Last Updated on December 1, 2025 by Bilal Hasdemir
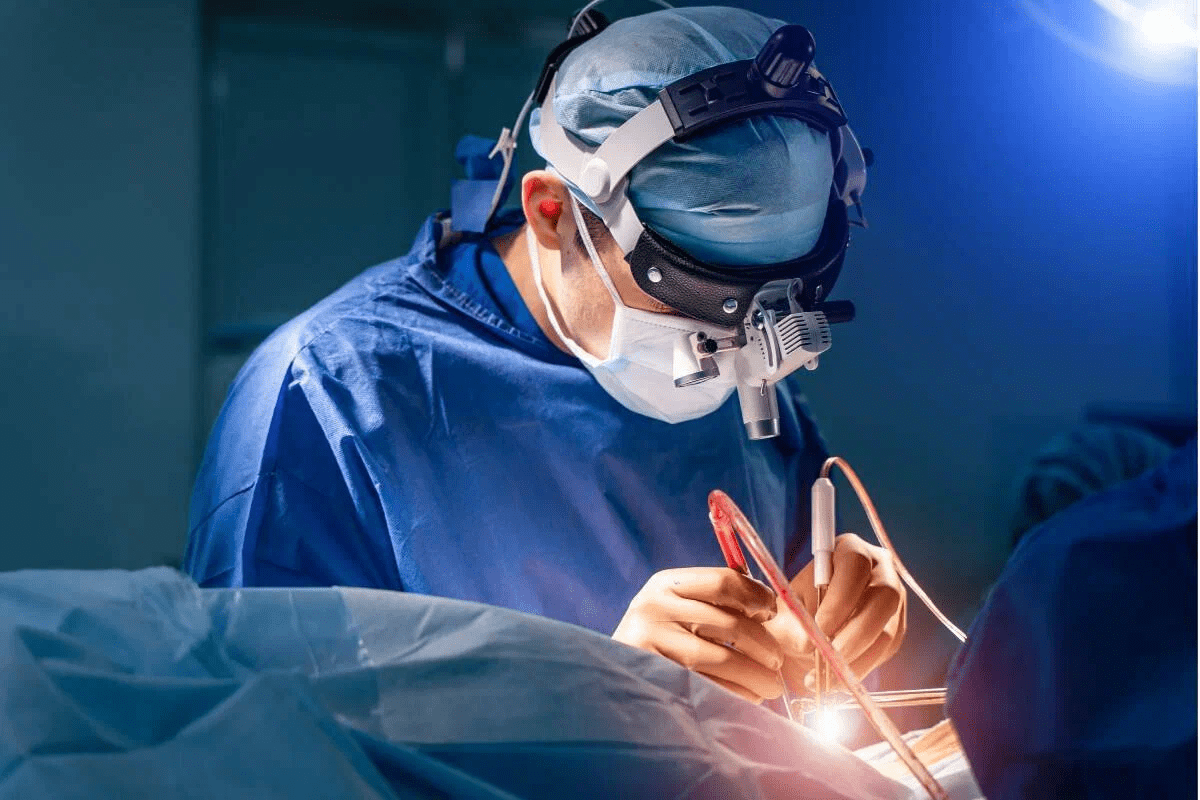
Key Takeaways
- Approximately 800,000 people in the U.S. experience strokes annually.
- Ischemic strokes account for about 85% of all stroke cases.
- Atherosclerosis buildup is a significant risk factor for ischemic strokes.
- Understanding the causes of CVAs is crucial for prevention and treatment.
