Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 70% of breast cancer patients have a lumpectomy. This surgery removes the tumor and some surrounding tissue. But what happens next? Many wonder if chemotherapy is needed after a lumpectomy.
The path through breast cancer treatment is complex and emotionally tough. Whether chemotherapy is needed varies. It depends on the cancer’s stage, its characteristics, and the patient’s health.
Key Takeaways
- Chemotherapy after a lumpectomy is not always required.
- The decision to undergo chemotherapy depends on the cancer’s stage and characteristics.
- Understanding individual circumstances is key in deciding on chemotherapy.
- The recovery from a lumpectomy affects treatment planning.
- Patients should talk to their healthcare provider about their situation.
Understanding Lumpectomy as a Breast Cancer Treatment
When breast cancer is diagnosed, many patients think about lumpectomy. This surgery removes the tumor. It aims to keep the breast looking and working like before.
What is a lumpectomy procedure?
Lumpectomy is done under general or local anesthesia. The surgeon cuts into the breast to find and remove the tumor. They also take some healthy tissue around it.
Then, they check the removed tissue for cancer cells. If there are none, radiation therapy follows. This helps kill any cancer left in the breast.
Differences between lumpectomy and mastectomy
Lumpectomy and mastectomy differ in how much tissue is removed. Lumpectomy takes out the tumor and a bit of healthy tissue. Mastectomy removes one or both breasts.
Lumpectomy is for early-stage breast cancer. It’s for tumors that are small and in one place.
Procedure | Tissue Removed | Typical Use |
Lumpectomy | Tumor and margin of healthy tissue | Early-stage breast cancer |
Mastectomy | One or both entire breasts | More advanced breast cancer or larger tumors |
Benefits and limitations of lumpectomy
Lumpectomy keeps the breast looking good and is less invasive. It might have fewer complications. But, it’s not right for everyone, like those with big tumors or more than one tumor.
Also, it often needs radiation therapy. This can make treatment longer and cause more side effects.
In summary, lumpectomy is a good choice for many with early-stage breast cancer. Knowing about it, its differences from mastectomy, and its pros and cons helps in making the right decision.
The Basics of Chemotherapy in Breast Cancer Treatment
Chemotherapy is a treatment that fights cancer cells all over the body. It’s a key part of breast cancer care after a lumpectomy. This treatment uses drugs to kill or slow down cancer cells.
How Chemotherapy Works Against Cancer Cells
Chemotherapy targets fast-growing cells, like most cancer cells. The drugs used in this treatment mess with the cancer cells’ growth. This helps lower the chance of cancer coming back after a lumpectomy.
Chemotherapy drugs can be given in different ways. They can be injected, taken by mouth, or given through an IV. The method depends on the drug and the patient’s needs.
Types of Chemotherapy Drugs Used After Lumpectomy
Many chemotherapy drugs are used after a lumpectomy. These include:
- Anthracyclines, like doxorubicin, which damage cancer cells’ DNA.
- Taxanes, such as paclitaxel, which mess with the microtubules needed for cell division.
- Cyclophosphamide, often used with other drugs.
The choice of chemotherapy depends on the cancer’s stage and type, and the patient’s health.
Timing of Chemotherapy (Neoadjuvant vs. Adjuvant)
Chemotherapy can be given at different times. Neoadjuvant chemotherapy is given before surgery to make the tumor smaller. Adjuvant chemotherapy is given after surgery to kill any remaining cancer cells.
Choosing between neoadjuvant or adjuvant chemotherapy depends on the tumor’s size and type, and the patient’s health and wishes.
Chemo Requirement After Lumpectomy: The Complete Picture
Deciding on chemotherapy after a lumpectomy is complex. It’s influenced by past treatments, current guidelines, and the patient’s situation. Understanding the data, treatment history, and current rules is key.
