Many women worldwide face discomfort or cervix pain during sex. This pain, known as cervical dyspareunia, happens when the cervix is touched or pressed during deep penetration.
About 31 percent of women of reproductive age deal with pelvic pain. This can be a big worry. But, it’s good to know there are causes and treatments for this issue.
Understanding why you might feel cervical pain during intercourse is key. It could be due to inflammation, changes in the cervix, or other health issues. We’re here to help you find a way to feel better.
Key Takeaways
- Cervical dyspareunia affects a significant percentage of reproductive-age women.
- Deep penetration can cause discomfort or pain in the cervix.
- Identifying the causes is key for effective treatment.
- Various factors contribute to cervical pain during sex.
- Understanding the condition is the first step towards relief.
Understanding Cervical Dyspareunia

Cervical dyspareunia is a condition that causes pain in the cervix during sex. It affects women’s quality of life. Understanding this condition is key to easing the discomfort and pain it brings. We will look into what causes cervical dyspareunia and how common it is.
What Happens When the Cervix is Touched During Sex
Touching or hitting the cervix during sex can cause pain, if it’s inflamed or has structural changes. The cervix is very sensitive. Any irritation or abnormality can lead to pain during deep penetration. Collision dyspareunia, pain from the penis hitting the cervix, is common in these cases.
The pain from cervical dyspareunia can feel sharp or dull. It can be constant or only happen in certain positions or activities.
The Prevalence of Cervical Pain
Cervical pain during sex is more common than you might think. About 31 percent of reproductive-age women with pelvic pain have cervical tenderness. This shows how important it is to understand and tackle cervical dyspareunia.
Condition | Prevalence | Common Causes |
Cervical Dyspareunia | 31% of women with pelvic pain | Inflammation, structural changes |
Collision Dyspareunia | Common in deep penetration | Sexual positions, penis size |
By understanding cervical dyspareunia’s prevalence and causes, we can improve life for those affected.
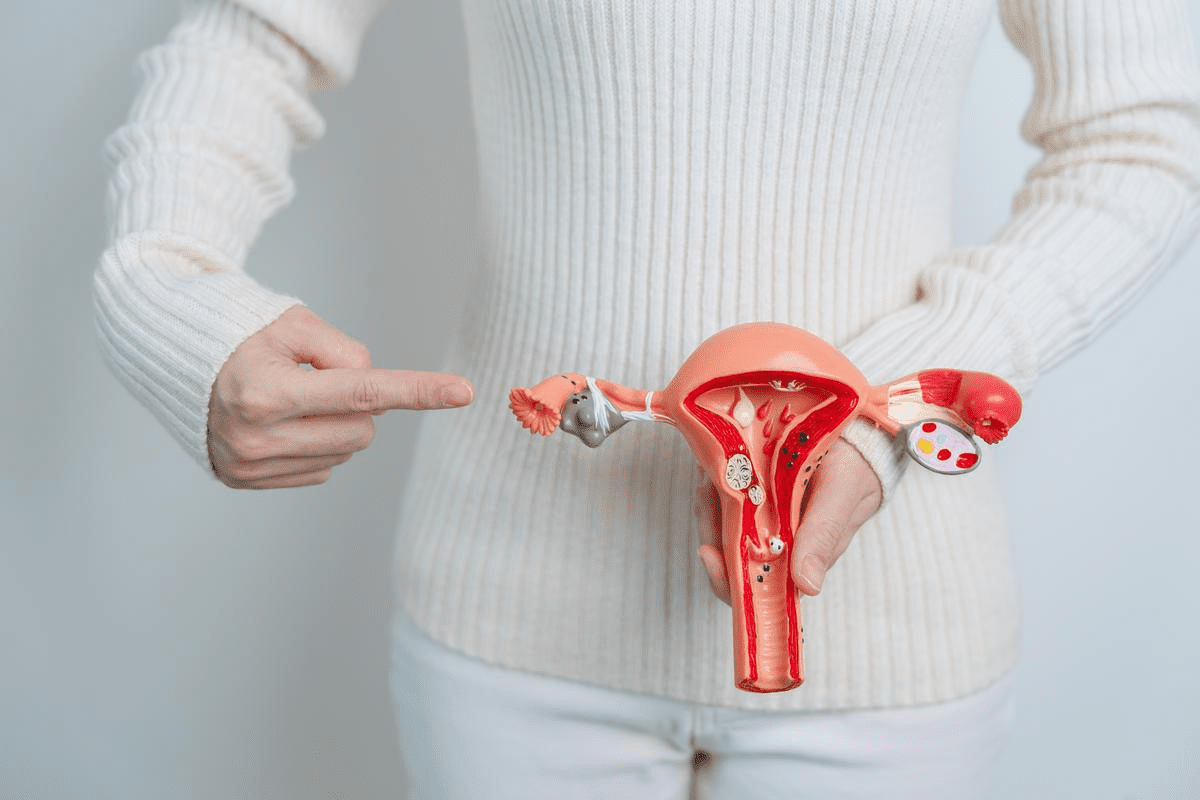
The Anatomy of the Cervix

The cervix is at the uterus’s lower end. It’s a key part of female reproductive anatomy. It connects the uterus to the vagina, playing a big role in reproductive health.
Location and Function of the Cervix
The cervix is at the uterus’s lower part, opening into the vagina. Its main job is to let menstrual blood flow from the uterus to the vagina. It also lets sperm into the uterus. During childbirth, it opens wide to let the baby pass through.
Cervical Function: The cervix makes mucus. This mucus changes throughout the menstrual cycle. It helps or blocks sperm entry, depending on the cycle’s phase.