Understanding Cerebrovascular Accidents (Strokes)
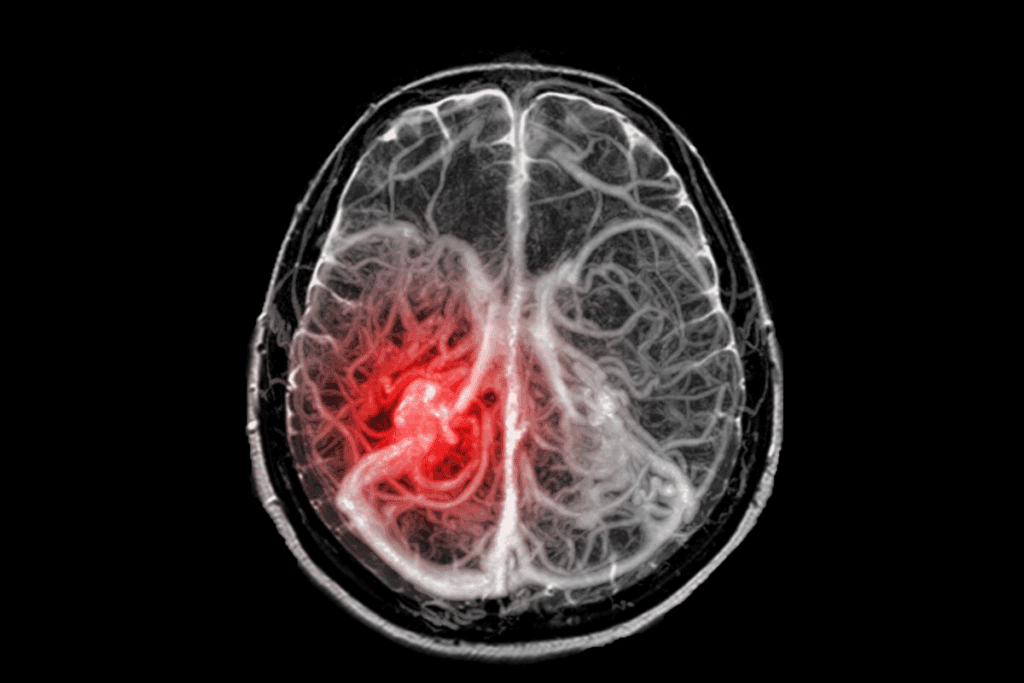
A detailed anatomical cross-section depicting the effects of an ischemic stroke on the brain. In the foreground, a realistic rendering of an occluded cerebral artery, the blockage causing disruption of blood flow and oxygen supply. In the middle ground, a precise visualization of the resulting tissue damage and infarction, areas of the brain parenchyma experiencing necrosis. The background showcases the overall structure of the brain, with muted tones emphasizing the severity of the condition. Rendered in a clinical, scientific style using realistic lighting, depth of field, and attention to anatomical accuracy to convey the complexity and impact of a cerebrovascular accident.
It’s key to know about cerebrovascular accidents to stop and treat them. These are called strokes. They happen when a blood vessel in the brain gets blocked or bursts. What is the most common cerebrovascular accident cause? We reveal the #1 risk factor. This is critical information for stroke prevention.
Definition and Terminology
A cerebrovascular accident is when the brain doesn’t get enough blood. This stops brain tissue from getting oxygen and nutrients. It can cause damage and be very dangerous.
The term “stroke” is often used to mean the same thing. It shows how quickly and severely it affects the brain.
Doctors have special words for different parts of cerebrovascular accidents. For example, “ischemic stroke” means a blood vessel is blocked. “hemorrhagic stroke” means there’s bleeding in or around the brain.
Atherosclerosis: The Leading Cerebrovascular Accident Cause

A detailed cross-section of a human artery, showcasing the progressive buildup of atherosclerotic plaque. The foreground depicts the arterial wall, with distinct layers of endothelium, intima, media, and adventitia. The middle ground highlights the gradual accumulation of cholesterol, lipids, and inflammatory cells, narrowing the lumen and restricting blood flow. The background features a realistic lighting setup, with subtle shadows and highlights emphasizing the textural complexity of the plaque formation. The overall scene conveys a sense of medical significance, capturing the essence of the leading cause of cerebrovascular accidents in a scientifically accurate and visually compelling manner.