Statistics on Chemotherapy Use Following Lumpectomy
Chemotherapy use after a lumpectomy changes based on several factors. These include the cancer’s stage, the patient’s age, and the tumor’s type. Recent chemotherapy statistics show many patients get chemotherapy, but this number is going down. This is thanks to new targeted therapies and personalized medicine.
Others got radiation or hormone therapy instead.
Evolution of Treatment Protocols Over Time
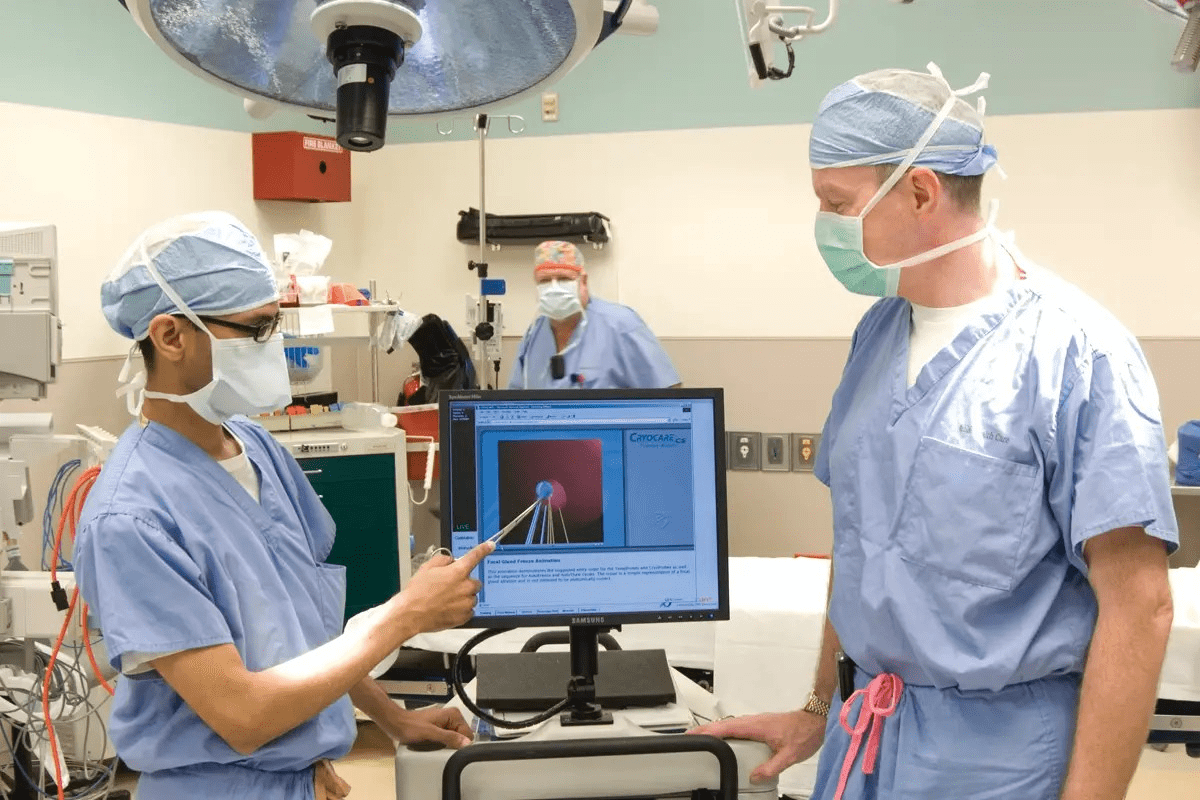
Breast cancer treatments have changed a lot over the years. This is due to new research, clinical trials, and medical tech advancements. In the past, chemotherapy was often used after a lumpectomy. But now, treatments are more tailored to each patient.
An oncologist noted, “Treatment plans have become more personalized. Chemotherapy is now based on the patient’s risk and tumor type.” This change is thanks to more use of genomic testing.
“The future of breast cancer treatment lies in precision medicine, where therapies are targeted to the specific characteristics of each patient’s cancer.”
