Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 1 in 8 women will get breast cancer in their lifetime. It’s a big health worry. For many, a lumpectomy is a key step in treatment. Then, chemotherapy follows to kill all cancer cells. An expert guide to the chemo timeline after lumpectomy. Understand when it starts, how it’s scheduled, and critical factors that affect it.
Knowing Understanding the chemotherapy schedule after breast cancer surgery is crucial for patients. The timing of chemotherapy changes based on several things. These include the cancer’s stage and the patient’s health.
We’ll help you understand what to expect with lumpectomy recovery time and chemotherapy. We aim to make this tough journey easier for you.
Key Takeaways
- Chemotherapy after a lumpectomy is a common treatment for breast cancer.
- The timing of chemotherapy depends on various factors, including cancer stage and patient health.
- Understanding the post lumpectomy chemotherapy schedule can help patients prepare.
- Lumpectomy recovery time can influence when chemotherapy begins.
- Patients should discuss their chemotherapy timeline with their healthcare provider.
The Breast Cancer Treatment Sequence
After a lumpectomy, patients often wonder about the next steps in their breast cancer treatment plan. Knowing the sequence of treatments can ease anxiety and prepare patients for what’s next.
The Role of Lumpectomy in Breast Cancer Treatment
A lumpectomy is a surgical procedure that removes the cancerous tumor along with some surrounding tissue, striving to preserve as much breast tissue as possible. The success of a lumpectomy is often followed by other treatments to make sure all cancer cells are gone.
Lumpectomy Follow-up Treatments: After a lumpectomy, treatments like chemotherapy, radiation therapy, or hormone therapy might be needed. This depends on the cancer’s stage and type.
Where Chemotherapy Fits in the Treatment Plan
Chemotherapy is a treatment that uses drugs to kill cancer cells. It can be given before surgery (neoadjuvant chemotherapy) to shrink tumors or after surgery (adjuvant chemotherapy) to kill any remaining cancer cells. The timing of chemotherapy depends on the cancer’s stage, the patient’s health, and the surgery type.
Treatment Stage | Purpose | Timing |
Neoadjuvant Chemotherapy | Shrink tumors before surgery | Before lumpectomy |
Adjuvant Chemotherapy | Kill remaining cancer cells | After lumpectomy |
Knowing where chemotherapy fits in the treatment sequence helps patients prepare for their journey. The timing and type of chemotherapy are tailored to each patient’s needs and cancer type.
Chemo Timeline After Lumpectomy: Standard Practices
After a lumpectomy, patients usually wait 2-6 weeks before starting chemotherapy. This time is key for healing and reducing risks. It makes sure the patient is ready for the next treatment steps.
The Typical 2-6 Week Waiting Period
The oncologist decides when to start chemotherapy. They look at the patient’s health and how they’re recovering. The 3-6 week wait lets the body heal from surgery.
This healing time makes it easier to handle chemotherapy. It helps reduce swelling and pain. This makes the treatment more manageable.
Though this time varies, 2-6 weeks is the usual range. It helps oncologists plan the chemotherapy schedule. This range is based on the surgery’s extent and the patient’s health.
Why Timing Matters for Treatment Effectiveness
Starting chemotherapy too soon can lead to more side effects. Waiting too long might let cancer cells grow. This could make the treatment less effective.
The oncologist sets the chemotherapy schedule based on the patient’s specific condition and the pathology report results. This approach makes treatment more effective. It aims to kill cancer cells while keeping side effects low.
Waiting 2-6 weeks after a lumpectomy is a good balance. It allows for healing and starts chemotherapy when it’s most effective. This balance is key for a successful treatment plan.
Post-Lumpectomy Recovery Milestones
The journey to recovery after a lumpectomy is key in deciding the next steps in breast cancer treatment. As patients get better, they reach milestones that show they’re ready for the next treatment. This might include chemotherapy.
First Week After Surgery: Initial Healing
In the first week after a lumpectomy, the main goal is to heal. Patients are told to rest and not do too much. It’s important to watch for signs of infection, like redness, swelling, or fever. Managing pain is also a big part, with medicine to keep discomfort down.
Weeks 2-3: Preparing for Next Treatment Steps
By weeks 2-3, patients start getting ready for the next part of their treatment. They have follow-up visits with their healthcare team to check on healing. They also learn what to expect in the coming weeks, including starting chemotherapy.
When Your Body Is Ready for Chemotherapy
Starting chemotherapy depends on how well the body has recovered. Doctors look at wound healing, overall health, and blood counts to decide. This approach makes sure patients are ready for chemotherapy.