Atherosclerosis is a major cause of cerebrovascular accidents. It happens when arteries narrow due to plaque buildup. This condition is influenced by hypertension risk and cholesterol levels.
Development of Atherosclerosis
Atherosclerosis starts with plaque in the arterial walls. It grows over time, especially with high blood pressure and high cholesterol. As plaque grows, arteries narrow, cutting off blood to vital organs like the brain.
The steps to develop atherosclerosis are:
- Initial injury to the arterial wall
- Accumulation of lipids and inflammatory cells
- Formation of a fibrous cap over the plaque
- Potential rupture of the plaque, leading to acute blockage
Plaque Formation and Stroke
When atherosclerotic plaque ruptures, it can cause a blood clot. This clot can block the artery, leading to an ischemic stroke. The brain gets damaged because it lacks oxygen and nutrients.
The steps from plaque to stroke are:
- Plaque instability and rupture
- Thrombus formation at the site of rupture
- Embolization of the clot to smaller arteries in the brain
- Resulting ischemia and brain tissue damage
Understanding atherosclerosis and its link to cerebrovascular accidents is key. It helps in creating better prevention and treatment plans. Keeping hypertension risk in check and maintaining healthy cholesterol levels are crucial to lower stroke risk.
Ischemic Strokes: The Most Common Type
Thrombotic Strokes
Thrombotic strokes happen when a blood clot forms in a brain-supplying artery. This clot blocks blood flow. The clot can form because of atherosclerosis, where plaque builds up in arteries. As the plaque grows, it can burst, causing a clot.
Embolic Strokes
Embolic strokes are caused by an embolus, a clot that travels to the brain from elsewhere in the body. This usually happens because of heart problems like atrial fibrillation. Knowing where emboli come from is key to stopping embolic strokes.
Both thrombotic and embolic strokes can severely harm the brain. They can cause tissue damage and loss of brain function. Quick medical help is crucial to reduce damage and improve chances of recovery.
Blood Clot Formation and Artery Blockage
A cross-section of an artery, with a prominent blood clot formation obstructing the lumen. The clot appears as a ragged, irregular mass, with a reddish-brown hue, partially occluding the vessel. Surrounding the clot is the arterial wall, with its distinct layers visible – the intima, media, and adventitia. The lighting is realistic, with a soft, even illumination that accentuates the textures and shades of the clot and the arterial structure. The perspective is slightly elevated, providing a clear, detailed view of the clot and its impact on the vessel. The overall mood is one of clinical precision, highlighting the medical significance of this pathological process.
Blood clotting is a complex process that can cause artery blockage, leading to stroke. When a blood clot forms in a blood vessel, it blocks blood flow. This can damage brain tissue.
The Clotting Process
The clotting process starts with damage to the blood vessel wall. This damage exposes collagen and tissue factor. Platelets then stick to the damaged area, attracting more platelets and starting the coagulation cascade.
The coagulation cascade is a series of reactions that lead to thrombin formation. Thrombin then changes fibrinogen into fibrin. This fibrin mesh traps blood cells and platelets, forming a blood clot.
How Clots Lead to Brain Damage
A blood clot can block an artery, cutting off blood to the brain. This leads to ischemia and damage. The damage’s severity depends on the clot’s location, size, and how long it blocks the artery.
If the blockage isn’t quickly resolved, brain tissue can be permanently damaged. This can lead to long-term disability or even death.
The table below shows the potential outcomes of artery blockage due to blood clot formation. It depends on the blockage’s severity and duration.
| Blockage Duration | Severity of Blockage | Potential Outcome |
| Short-term | Partial | Transient Ischemic Attack (TIA) |
| Prolonged | Complete | Ischemic Stroke |
| Variable | Variable | Brain Ischemia, potentially leading to Infarction |
Understanding blood clot formation and artery blockage is key. It helps in developing prevention and treatment strategies for cerebrovascular accidents.