Current Guidelines for Post-Lumpectomy Chemotherapy
Current chemotherapy guidelines suggest a team approach to treatment planning. This includes surgeons, medical oncologists, and radiation oncologists. The decision to use chemotherapy after a lumpectomy depends on several factors. These include the cancer’s stage, grade, hormone receptor status, and HER2 status.
The National Cancer Network (NCCN) says chemotherapy is often needed for high-risk patients. This includes those with big tumors, positive lymph nodes, or aggressive tumors. But for those with low-risk features, hormone therapy might be an option.
- Chemotherapy is frequently recommended for patients who have high-grade tumors or positive lymph nodes, which helps to ensure a more effective treatment strategy.
- Hormone receptor-positive patients may benefit from hormone therapy.
- HER2-positive patients may receive targeted therapies.
Early-Stage Breast Cancer: When Chemotherapy Might Be Optional
For those with early-stage breast cancer, the need for chemotherapy isn’t always clear. New research has helped us understand when it’s really needed.
Stage I Breast Cancer Treatment Approaches
Stage I breast cancer has small tumors and no lymph node involvement. Treatments often include surgery and radiation. Whether to use chemotherapy depends on the tumor and the patient’s health.
Low-Risk Characteristics That May Avoid Chemotherapy
Some low-risk traits might mean no chemotherapy is needed. These include:
- Tumors that are small (less than 1 cm) and have favorable biological features.
- Cancers that are hormone receptor-positive and HER2-negative.
- Patients with no lymph node involvement.
Genomic testing, like Oncotype DX, can help find who can skip chemotherapy.
Research Supporting Omission of Chemotherapy in Select Cases
Studies have shown that in some cases, chemotherapy isn’t needed. For example, in low-risk, hormone receptor-positive breast cancer, chemotherapy might not add much benefit. Treatment should be tailored to each patient’s needs.
Knowing your cancer’s specifics and talking to your doctor can help you decide on treatment. This might mean avoiding chemotherapy.
Factors That Determine If Chemotherapy Is Needed
Deciding on chemotherapy involves looking at several things. This includes the cancer’s stage and how it behaves. When thinking about chemotherapy after a lumpectomy, certain key points are checked.
Cancer Stage and Grade Considerations
The stage and grade of cancer are very important. Cancer stage tells us about the tumor’s size and if it has spread. Early stages (Stage I and some Stage II) might not need chemotherapy. But, more advanced stages often do.
The cancer grade shows how much the tumor cells look like normal cells. High-grade tumors, which look less like normal cells, often need chemotherapy. This is because they grow quickly and aggressively.
Tumor Characteristics That Influence Treatment Decisions
Tumor characteristics are also key in deciding on chemotherapy. Things like tumor size, if it has spread to lymph nodes, and certain receptors are looked at. For example, big tumors or those with aggressive features might need chemotherapy to lower the chance of coming back.
Molecular and Genetic Markers
Molecular and genetic markers give more info for making treatment choices. Tests like Oncotype DX look at the tumor’s genes to see if chemotherapy will help. Genetic markers like BRCA1 and BRCA2 can also change treatment plans. They might show a higher risk of cancer coming back or the benefit of certain treatments.
By looking at cancer stage and grade, tumor features, and genetic markers, doctors can decide if chemotherapy is right after a lumpectomy.
The Role of Tumor Size in Chemotherapy Decisions
Understanding how tumor size affects chemotherapy choices is key for patients. Oncologists look at tumor size when deciding if chemotherapy is needed after a lumpectomy.
Small Tumors and Chemotherapy Necessity
Deciding on chemotherapy for small tumors is complex. Small tumors are usually under 1 cm. Early detection and small size might mean no chemotherapy is needed, depending on other factors.
Studies show that for some with small, hormone-positive cancers, chemotherapy’s benefits are small. Genomic tests, like Oncotype DX, can help figure out if chemotherapy will help.