Here’s a quick look at the typical recovery milestones and what they mean:
Recovery Period | Key Milestones | Healthcare Actions |
First Week | Initial healing, pain management | Rest, monitor for infection, pain medication |
Weeks 2-3 | Assessing healing progress, preparing for next treatments | Follow-up appointments, patient education |
Variable | Determining readiness for chemotherapy | Assess wound healing, overall health, blood counts |
The recovery process is a journey that needs patience and careful watching.
Factors That Determine Your Specific Timeline
The chemotherapy schedule after a lumpectomy is tailored based on several critical factors. Understanding these elements can help patients better prepare for their treatment journey.
Cancer Stage and Type Considerations
The stage and type of breast cancer are key in setting the chemotherapy timeline. Aggressive cancer types may require chemotherapy to start sooner, while early-stage cancers might allow for a slightly longer wait. We consider the cancer’s characteristics to plan the most effective treatment sequence.
For instance, if the cancer is hormone receptor-positive, the treatment plan might differ from that for triple-negative breast cancer. We assess these factors to decide the optimal timing for chemotherapy.
Surgical Healing Progress
The body’s healing progress after lumpectomy surgery is another critical factor. We need to ensure that the surgical site is healing properly before starting chemotherapy. This postoperative healing period typically lasts a few weeks and is essential for minimizing complications.
During this time, we monitor the patient’s recovery closely. If healing is slower than expected, we may need to adjust the chemotherapy start date.
Pathology Report Results and Their Impact
The pathology report provides vital information about the cancer and the effectiveness of the lumpectomy. We review these results carefully to determine if additional treatments, such as chemotherapy, are necessary.
The report’s findings can also influence the timing of chemotherapy. For example, if the margins are clear and the cancer is contained, we might have more flexibility in planning treatment. But if there’s a higher risk of recurrence, we may need to start chemotherapy sooner.
By considering these factors – cancer stage and type, surgical healing progress, and pathology report results – we can create a personalized treatment plan. This plan optimizes the timing of chemotherapy for the best possible outcome.
Clinical Guidelines for Chemotherapy Timing
The timing of chemotherapy after a lumpectomy is based on medical standards and research. These guidelines help ensure patients get the best treatment for their breast cancer.
Medical Standards for Post-Surgical Chemotherapy
Medical standards say chemotherapy should start 2-6 weeks after surgery. This allows enough time to recover from the lumpectomy. The exact timing depends on the surgery’s extent, any complications, and the patient’s health.
Adjuvant chemotherapy after lumpectomy is common for many breast cancer patients. It aims to kill any cancer cells left after surgery, lowering the chance of cancer coming back.
How Guidelines Have Evolved Over Time
Clinical guidelines for chemotherapy timing have changed a lot over time. They’ve been updated by new medical research and a deeper understanding of breast cancer. At first, the goal was to start chemotherapy right after surgery. But, as more evidence came in, guidelines started to consider the cancer type and stage, and the patient’s health.
Recent studies have made these guidelines even more precise. They show that starting chemotherapy too late can harm some patients. So, guidelines now stress starting chemotherapy on time but also making sure patients are fully recovered and ready for treatment.
There’s always new research on how to improve chemotherapy timing and administration. By following current guidelines and staying updated, doctors can give care that’s tailored to each patient’s needs.
How Your Oncologist Makes Timing Decisions
Oncologists decide when to start chemotherapy after careful thought. They look at medical tests and talk with a team. This helps make sure the treatment works well and you’re ready.
Medical Assessments Used to Determine Readiness
Your oncologist checks your health before starting chemotherapy. They look at your overall health, check for infections, and see how you’re doing after surgery. Your health status is key in deciding when to start chemotherapy.
These checks are important. They show if your body can handle the treatment. If you’re not fully recovered or have an infection, treatment might wait.
The Multidisciplinary Team Approach
Deciding when to start chemotherapy isn’t just one person’s job. Your oncologist works with surgeons, radiologists, and others. This team reviews your case and decides on the best timing for chemotherapy.
Team Member | Role in Decision Making |
Oncologist | Leads the chemotherapy treatment plan and timing decisions. |
Surgeon | Provides insights into the surgical outcome and recovery progress. |
Pathologist | Supplies information on the cancer type and stage from the pathology report. |
Personalized Treatment Planning
Every treatment plan is unique. Your oncologist looks at your cancer type, stage, health, and past treatments. This ensures the plan fits your needs perfectly.