Cervical Changes | Menstrual Cycle Phase | Function |
Mucus becomes more fluid | Approaching ovulation | Facilitates sperm entry |
Mucus becomes thicker | After ovulation | Blocks sperm entry |
How the Cervix Changes During Arousal
When sexually aroused, the cervix changes. It moves up and the os (the cervix’s opening) gets a bit wider. This can change its position and how sensitive it is.
Arousal Effects: More blood flow to the area makes the cervix move. This can make it more likely to be touched during deep penetration.
Individual Anatomical Variations
Every woman’s cervix is different. The length, shape, and position can vary. This affects how it feels during sex.
Variations: Some women have a longer or shorter cervix. It might be more forward or backward. This can change how likely it is to be touched during sex.
Knowing these differences and how they change with arousal helps understand cervical pain during sex.
Mechanics of Deep Penetration
Deep penetration can cause cervical pain during sex. This happens when the penis hits or presses on the cervix. This can lead to discomfort or pain.
How and Why the Cervix Gets Hit
The cervix is at the end of the vaginal canal. It’s a sensitive area. When it’s hit or pressed, it can hurt.
- The angle of penetration can influence the likelihood of cervical contact.
- The depth of penetration is a significant factor in determining whether the cervix will be hit.
- Individual anatomical variations can affect how the penis interacts with the cervix during sex.
Sexual Positions That Increase Cervical Contact
Certain sexual positions are more likely to result in cervical contact. This is because of the angle and depth of penetration they allow.
Some of these positions include:
- Missionary position with deep penetration.
- Positions where the legs are raised, allowing for deeper penetration.
- Positions that involve bending or arching, which can alter the angle of penetration.
Avoiding these positions or modifying them to reduce the depth of penetration can help minimize cervical pain.
The Role of Penis Size and Vaginal Depth
The size of the penis and the depth of the vagina can also play a role. A larger penis or a vagina with a shorter depth may increase the likelihood of cervical contact.
Understanding individual anatomical differences is key to addressing cervical pain.
By considering these factors and potentially adjusting sexual practices, individuals can work towards reducing cervical pain during sex.
Cervix Pain During Sex: Causes and Triggers
Cervix pain during sex can be very distressing. Finding out what causes it is the first step to feeling better. We know that cervix pain can show up in different ways and at different times. Here, we’ll look at the causes and triggers of cervical pain during sex.