When Larger Tumors Typically Require Chemotherapy
Larger tumors, over 2 cm, often need aggressive treatment, including chemotherapy. The bigger the tumor, the higher the risk of cancer spreading. Chemotherapy can help lower this risk.
Other tumor traits, like grade and hormone receptor status, also play a role. For example, a big tumor that’s hormone-positive might do well with hormone therapy, possibly avoiding chemotherapy.
Borderline Cases and Decision Factors
Tumors between 1 and 2 cm pose a tough decision on chemotherapy. These borderline cases need careful thought of many factors, like tumor grade and lymph node status.
Oncologists use a team approach to make these decisions. They consider input from various fields and use genomic tests for more insight into chemotherapy’s benefits.
Tumor Size | Chemotherapy Consideration | Other Factors |
<1 cm | Less likely necessary | Tumor grade, hormone receptor status |
1-2 cm | Decision based on multiple factors | Lymph node status, genomic testing |
>2 cm | More likely recommended | Tumor characteristics, patient health |
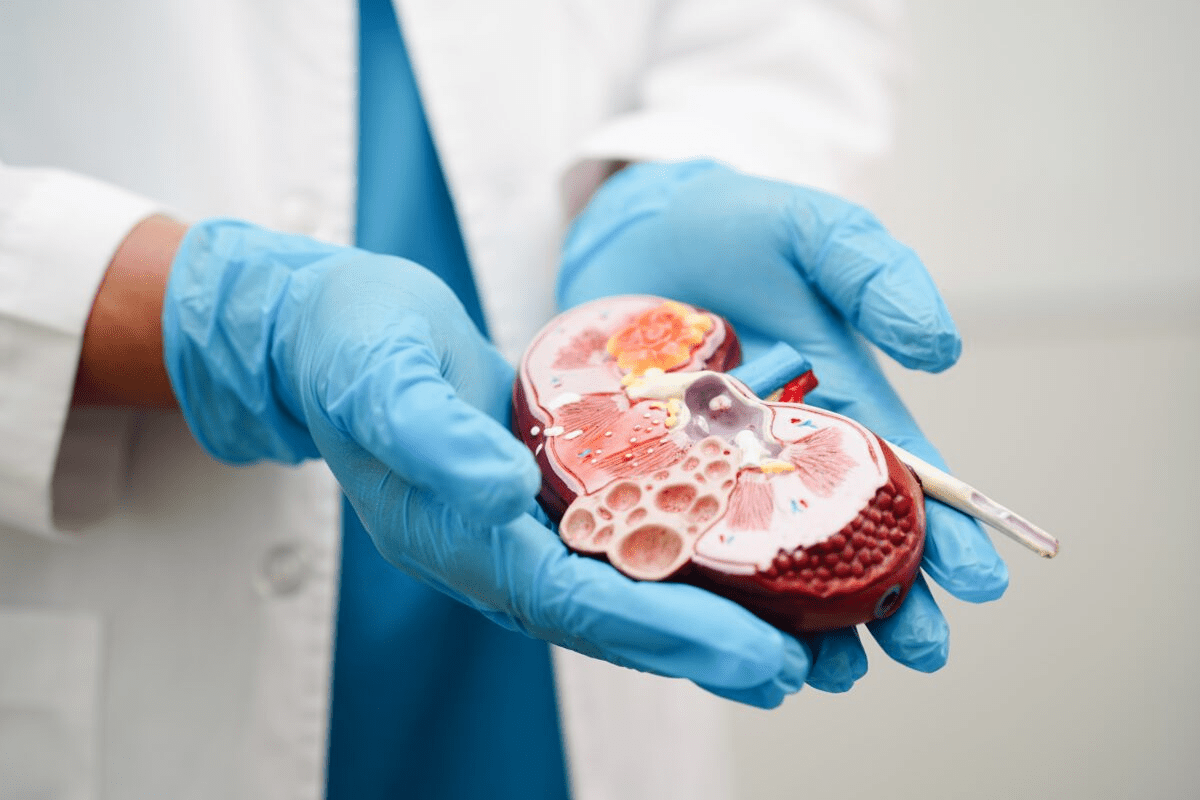
Lymph Node Status and Its Impact on Treatment Plans
Lymph nodes are small, bean-shaped structures in the body’s lymphatic system. They help fight infection and disease. The status of these nodes is key in deciding treatment after a lumpectomy.