Hypertension: A Major Risk Factor
A high-contrast, hyper-realistic medical illustration depicting the cardiovascular system under the strain of hypertension. In the foreground, a cross-section of an artery shows thickened, hardened walls and narrowed lumen, indicating arterial stiffness and reduced blood flow. The middle ground features a detailed diagram of the heart, with enlarged ventricles and prominent vasculature to represent the increased workload. In the background, a three-dimensional model of the brain highlights the delicate cerebrovascular network, hinting at the heightened risk of stroke. Dramatic, directional lighting casts dramatic shadows, conveying a sense of tension and urgency. Muted, desaturated color palette evokes a clinical, diagnostic atmosphere.
Damage to Blood Vessels
Hypertension harms blood vessels in many ways. High blood pressure can make blood vessels weak and more likely to block or burst. This can cause aneurysms or narrow arteries, raising stroke risk.
Damage to blood vessels can also lead to scar tissue. This scar tissue can narrow the vessel. This narrowing, called stenosis, can cut down blood flow to the brain. This increases the chance of an ischemic stroke.
Blood Pressure Management for Stroke Prevention
Managing hypertension is key to preventing strokes. Effective blood pressure management involves lifestyle changes and, if needed, medication. Keeping blood pressure in check can greatly lower stroke risk.
Changes in lifestyle can help manage hypertension. Eating well, exercising, drinking less alcohol, and not smoking are good steps. Sometimes, doctors will prescribe medication to control blood pressure.
By knowing the risks of hypertension and managing blood pressure, people can lower their stroke risk. This helps keep their heart health in check.
Atrial Fibrillation and Other Heart Conditions
Atrial fibrillation and stroke risk: a realistic depiction of the cardiovascular system. In the foreground, a detailed illustration of the heart, its chambers, and the irregular electrical impulses associated with atrial fibrillation. In the middle ground, a network of blood vessels, with areas highlighted to indicate increased stroke risk. In the background, a subtle anatomical diagram, conveying the connection between the heart condition and cerebrovascular events. The scene is rendered with a clean, medical illustration style, utilizing muted tones and precise, technical linework. Lighting is soft and directional, emphasizing the structure and form of the anatomical elements. The overall mood is one of educational clarity, inviting the viewer to understand the relationship between atrial fibrillation and stroke risk.
Atrial fibrillation and other heart conditions are key when we talk about stroke risk. Atrial fibrillation, with its irregular heartbeats, raises the risk of blood clots. These clots can cause a stroke.
Connection Between Heart Disease and Stroke
Heart disease and stroke are closely related. Many heart conditions, like atrial fibrillation, raise stroke risk. Atrial fibrillation is a common heart rhythm disorder linked to stroke.
| Heart Condition | Stroke Risk | Prevention Strategies |
| Atrial Fibrillation | High | Anticoagulation therapy, rhythm control |
| Coronary Artery Disease | Moderate | Lifestyle modifications, antiplatelet therapy |
| Heart Valve Disorders | Variable | Surgical intervention, anticoagulation |
It’s important to understand the link between heart disease and stroke. By managing heart conditions and reducing risk factors, we can lower stroke rates. This improves patient outcomes.
Hemorrhagic Stroke Causes
A detailed anatomical illustration depicting the causes of hemorrhagic stroke. In the foreground, a cross-sectional view of the brain showcases the intricate blood vessels and highlights areas of ruptured or weakened blood vessels. The middle ground features a magnified view of the damaged vessels, with emphasis on factors like hypertension, aneurysms, and arteriovenous malformations that can lead to hemorrhagic stroke. The background provides a realistic, muted color palette with subtle gradients to create depth and a sense of scientific inquiry. The lighting is soft and diffused, lending a clinical yet approachable feel to the image. The overall composition and technical execution convey a sense of educational purpose, aiding in the understanding of this critical medical condition.