Types of Pain Sensations
The pain from cervical contact during sex can be different for everyone. Some might feel a sharp, stabbing pain, while others might feel a dull ache or pressure. Knowing the type of pain helps figure out its cause.
The pain sensations can be grouped into a few types:
- Sharp or stabbing pain
- Dull ache or cramping
- Sensation of pressure or discomfort
Timing of Pain During Intercourse
When the pain happens during sex can give clues about its cause. Pain can happen at the start, during deep penetration, or after sex. We’ll look at how the timing of pain relates to different causes.
Pain during deep penetration might mean the cervix is being hit or pressed. Pain after sex could mean an infection or other condition.
Factors That Worsen Symptoms
Several things can make cervix pain worse during sex. These include certain sexual positions, the size and depth of the penis, and body shape. Also, medical conditions or infections can play a big role.
Knowing these factors is key to managing and possibly easing the pain. By tackling these issues, people can aim for a more comfortable and enjoyable sex life.
Medical Conditions Causing Cervical Pain
Cervical pain during sex can be linked to various medical conditions. These need to be diagnosed and treated properly. We’ll look at the different health issues that can cause this pain.
Infections: Cervicitis, Herpes, and Other STIs
Infections are a big reason for cervical pain. Cervicitis, an inflammation of the cervix, can be caused by STIs like chlamydia and gonorrhea. Herpes simplex virus can also cause pain, mainly during outbreaks. Other STIs, such as trichomoniasis and mycoplasma genitalium, can lead to discomfort.
If you’re experiencing persistent or severe pain, getting tested for STIs is key. Early diagnosis and treatment can ease symptoms and prevent complications.
Endometriosis and Adenomyosis
Endometriosis is when tissue like the uterus lining grows outside the uterus. This causes inflammation and scarring, leading to pain, mainly during menstruation or sex. Adenomyosis, where endometrial tissue grows into the uterine wall, can also cause pain.
Women with endometriosis are more likely to have cervical pain during sex. Managing these conditions can help reduce pain and improve life quality.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It can cause cervical pain and other symptoms. PID is often caused by untreated STIs and can lead to serious complications if not treated.
PID can cause scarring and adhesions in the reproductive organs. This can lead to chronic pain and discomfort during sex. It’s important to treat PID promptly to prevent damage and alleviate symptoms.
Fibroids and Pelvic Congestion Syndrome
Fibroids are non-cancerous growths in the uterus. They can cause cervical pain, heavy bleeding, and other symptoms. Large fibroids can put pressure on the cervix, leading to discomfort during sex.
Pelvic congestion syndrome is a condition with varicose veins in the pelvis. It can cause chronic pain and discomfort. This condition can contribute to cervical pain, mainly during or after sex.
Medical Condition | Symptoms | Treatment Options |
Cervicitis | Cervical pain, abnormal discharge | Antibiotics, antiviral medications |
Endometriosis | Cervical pain, pelvic pain, heavy bleeding | Hormonal therapies, surgery |
Pelvic Inflammatory Disease | Cervical pain, pelvic pain, fever | Antibiotics, hospitalization (in severe cases) |
Fibroids | Cervical pain, heavy bleeding, pelvic pressure | Surgery, hormonal therapies, uterine artery embolization |
Understanding the medical conditions behind cervical pain is key to managing it. By addressing these conditions, women can find relief and improve their quality of life.
“The key to managing cervical pain is identifying and treating the underlying medical conditions. With proper diagnosis and treatment, women can alleviate symptoms and improve their overall well-being.”
Medical Expert, OB-GYN Specialist
Structural and Physical Factors
Understanding the role of structural and physical factors is key to tackling cervical pain during sex. These elements can greatly affect the cervix’s sensitivity, leading to discomfort.
IUD Placement Issues
An intrauterine device (IUD) is a common birth control method. Yet, its placement can sometimes cause problems. If the IUD is not placed right, it can lead to pain during sex. Proper placement and regular check-ups are essential to avoid discomfort.