Significance of Positive Lymph Nodes
When cancer is found in lymph nodes, it’s called “positive” or “involved.” This means cancer has spread beyond the original site. This info is vital for cancer staging and treatment planning.
Positive lymph nodes are a big deal. They can mean you might need chemotherapy after a lumpectomy. The more nodes involved, the higher the risk of cancer spreading.
Sentinel Lymph Node Biopsy and Its Role
A sentinel lymph node biopsy finds the first node cancer cells spread to. This node is called the sentinel node. It’s removed and checked for cancer cells.
- This biopsy helps see if cancer has spread.
- It might avoid more extensive lymph node removal.
- It’s key for staging and treatment planning.
How Many Affected Nodes Typically Trigger Chemotherapy Recommendation
The number of cancer-positive lymph nodes affects treatment. Generally, more nodes mean more likely chemotherapy.
- No involved nodes might not need chemotherapy, depending on the tumor.
- One to three positive nodes might or might not need chemotherapy, based on tumor size and grade.
- Four or more positive nodes usually mean chemotherapy is recommended due to higher recurrence risk.
Knowing about your lymph nodes and their impact on treatment is important. Your healthcare team will talk about these details with you. They’ll help decide the best treatment for you.
Hormone Receptor Status and Treatment Decisions
Knowing the hormone receptor status of a breast cancer tumor is key for the best treatment. The status of estrogen and progesterone receptors helps decide if chemotherapy is needed.
Estrogen and Progesterone Receptor Positive Cancers
Cancers with estrogen or progesterone receptors use these hormones to grow. Tumors with these receptors are often treated with hormone therapy. This therapy blocks hormones from reaching cancer cells. It works well for ER-positive or PR-positive cancers.
HER2 Status and Its Influence on Chemotherapy Decisions
The HER2 gene is also important in breast cancer treatment. HER2-positive cancers grow faster because of too much HER2 gene. Knowing the HER2 status helps decide if targeted therapies are needed. Patients with HER2-positive cancers might also need chemotherapy.
Triple-Negative Breast Cancer and Chemotherapy Necessity
Triple-negative breast cancer (TNBC) doesn’t have estrogen, progesterone receptors, or too much HER2. It grows and spreads quickly. Chemotherapy is often the main treatment for TNBC because other therapies don’t work. Knowing about TNBC is important for treatment choices.
Healthcare providers use hormone and HER2 status to tailor treatments. This personalized approach helps decide if chemotherapy is needed. It ensures treatments fit each patient’s cancer best.
Genomic Testing to Guide Chemotherapy Decisions
Genomic tests, like Oncotype DX, are key in deciding if chemotherapy is needed after a lumpectomy. They look at the tumor’s genes to see if cancer might come back and if chemo will help.
Oncotype DX and Other Genomic Tests
Oncotype DX is a top choice for early-stage breast cancer. It checks 21 genes in the tumor to give a recurrence score. This score shows how likely cancer is to come back. Tests like MammaPrint and EndoPredict also help predict this risk.
How Recurrence Scores Influence Treatment Recommendations
The score from tests like Oncotype DX is key in deciding treatment. A low score means chemo might not help much. But a high score suggests chemo could lower the risk of cancer coming back.
- A low score might mean skipping chemo.
- A high score usually means chemo is recommended.
- Intermediate scores need more talk between the patient and doctor.