By considering these factors, your oncologist creates a plan. It fights your cancer well and keeps side effects low. This plan also supports your overall health.
When Chemotherapy Might Be Delayed
Starting chemotherapy after a lumpectomy isn’t always easy. It can be delayed for many reasons. Usually, chemotherapy begins a few weeks after surgery. But, health problems or surgery issues can cause delays.
Surgical Complications That May Extend the Timeline
Surgical problems can make starting chemotherapy harder. Issues like hematoma, seroma, or wound infections can slow healing. This makes it unsafe to start chemotherapy too soon.
Surgical Complication | Impact on Chemotherapy |
Hematoma | May require additional surgery or drainage, delaying chemotherapy |
Seroma | Can cause swelling and discomfort, potentially delaying treatment |
Wound Infection | Requires antibiotic treatment and healing before chemotherapy can start |
Infection Concerns and Management
Infections after a lumpectomy are a big worry. They can change when chemotherapy starts. It’s key to manage infections well to get back on schedule.
“Effective infection management is critical to ensuring that chemotherapy can start as soon as possible.”
- Watch for signs of infection, like redness, swelling, or fever
- Take antibiotics as your doctor tells you to
- Keep your wound clean and follow your doctor’s advice
Other Health Issues That May Affect Timing
Other health problems can also affect when chemotherapy starts. It’s important to handle these issues well to avoid delays.
Knowing why delays happen and working with your healthcare team can help. This way, you can overcome challenges and keep up with your treatment plan.
Preparing for Chemotherapy During the Waiting Period
Getting ready for chemotherapy after a lumpectomy is more than just medical checks. It’s about preparing your body and mind for what’s coming. This preparation is key for a smoother treatment journey and can greatly affect your experience.
Physical Preparation Steps
Physical prep is a big part of getting ready for chemotherapy. Maintaining a healthy diet full of nutrients helps your body handle the treatment. Drinking lots of water is also important. Some people get help from a nutritionist to make a meal plan that fits their needs.
- Eat a balanced diet with lots of fruits, veggies, and lean proteins.
- Drink at least 8-10 glasses of water a day to stay hydrated.
- Avoid foods high in sugar, salt, and unhealthy fats.
Also, gentle exercise can boost your physical health and lower stress. Walking, yoga, or light swimming are good options. But, always talk to your doctor before starting any new exercise.
Emotional and Mental Readiness
Getting ready emotionally and mentally is just as important as physical prep. Mindfulness practices like meditation or deep breathing can help with anxiety and stress. Many find support groups helpful for sharing experiences and connecting with others facing similar challenges.
- Try mindfulness with meditation or deep breathing exercises.
- Join a support group to connect with others going through chemotherapy.
- Think about counseling or therapy for emotional support.
Practical Arrangements to Consider
Practical plans can make a big difference during chemotherapy. Organizing your schedule for treatment and recovery is key. You might need to arrange for transportation to treatment centers and have a support system for daily tasks and emotional support.
- Make a calendar for your treatment schedule and follow-up appointments.
- Find someone to drive you to and from chemotherapy sessions.
- Get your home ready by stocking up on essentials and making it comfortable for recovery.
By following these steps, you can prepare better for chemotherapy. This makes the journey less scary and more manageable.
Different Chemotherapy Regimens and Their Schedules
It’s important for patients to know about chemotherapy after a lumpectomy. Chemotherapy uses drugs to kill cancer cells. It’s often used after a lumpectomy to lower the chance of cancer coming back.
Common Chemotherapy Protocols After Lumpectomy
There are several chemotherapy protocols used after a lumpectomy. These include:
- AC-T (Adriamycin and Cytoxan followed by Taxotere): A mix of anthracyclines and taxanes, effective for many breast cancer patients.
- FEC-T (Fluorouracil, Epirubicin, and Cytoxan followed by Taxotere): A mix that includes an anthracycline and a taxane, popular in Europe.
- TC (Taxotere and Cytoxan): A regimen without anthracyclines, for those who can’t handle them well.
Duration and Frequency of Treatment Sessions
Chemotherapy sessions last different lengths and happen at different times. It’s usually given in cycles, lasting 2-4 weeks. The number of cycles can be 4 to 8, based on the regimen and how well the patient responds.
In the AC-T regimen, patients get 4 cycles of AC and then 4 cycles of T. This is done every 2-3 weeks. The whole treatment can take months, with close monitoring for side effects and how well the treatment is working.