Post-Childbirth Changes
Childbirth can significantly alter the female body, including the cervix. Changes like scarring or structural changes can cause pain during sex. It’s essential for women to discuss any concerns with their healthcare provider after giving birth.
Surgical Scarring
Surgeries, like cesarean sections, can lead to scarring. This scarring can sometimes cause pain during sex. Proper post-operative care and follow-up can help minimize the risk of such complications.
Hormonal Influences on Cervical Sensitivity
Hormonal changes can affect cervical sensitivity. For example, changes in estrogen levels can impact the cervix’s sensitivity, leading to pain during sex. Understanding these hormonal influences can help in managing and treating cervical pain.
By addressing these structural and physical factors, we can better understand and manage cervical pain during sex. It’s vital to consult healthcare professionals for personalized advice and treatment.
Diagnosis Process for Cervical Pain
To find out why someone has cervical pain, doctors follow a specific process. This process is key to figuring out the cause and creating a good treatment plan.
Medical History and Physical Examination
The first step is to take a detailed medical history. Doctors ask about symptoms, sexual activity, menstrual cycle, and past surgeries or health issues. Then, they do a physical examination to check the patient’s health and find possible causes of cervical pain.
During the physical exam, doctors might do a pelvic exam. This is to look for any tenderness or lesions on the cervix and nearby areas.
Diagnostic Tests and Procedures
If the history and physical exam don’t give a clear answer, diagnostic tests might be needed. These can include:
- Pelvic ultrasound to look for any issues in the reproductive organs
- Laparoscopy to see inside the body and check for things like endometriosis
- Biopsy to examine tissue samples for abnormal cell growth or infection
These tests help doctors find the real cause of cervical pain.
Differential Diagnosis
A differential diagnosis is a big part of finding the cause. It’s about ruling out other conditions that might look like cervical pain. By looking at other possible causes, doctors can find the right diagnosis.
For example, conditions like pelvic inflammatory disease, endometriosis, or cervical stenosis can have similar symptoms. A differential diagnosis helps tell these apart.
Treatment Options and Pain Management
Managing cervical pain well means knowing the cause and using the right treatments. The treatment depends on the cause of the pain.
Medical Treatments for Underlying Conditions
First, treat the underlying condition causing the pain. For example, if it’s an infection like cervicitis, antibiotics or antiviral meds are used. If endometriosis is the cause, treatments might include hormones or surgery to remove lesions.
A study in the Journal of Minimally Invasive Gynecology shows laparoscopic surgery can greatly reduce pain in endometriosis patients.
“Laparoscopic excision of endometriosis has been shown to improve pain symptoms in a significant proportion of women.”
— Journal of Minimally Invasive Gynecology
Pain Relief Medications and Approaches
Medicines like ibuprofen or acetaminophen can help with cervical pain. Sometimes, stronger meds are needed. Also, methods like acupuncture or pelvic floor physical therapy can help.
Pain Relief Method | Description | Benefits |
Over-the-counter pain relievers | Medications like ibuprofen or acetaminophen | Easy to access, effective for mild to moderate pain |
Prescription pain medications | Stronger medications for severe pain | Effective for severe pain, can be tailored to individual needs |
Alternative therapies | Acupuncture, pelvic floor physical therapy | Non-pharmacological, can address underlying causes |
Physical Therapy and Pelvic Floor Exercises
Physical therapy, like pelvic floor therapy, is key in managing cervical pain. It includes pelvic floor rehabilitation and trigger point therapy. A physical therapist can create a custom exercise plan.
Hormonal Treatments When Applicable
For pain linked to hormonal issues like endometriosis, hormonal treatments work well. Options include birth control pills, gonadotropin-releasing hormone (GnRH) agonists, or other hormones that reduce menstrual cycles and pain.
Understanding and treating the cause of cervical pain can greatly improve life quality. It’s important to work with healthcare providers to find the best treatment.