Limitations of Genomic Testing
Genomic testing has changed how we plan breast cancer treatment. But, it’s not for everyone. The results must be seen with other health factors in mind. Also, these tests can be expensive, and not all insurance covers them.
Age and Health Considerations in Chemotherapy Decisions
When deciding on chemotherapy after a lumpectomy, age and health are key. These factors help doctors create treatment plans that fit each patient’s needs.
Treatment Approaches for Younger Patients
Younger patients often want to keep their fertility and quality of life. We think about how chemotherapy might affect them, like causing early menopause or fertility problems. Preserving fertility might mean talking about freezing eggs before starting treatment.
Younger people usually handle chemotherapy better than older ones. But we also look at the cancer and the patient’s health to choose the right treatment.
Special Considerations for Elderly Patients
Elderly patients have unique challenges with chemotherapy, like other health issues and less energy. We do a detailed geriatric assessment to help decide on treatment.
Patients with heart disease or diabetes face extra challenges with chemotherapy. We work with patients and their caregivers to find a balance between fighting cancer and avoiding treatment risks.
How Existing Health Conditions Affect Chemotherapy Decisions
Health conditions are very important in choosing chemotherapy. We check how these conditions might affect how well a patient can handle chemotherapy. For example, those with heart disease might need different treatments to avoid heart problems.
By looking at age, health, and current conditions, we create a treatment plan that works best for each patient. This way, chemotherapy decisions are made with the patient’s best interests in mind.
Alternative Treatments to Chemotherapy After Lumpectomy
After a lumpectomy, patients often think about more treatments to lower cancer risk. Chemotherapy is common, but other therapies are also key in care.
Radiation Therapy as a Standard Companion Treatment
Radiation therapy is often suggested after lumpectomy. It aims to kill any cancer cells left in the breast. This treatment uses high-energy rays to target and destroy cancer cells, given over weeks. It helps avoid more surgery or treatments.
Hormone Therapy Options and Effectiveness
Hormone therapy is good for hormone receptor-positive breast cancer. Hormone therapy blocks the body’s natural hormones, like estrogen and progesterone, from reaching cancer cells. This slows or stops cancer growth. Tamoxifen and aromatase inhibitors are common hormone therapies.
- Tamoxifen is used in premenopausal women to block estrogen receptors.
- Aromatase inhibitors are for postmenopausal women to lower estrogen production.
Hormone therapy can be used alone or with other treatments. Its success depends on the cancer’s hormone receptor status and the patient’s menopausal status.
Targeted Therapies as Alternatives or Complements
Targeted therapies are for certain breast cancers. They target specific characteristics of cancer cells, such as proteins that signal cancer cells to divide. For example, HER2-positive breast cancers are treated with trastuzumab (Herceptin).
Targeted therapies can be used with chemotherapy, hormone therapy, or radiation therapy. They offer a tailored approach to treatment, focusing on the cancer’s unique traits.
In conclusion, while chemotherapy is common after lumpectomy, other treatments like radiation, hormone therapy, and targeted therapies are also vital. The right treatment depends on the cancer’s stage and type, and the patient’s health.
Radiation Therapy: Almost Always Required After Lumpectomy
Radiation therapy is a key part of breast cancer treatment after a lumpectomy. It helps get rid of any cancer cells left behind. This lowers the chance of cancer coming back.
Why Radiation is Standard Following Lumpectomy
Radiation therapy is often needed after a lumpectomy. It helps prevent cancer from coming back in the same breast. Without it, the risk of cancer returning is higher.
Key Benefits of Radiation Therapy:
- Reduces the risk of local recurrence
- Preserves the breast
- Effective in eliminating microscopic cancer cells
Radiation Protocols and Timeframes
Radiation therapy starts a few weeks after surgery. This is when the wound has healed. It involves daily treatments, Monday through Friday, for several weeks.