A hemorrhagic stroke happens when a blood vessel bursts and bleeds into or around the brain. This type of stroke is less common but can be more severe. The bleeding can damage the brain and lead to serious complications.
Aneurysm Rupture
An aneurysm is a bulge in a blood vessel that can burst, causing bleeding. When it ruptures, it leads to a subarachnoid hemorrhage, bleeding around the brain. This is a medical emergency that needs immediate care.
High blood pressure, smoking, and a family history of aneurysms increase the risk of rupture. Knowing these risk factors helps in prevention and early detection.
Arteriovenous Malformations
Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels in the brain. They can rupture, causing a hemorrhagic stroke. AVMs are present at birth but may not be diagnosed until later, often after they rupture.
Symptoms of AVMs can vary, from seizures to headaches. Treatment options include surgery, embolization, and radiation therapy. These aim to reduce the risk of rupture.
Understanding hemorrhagic stroke causes, like aneurysm rupture and AVMs, is key to better prevention and treatment. We focus on addressing these conditions to improve patient outcomes and save lives.
Modifiable Risk Factors for Cerebrovascular Accidents
Knowing and managing risk factors is crucial for preventing strokes. By tackling these factors, we can lower the chance of having a stroke.
Smoking and Tobacco Use
Smoking is a major risk for stroke. Tobacco smoke harms the heart and blood vessels, leading to blockages and ruptures. Quitting smoking can greatly lower stroke risk.
Diabetes and Blood Sugar Control
Diabetes is a big risk for stroke. High blood sugar damages blood vessels, raising the risk of blockages. Controlling diabetes through lifestyle and medicine can lower this risk.
It’s important for people with diabetes to check their blood sugar often and follow their treatment plans. This helps reduce stroke risk.
Cholesterol Levels and Management
High LDL cholesterol can cause artery blockages, increasing stroke risk. Lowering cholesterol through diet, exercise, and medicine can help.
| Cholesterol Type | Desirable Level | Action Required |
| LDL Cholesterol | Less than 100 mg/dL | Lifestyle changes and possibly medication |
| HDL Cholesterol | 60 mg/dL or higher | Maintain healthy lifestyle |
| Total Cholesterol | Less than 200 mg/dL | Monitor and adjust lifestyle as needed |
Non-Modifiable Risk Factors
Some risk factors for stroke can be managed, but others can’t. Non-modifiable risk factors are those we can’t change. Knowing these factors helps us understand our stroke risk and how to lower other risks.
Age and Gender Considerations
Age is a big risk factor for stroke. Most strokes happen to people over 65. The American Heart Association says stroke risk doubles every decade after 55. Knowing this can help us make better choices about managing other risks. Men usually have a higher stroke risk than women, but women’s risk goes up after menopause.
Genetic and Ethnic Factors
Genetic predisposition is another risk factor we can’t change. If your family has a history of stroke, you might be at higher risk. Some genetic conditions can also raise your risk. Ethnicity matters too, with African Americans facing a higher risk. Knowing these factors helps us spot and manage stroke risk early.
Having non-modifiable risk factors doesn’t mean you’ll definitely have a stroke. It shows how important it is to manage the risks we can change. By tackling both types of risks, we can prevent strokes and improve our health.
Transient Ischemic Attacks: Warning Signs
Knowing the signs of a transient ischemic attack can help prevent a stroke. TIAs, or “mini-strokes,” are brief blockages in brain blood flow. They warn of a possible bigger stroke.
Recognizing a TIA
Symptoms of a TIA are like those of a stroke. They include sudden weakness, trouble speaking, vision changes, dizziness, or loss of balance. These symptoms last from minutes to hours and go away within 24 hours.
Act fast if you or someone else has these symptoms. Even if they seem to go away, get medical help right away. TIAs are emergencies and need urgent care.
Vessel Narrowing and Brain Ischemia
The narrowing of vessels, especially in the carotid and intracranial arteries, is a big risk for brain ischemia. This narrowing means the brain gets less blood, which can lead to ischemia or even a stroke. We will look into how this happens and its effects on brain health.