Adjuvant vs. Neoadjuvant Approaches
Chemotherapy can be given before or after surgery. Adjuvant chemotherapy is after surgery to kill any remaining cancer cells and lower recurrence risk. Neoadjuvant chemotherapy is before surgery to shrink tumors, making them easier to remove and possibly reducing the need for extensive surgery.
The choice between adjuvant and neoadjuvant chemotherapy depends on several factors. These include the cancer’s stage and type, tumor size, and the patient’s health. Our healthcare team works with patients to choose the best option based on their needs.
The Role of Radiation Therapy in Your Treatment Timeline
Understanding radiation therapy’s role is key to your breast cancer treatment. After a lumpectomy, it helps kill any cancer cells left in the breast. This reduces the chance of cancer coming back.
Timing of Radiation Therapy in Relation to Chemotherapy
The timing of radiation therapy with chemotherapy varies. Usually, radiation comes after chemotherapy is done. But sometimes, it’s given at the same time as certain chemotherapy, called concurrent chemoradiation.
Sequential vs. Concurrent Therapy Approaches
Choosing between sequential or concurrent therapy depends on many factors. These include the cancer’s stage and type, your health, and treatment goals. Sequential therapy means one treatment after another. Concurrent therapy means using multiple treatments together.
Coordinating Multiple Treatment Modalities
Coordinating treatments needs a team effort. Your healthcare team will create a plan that includes radiation, chemotherapy, and other treatments. This plan is tailored just for you.
Treatment Modality | Typical Timing | Purpose |
Chemotherapy | Before or after surgery | Kill cancer cells throughout the body |
Radiation Therapy | After chemotherapy, if given | Eliminate remaining cancer cells in the breast |
Surgery (Lumpectomy) | Initial treatment step | Remove the tumor and some surrounding tissue |
Sequential vs. Concurrent Therapy Approaches
The choice between sequential and concurrent therapy depends on your case. Sequential therapy lets each treatment be fully given without mixing. This might lower side effects. Concurrent therapy targets the tumor with different treatments at the same time. It might be better for aggressive cancers.
Your oncologist will talk about the best option for you. They’ll consider the latest guidelines and what you prefer.
What to Expect at Your First Chemotherapy Appointment
Your first chemotherapy appointment is a big step in your treatment. Being ready can make it easier. Knowing what to expect can help reduce stress and make things smoother.
Pre-Treatment Testing and Evaluation
Before your first treatment, your team will do several tests. These tests check your health and if you’re ready for treatment. They might include:
- Blood tests to check your blood cell counts and liver function
- Imaging tests, such as X-rays or CT scans, to evaluate your current condition
- A review of your medical history and current medications
These tests help your oncologist make your treatment fit you best. They also help reduce side effects.
The First Day of Chemotherapy: A Step-by-Step Overview
On your first chemotherapy day, here’s what you can expect:
- Registration and preparation: Arrive early to complete any necessary paperwork and get settled.
- Initial assessment: Your nurse will check your vital signs and assess your overall condition.
- Port placement (if needed): If you don’t already have a port, you may have one placed on the day of or before your treatment.
- Chemotherapy administration: The chemotherapy drugs will be administered through your port or IV.
- Monitoring: Your healthcare team will closely monitor you for any reactions or side effects during and after the treatment.
Port Placement Considerations and Timing
If you need a port for chemotherapy, it’s usually placed before your first treatment. Your healthcare team will tell you when it’s best. A port makes getting chemotherapy drugs easier and more comfortable.
Getting ready for your first chemotherapy appointment is important. Knowing what happens, from tests to treatment, helps you feel more ready. It’s a big step in your treatment journey.
Managing Side Effects Throughout Your Treatment Journey
Handling side effects well is key to getting through chemotherapy. Knowing what side effects might happen and how to deal with them can make life better during treatment.
Common Side Effects and Their Timing
Side effects from chemotherapy can be different for everyone. Common ones include feeling tired, getting sick, losing hair, and changes in appetite. When these side effects show up can vary too.
For example, feeling very tired often lasts the whole treatment time. Losing hair usually starts a few weeks after starting chemo. Knowing when these side effects will happen can help you get ready and manage them better.
Strategies for Side Effect Management
There are ways to manage side effects from chemotherapy. For feeling sick, medicines like ondansetron can help. Eating well and drinking lots of water are also important. To fight tiredness, try to pace yourself and rest a lot.
Also, having support from loved ones or groups can help with the emotional side of chemo. Look into these options to find what works for you.