Radiation Protocol | Description | Duration |
Whole Breast Irradiation (WBI) | Radiation to the entire breast | 3-6 weeks |
Partial Breast Irradiation (PBI) | Radiation to the area around the tumor | 1-2 weeks |
New methods have made treatments shorter. For example, hypofractionated radiation therapy can be done in less time.
Rare Exceptions When Radiation Might Be Omitted
In some rare cases, radiation therapy might not be needed. This includes very elderly patients or those with small, low-grade tumors. It depends on other risk factors too.
Talking to a healthcare provider is key to figuring out the right treatment plan.
Clinical Trials and Emerging Approaches in Post-Lumpectomy Treatment
Clinical trials are leading the way in finding new treatments for breast cancer after lumpectomy. They look for alternatives to traditional chemotherapy. As research grows, we’re moving towards treatments that are more tailored and effective.
Current Clinical Trials Investigating Chemotherapy Alternatives
Many clinical trials are looking into new ways to treat breast cancer. They aim to reduce or replace chemotherapy with more focused therapies. For example, some studies are checking if immunotherapy can help fight cancer cells. Others are looking at combining treatments to get better results with less harm.
Examples of ongoing clinical trials include:
- Trials investigating the use of PARP inhibitors in patients with BRCA1/2 mutations.
- Studies comparing the effectiveness of different chemotherapy regimens.
- Research into the role of CDK4/6 inhibitors in hormone receptor-positive breast cancer.
De-escalation of Treatment: The Trend Toward Less Chemotherapy
There’s a growing trend to use less treatment in breast cancer. This is to reduce side effects while keeping cancer under control. It’s most relevant for early-stage cancer or tumors with good biological characteristics.
De-escalation Strategy | Potential Benefits | Current Status |
Omitting chemotherapy in low-risk patients | Reduced toxicity, improved quality of life | Being investigated in several clinical trials |
Using targeted therapies instead of chemotherapy | More precise treatment, potentially fewer side effects | Promising results in early-stage trials |
Reducing the intensity of radiation therapy | Less damage to healthy tissues, reduced long-term risks | Ongoing research to determine optimal protocols |
How to Find and Participate in Clinical Trials
For those interested in clinical trials, there are many resources. The National Cancer Institute’s Clinical Trials Database lists trials in the U.S. Many cancer centers and hospitals also have their own trial programs.
To join a clinical trial, patients must meet certain criteria. This includes the cancer’s stage and type, overall health, and previous treatments.
The Decision-Making Process: Working With Your Oncology Team
When you get a breast cancer diagnosis, working with your oncology team is key. They help you make treatment choices that fit you best. Your team includes many specialists who work together to care for you.
The Multidisciplinary Approach to Treatment Planning
A team approach is vital in treating breast cancer. Your team might include surgeons, medical oncologists, and others. Each specialist adds their expertise to your care.
The surgeon will talk about surgery options with you. The medical oncologist will explain chemotherapy and other treatments. The radiation oncologist will discuss radiation therapy. This teamwork ensures your treatment fits your needs perfectly.
Questions to Ask Your Oncologist About Chemotherapy
When talking to your oncologist about chemotherapy, ask important questions. Ask about benefits, risks, side effects, and alternatives. This helps you understand your options better.
- What is the goal of chemotherapy in my treatment plan?
- How will chemotherapy be administered, and how often will I need to undergo treatment?
- What are the possible long-term effects of chemotherapy?
These questions help you make choices that match your values and preferences.
Getting Second Opinions on Treatment Recommendations
Getting a second opinion can offer new insights and peace of mind. It’s a common practice, and very helpful if you’re unsure. Your primary oncologist can suggest who to see for a second opinion.
Bring all your medical records and test results when you get a second opinion. This gives the specialist a full view of your case. Don’t be shy to ask questions and share your concerns. A second opinion can be a big step in feeling sure about your treatment.
Psychological Aspects and Coping With Treatment Decisions
The emotional impact of a breast cancer diagnosis is huge. It affects how patients make treatment choices and their overall happiness. Going through diagnosis and treatment is tough, needing medical care and emotional support.