Carotid Artery Stenosis
Carotid artery stenosis is when the carotid arteries narrow. These arteries are key because they carry a lot of blood to the brain. The narrowing is often due to atherosclerosis, where plaque builds up inside the arteries.
Key Factors in Carotid Artery Stenosis:
- Atherosclerosis: The buildup of plaque inside the carotid arteries.
- Hypertension: High blood pressure can damage the artery walls, making them more susceptible to narrowing.
- Smoking: Tobacco use is a significant risk factor for developing carotid artery stenosis.
Intracranial Artery Stenosis
Intracranial artery stenosis is when the arteries inside the brain narrow. This can cause reduced blood flow to certain brain areas, leading to ischemia. The causes and risk factors are similar to those of carotid artery stenosis, with atherosclerosis being a main concern.
| Condition | Causes | Risk Factors |
| Carotid Artery Stenosis | Atherosclerosis, Plaque Buildup | Hypertension, Smoking, High Cholesterol |
| Intracranial Artery Stenosis | Atherosclerosis | Hypertension, Diabetes, Smoking |
Recent Advances in Understanding Stroke Causes
Medical research has made big strides in understanding stroke causes. We now know more about the genetic and inflammatory factors involved. This helps us grasp the complex reasons behind cerebrovascular accidents.
Genetic Risk Factors
Genetics play a big role in stroke risk. Research has found several genetic variants linked to stroke. For example, some genes can make people more likely to develop high blood pressure and atherosclerosis, both major stroke risks.
Learning about these genetic links helps us create better prevention plans. This is especially important for those at higher genetic risk.
| Genetic Factor | Association with Stroke |
| Hypertension-related genes | Increased risk of hemorrhagic stroke |
| Atherosclerosis-related genes | Increased risk of ischemic stroke |
| Genetic variants affecting blood clotting | Increased risk of thrombotic events |
Inflammatory and Immune Mechanisms
Inflammation is key in stroke development. Recent studies show how blood vessel inflammation can cause atherosclerosis and stroke risk.
Immune mechanisms also play a part. Autoimmune conditions, for instance, can cause inflammation and damage blood vessels. Knowing this helps us find new ways to treat inflammation and immune responses.
Understanding genetic and inflammatory factors in stroke leads to better prevention and treatment. This includes personalized medicine and anti-inflammatory therapies.
As we learn more about stroke causes, we’re getting closer to reducing its impact. Recent breakthroughs give us hope for better outcomes for those at risk of stroke.
Prevention Strategies for Cerebrovascular Accidents
Preventing cerebrovascular accidents needs a mix of lifestyle changes and medical care. Knowing and using these strategies can lower stroke risk a lot.
Lifestyle Modifications
Changing your lifestyle is key to preventing strokes. Eating well, staying active, keeping a healthy weight, and not smoking are important. A diet full of fruits, veggies, whole grains, and lean meats helps control blood pressure and cholesterol.
Exercise like walking, cycling, or swimming boosts heart health and lowers stroke risk. The American Heart Association suggests 150 minutes of moderate activity or 75 minutes of vigorous activity weekly.
Key Lifestyle Modifications:
- Eating a balanced diet
- Engaging in regular physical activity
- Maintaining a healthy weight
- Avoiding tobacco use
- Limiting alcohol consumption
Recognizing Stroke Symptoms and Emergency Response
Knowing and spotting stroke symptoms early can greatly help patients. Quick medical help is key to reduce brain damage and boost survival rates.
Importance of Immediate Medical Attention
Quick medical care is crucial when a stroke is suspected. The sooner a stroke victim gets help, the better their recovery chances. Giving clot-busting drugs quickly can greatly help ischemic stroke patients.
| Symptom | Action |
| Face Drooping | Call emergency services |
| Arm Weakness | Seek immediate medical help |
| Speech Difficulty | Do not delay; act quickly |
We stress the need to act fast when seeing stroke symptoms. Using the FAST method and knowing the need for quick medical help can greatly improve recovery chances for stroke victims.