Prevention and Coping Strategies
Managing cervical pain during sex involves smart sexual positions, talking openly with your partner, and proper arousal. These strategies can greatly reduce discomfort and make sex better for you.
Sexual Positions That Minimize Cervical Contact
Some sex positions can reduce cervix contact and pain. For example, being on top gives you control over how deep you go. Try different angles and depths to find what feels best for you.
Communication Techniques With Your Partner
Talking openly with your partner is key to managing cervical pain. Share what feels good and what doesn’t. Use “I” statements to express your feelings without blaming.
Proper Lubrication and Arousal
Good lubrication is vital for comfortable sex. A high-quality lubricant can cut down on friction and make sex more enjoyable. Also, getting properly aroused before sex can help the vagina accept the penis better, reducing pain.
Timing Intercourse With Your Menstrual Cycle
Cervical pain might change with your menstrual cycle. Knowing how your cycle affects you can help plan sex better. Keep a menstrual diary to spot any patterns in pain.
Using these strategies can help you manage cervical pain during sex. It can also improve your overall well-being.
Conclusion
Understanding cervical pain during sex is key for those who feel discomfort or pain. We’ve looked at why cervical pain happens, how to diagnose it, and how to treat it. We’ve learned about the cervix’s anatomy and how deep penetration can cause pain.
We’ve talked about how medical issues like infections and endometriosis can cause pain. We’ve also discussed how physical changes, like IUDs and post-childbirth, can lead to pain. The diagnosis process involves looking at your medical history, doing a physical exam, and running tests.
We’ve covered many ways to manage cervical pain, like treating underlying conditions and using pain relief. We’ve also talked about physical therapy, hormonal treatments, and how to prevent pain. This includes changing sexual positions, talking to your partner, and using lubrication.
In summary, cervical pain during sex is a complex issue that needs a detailed approach to solve. By understanding the causes and using the right treatments, people can feel better and live a better life. This gives a clear overview of cervical pain during sex.
FAQ
Does hitting the cervix during sex hurt?
Hitting the cervix can hurt for some, but not for others. It depends on many things, like how your body is made and any health issues you might have.
Why does my cervix hurt when I have sex?
There are many reasons why your cervix might hurt during sex. It could be because of how deep you’re going, health problems like infections, or how your body is shaped.
What are the causes of cervical pain during intercourse?
Cervical pain can come from infections, like cervicitis, or health issues like endometriosis. It can also be caused by pelvic inflammatory disease, fibroids, or pelvic congestion syndrome.
How is cervical pain during sex diagnosed?
Doctors will first ask you about your health and then do a physical check. They might also do tests to find out why you’re in pain.
What treatment options are available for managing cervical pain?
Doctors can treat the cause of your pain with medicine or surgery. They might also suggest pain relief, physical therapy, or hormonal treatments.
Can changing sexual positions help reduce cervical pain?
Yes, choosing positions that don’t put pressure on your cervix can help. Trying different ways can help you find what feels best.
How can I communicate with my partner about cervical pain during sex?
Talking openly with your partner is important. Tell them about your pain and try new positions or ways together. This can make sex better for both of you.
Does proper lubrication and arousal help with cervical pain during sex?
Yes, using the right lubricant and getting turned on can make sex more comfortable. This includes reducing cervical pain.
Can timing intercourse with my menstrual cycle help with cervical pain?
For some, timing sex with their cycle can help with pain. This is because some conditions might be worse at certain times.
Is it normal to experience pain when the cervix is hit during sex?
Some discomfort is okay, but if the pain is bad or lasts, you should talk to a doctor. They can check for any health problems.
Can an IUD cause cervical pain during sex?
Sometimes, an IUD can cause discomfort or pain, including cervical pain. But this is rare for most people using them.
How do hormonal influences affect cervical sensitivity?
Hormones can change how sensitive your cervix is. Some people might feel more pain or discomfort at certain times in their cycle or because of hormonal issues.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2080987/