Managing Anxiety About Treatment Choices
It’s key to manage anxiety when facing breast cancer treatment. Talking openly with healthcare providers can lessen fear and uncertainty. Patients should ask about treatment options, like chemotherapy, to make choices that fit their values.
Mindfulness and relaxation techniques also help with anxiety. Activities like meditation, deep breathing, and yoga can reduce stress and improve well-being.
Support Resources for Patients Facing Chemotherapy Decisions
Support from loved ones and groups is essential for emotional health during treatment. Support groups, online or in-person, let patients share and learn from others. It’s a great way to find strength in shared experiences.
Cancer centers also offer psychological support services like counseling. These services are key for emotional support and coping strategies.
Balancing Quality of Life with Treatment Effectiveness
It’s important to balance treatment success with quality of life. While treatment aims to cure cancer, keeping the patient’s life quality is also key. Treatment planning should consider side effects and their daily life impact.
Talking about quality of life concerns with doctors helps make better treatment choices. These choices aim to cure cancer and protect the patient’s physical and emotional health.
Conclusion: Making Informed Decisions About Your Breast Cancer Treatment
Understanding your breast cancer treatment options is key. This article has covered many aspects, like chemotherapy after a lumpectomy. We also talked about factors that affect treatment choices and alternative therapies.
Knowing your cancer’s details is vital. This includes tumor size, lymph node status, and hormone receptor status. These details help choose the best treatment for you. Talking about these with your oncology team is important.
The aim is to help you feel confident in your treatment choices. By staying informed and working with your healthcare team, you can make decisions that fit your needs. This ensures the best results in your breast cancer treatment.
FAQ
Do all patients need chemotherapy after a lumpectomy?
No, not all patients need chemotherapy after a lumpectomy. It depends on the cancer stage, tumor characteristics, and genetic markers.
What factors determine if chemotherapy is needed after a lumpectomy?
Decisions on chemotherapy are based on several factors. These include cancer stage, tumor size, and lymph node status. Hormone receptor status, HER2 status, and genetic testing results also play a role.
How does tumor size impact chemotherapy decisions?
Tumor size is a key factor in deciding on chemotherapy. Larger tumors often need chemotherapy, while smaller ones might not. The decision for borderline cases depends on other factors.
What is the significance of lymph node status in breast cancer treatment?
Lymph node status is very important in breast cancer treatment. Positive nodes mean a higher risk of cancer spreading. The number of affected nodes helps decide on chemotherapy.
How does hormone receptor status affect treatment decisions?
Hormone receptor status and HER2 status are important in treatment decisions. Hormone-positive cancers may get hormone therapy. HER2-positive cancers might need targeted therapies.
What is the role of genomic testing in guiding chemotherapy decisions?
Genomic testing, like Oncotype DX, helps decide on chemotherapy. It gives recurrence scores that show the risk of cancer coming back. This helps tailor treatment plans.
Are there alternative treatments to chemotherapy after lumpectomy?
Yes, there are alternatives to chemotherapy after a lumpectomy. These include radiation therapy, hormone therapy, and targeted therapies. The choice depends on individual circumstances.
Is radiation therapy always required after lumpectomy?
Radiation therapy is usually needed after a lumpectomy to kill any remaining cancer cells. But, there are rare exceptions. The decision is made on a case-by-case basis.
How can patients find and participate in clinical trials?
Patients can find and join clinical trials by talking to their oncologist or searching online. They can also contact research institutions. Clinical trials offer new treatments and options.
What role does the oncology team play in the decision-making process?
The oncology team is key in making treatment decisions. They guide on options, discuss risks and benefits, and help patients make informed choices.
How can patients cope with the psychological aspects of treatment decisions?
Patients can manage the psychological aspects by dealing with anxiety and using support resources. It’s important to balance quality of life with treatment effectiveness. Support from family, friends, and healthcare professionals is vital.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7538693/