“Time is brain” is a mantra used in the medical community to stress the importance of rapid response to stroke symptoms.
By spotting stroke symptoms and acting quickly, we can greatly improve patient outcomes. It’s vital that everyone knows how to identify a stroke and what to do next.
Conclusion
Knowing the main reasons for cerebrovascular accidents is key to preventing strokes and responding quickly. We’ve looked at how atherosclerosis, high blood pressure, and atrial fibrillation play a part. These factors can lead to a stroke.
It’s also important to know the signs of a stroke and act fast. Spotting the symptoms early and taking quick action can help avoid serious brain damage. This is crucial.
Preventing strokes is the best way to handle cerebrovascular accidents. Making healthy lifestyle choices and managing health conditions can lower stroke risk. We stress the importance of learning more about preventing strokes.
In summary, understanding the causes of cerebrovascular accidents and taking steps to prevent them is vital. We need to stay alert and take action to fight strokes. This is how we can make a difference.
FAQ
What is a cerebrovascular accident (CVA), and what are its main types?
A cerebrovascular accident, or stroke, happens when the brain doesn’t get enough oxygen and nutrients. This is because the blood supply to the brain is cut off or reduced. There are two main types: ischemic strokes, caused by a blockage, and hemorrhagic strokes, caused by bleeding.
What is atherosclerosis, and how does it lead to a stroke?
Atherosclerosis is when plaque builds up in arteries, narrowing or blocking them. This can lead to a stroke by cutting off blood flow to the brain. It can also cause blood clots to form, which can then travel to the brain.
What are the risk factors for ischemic strokes?
Risk factors for ischemic strokes include high blood pressure, irregular heartbeat, high cholesterol, diabetes, smoking, and being overweight. Changing your lifestyle and getting medical help can lower your risk.
How does hypertension contribute to the risk of stroke?
High blood pressure damages blood vessels, making them more likely to block or burst. It also increases the risk of heart disease, which can lead to blood clots causing a stroke.
What is the connection between atrial fibrillation and stroke risk?
Atrial fibrillation, or an irregular heartbeat, can cause blood clots in the heart. These clots can then travel to the brain and cause a stroke. Treating atrial fibrillation can help lower this risk.
What are the causes of hemorrhagic strokes?
Hemorrhagic strokes are usually caused by a burst aneurysm or arteriovenous malformation (AVM). This leads to bleeding in or around the brain.
How can modifiable risk factors be managed to reduce stroke risk?
Risk factors like smoking, diabetes, high cholesterol, and obesity can be managed. This includes eating healthy, exercising regularly, and quitting smoking. Medical treatments like medication and surgery also help.
What are non-modifiable risk factors for stroke?
Non-modifiable risk factors include age, gender, and genetics. Knowing these can help assess stroke risk and take preventive steps.
What is a transient ischemic attack (TIA), and what does it signify?
A TIA, or “mini-stroke,” is a temporary blockage of blood flow to the brain. It causes symptoms similar to a stroke. TIAs are warning signs of a more serious stroke and need immediate medical attention.
How can recognizing stroke symptoms promptly save lives?
Recognizing stroke symptoms early, using the FAST method, can save lives. The FAST method checks for Face drooping, Arm weakness, Speech difficulty, and Time to call for help. Quick action allows for timely treatment.
What are the latest advances in understanding stroke causes?
Recent research has improved our understanding of genetic and immune factors in stroke. These findings are leading to new ways to prevent and treat strokes.
What strategies can prevent cerebrovascular accidents?
Preventing strokes involves lifestyle changes like a healthy diet, exercise, not smoking, and stress management. Medical interventions like controlling blood pressure and heart disease, and using anticoagulants when needed, also play a role.