned. We focus on removing the tumor without harming the brain around it. This approach helps keep brain function intact.
Meningioma Removal Techniques
Meningiomas grow from the meninges, which protect the brain and spinal cord. Surgical removal is usually the best option for these tumors. We use advanced imaging and planning to remove the tumor safely.
The main goal is to remove the tumor completely. This includes any dura mater involved. We use intraoperative imaging and neuromonitoring to guide the surgery.
Acoustic Neuroma Surgery
Acoustic neuromas, or vestibular schwannomas, grow on the nerve from the inner ear to the brain. Surgery aims to remove the tumor without harming the facial nerve or hearing. When possible.
We use advanced surgical techniques like microsurgery and stereotactic radiosurgery. The choice depends on the tumor’s size, location, and the patient’s health and wishes.
We tailor our care to each patient’s needs. Our goal is to remove benign brain tumors effectively. Our team provides full care, from the first visit to after surgery and follow-ups.
Post-Surgery Recovery Timeline
Knowing the recovery timeline after brain tumor surgery is key for patients and their caregivers. We’ll walk you through the recovery stages, from right after surgery to long-term rehab.
Immediate Recovery (First 48 Hours)
The first 48 hours after brain tumor removal surgery are very important. Patients are watched closely in the ICU for any issues like bleeding or infection. We make sure pain is well managed, keeping patients comfortable.
Patients might feel confused, sleepy, or have trouble speaking and moving. Our team is always ready to help and answer any questions.
Short-Term Recovery (First Month)
When patients move from the ICU to the general ward, they start their short-term recovery. This stage includes watching their condition, managing symptoms, and starting therapy.
We encourage patients to start with simple exercises and then do more challenging ones. Regular check-ups with our neurosurgery team are key to tracking healing and addressing any issues.
Long-Term Recovery and Rehabilitation
Long-term recovery after brain tumor surgery varies. It depends on the tumor’s size, location, and the patient’s health. Some may need ongoing rehab to regain lost functions or manage symptoms.
Our rehab team creates plans tailored to each patient. This may include physical, occupational, and speech therapy. We also help with any cognitive or emotional changes.
Throughout recovery, we stress the importance of follow-up care. By understanding the recovery timeline, patients and their families can prepare for what’s ahead.
Managing Complications After Brain Tumor Extraction
Managing complications after brain tumor surgery is key. After surgery, patients are watched closely for any signs of trouble. This could affect their recovery.
Common Complications and Their Management
After brain tumor surgery, patients might face issues like infection, bleeding, and neurological problems. Effective management of these is vital for the best results.
| Complication | Management Strategy |
| Infection | Antibiotics, wound care, and monitoring for signs of infection |
| Bleeding | Close monitoring of vital signs, imaging studies to detect bleeding |
| Neurological Deficits | Rehabilitation therapy, including physical, occupational, and speech therapy |
Warning Signs to Monitor
It’s important for patients and caregivers to watch for warning signs. These could mean complications are happening.
- Increasing headache or pain
- Confusion or changes in mental status
- Weakness or numbness in the face, arm, or leg
- Difficulty speaking or swallowing
- Fever or signs of infection
Prompt recognition of these signs can help get the right help fast. This can lead to better outcomes.
When to Seek Medical Attention
If you notice any of these signs, get medical help right away. Early intervention is critical for managing complications and recovery.
Knowing about possible complications and warning signs helps patients and caregivers. They can play a big role in recovery. And they know when to get medical help.
Conclusion: Advances and Future Directions in Brain Tumor Surgery
Brain tumor surgery is getting better thanks to new technology and techniques. Tools like stereotactic navigation systems and intraoperative imaging help doctors remove tumors more accurately. This leads to better results for patients.
The future looks bright for brain tumor surgery. Researchers are working hard to make these techniques even better. We’re committed to keeping up with these advancements to give patients the best care.
By using these new methods, we’re not just saving lives. We’re also making sure patients live better lives. It’s important to keep investing in research to improve brain tumor surgery. This way, we can give the best possible care to those who need it.
FAQ
What is the primary goal of brain tumor surgery?
The main goal is to remove the tumor while keeping the healthy brain tissue safe.
Can all brain tumors be removed surgically?
No, not all brain tumors can be removed by surgery. Some tumors are too hard to reach or have other issues.
What are the different techniques used for brain tumor removal?
There are several methods, including craniotomy, minimally invasive procedures, and awake craniotomy.
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is removed to get to the brain.
What is awake craniotomy?
Awake craniotomy is a method where the patient stays awake. This helps the surgeon avoid harming important brain areas.
How is brain tumor surgery planned?
Surgery planning uses advanced imaging and a team approach to make sure the treatment is right.
What are the risks and complications associated with brain tumor surgery?
Risks include infection, bleeding, and damage to the brain around the tumor.
How long does it take to recover from brain tumor surgery?
Recovery time varies. It includes an immediate phase, a short-term phase, and a long-term phase.
What are the alternative treatment approaches for inoperable brain tumors?
For tumors that can’t be removed, treatments include radiation, chemotherapy, and clinical trials.
Can non-malignant brain tumors be removed surgically?
Yes, non-cancerous brain tumors can be removed. The method depends on the tumor’s type and location.
What is laser interstitial thermal therapy?
Laser interstitial thermal therapy is a minimally invasive method. It uses a laser to kill tumor cells by heating them.
How is brain tumor removal surgery performed?
Surgery involves steps like anesthesia, accessing the brain, finding and removing the tumor, and closing the incision.
What is the role of a multidisciplinary tumor board in brain tumor surgery?
A tumor board is key. It brings experts together to plan a complete treatment strategy.
What are the warning signs to monitor after brain tumor surgery?
Watch for signs of infection, increased pressure in the brain, and any changes in brain function.
When should I seek medical attention after brain tumor surgery?
Seek help right away if you have severe headaches, confusion, or weakness.
References
- Choi, B. D., Karmonik, C., & Berger, M. S. (2024). Recent Advances in the Diagnosis and Treatment of Brain Tumors. Brain Sciences, 14(3), 224. https://www.mdpi.com/2076-3425/14/3/224
- Preoperative mapping techniques for brain tumor surgery. (2024). Frontiers in Oncology. https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1481430/full