Side Effect | Management Strategy |
Fatigue | Pacing activities, rest |
Nausea | Anti-nausea medication, balanced diet |
Hair Loss | Emotional support, scalp cooling |
When to Contact Your Healthcare Team
It’s important to know when to talk to your healthcare team about side effects. If you have severe symptoms like a high fever, can’t stop feeling sick, or have signs of infection, call them right away.
Talking to your healthcare team often can help manage side effects better. They can also change your treatment plan if needed. Keeping a log of your side effects is a good idea to talk about during your visits.
Also, watch out for long-term effects like hypothyroidism from radiation therapy. Regular check-ups can help catch and manage these effects early.
Monitoring Treatment Effectiveness
After a lumpectomy, it’s important to keep an eye on how well treatment is working. This includes regular check-ups, tests, and changes to your treatment plan if needed. This ongoing effort helps see how your body is reacting to the therapy and makes sure you get the best care.
Follow-up Appointments and Testing
Seeing your healthcare team regularly is key to tracking your progress. They will check your health, look for cancer signs, and watch for treatment side effects. They might also do tests like imaging or blood work to see how you’re doing.
Common tests used to monitor treatment effectiveness include:
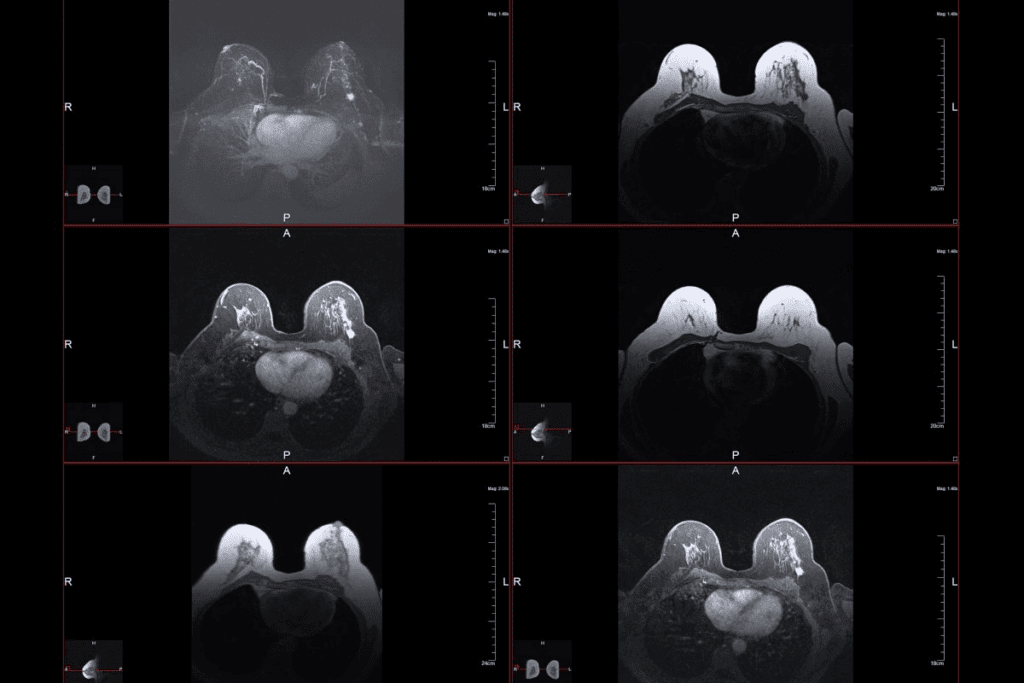
- Mammograms
- Ultrasound
- MRI scans
- Blood tests to check for tumor markers
Adjustments to Treatment Plans
As treatment goes on, your plan might need tweaks. This could mean changing the chemotherapy dose or type, adding radiation, or handling side effects. These changes help keep your treatment on track and improve your life quality.
Reason for Adjustment | Potential Change |
Inadequate response to current therapy | Switch to a different chemotherapy regimen |
Significant side effects | Modify dosage or add supportive medications |
New information from test results | Adjust treatment plan to address new findings |
Measuring Response to Therapy
Checking how well therapy is working means looking at how it controls cancer. Doctors use clinical checks, imaging, and tests to see how you’re doing. This helps them know if your treatment is effective and if it needs changes.
By watching how treatment is working and making changes when needed, your healthcare team aims for the best care. Working together with your healthcare providers is essential for good outcomes and quality of life during treatment.
Patient Experiences: Real-World Timelines
Breast cancer treatment is a journey that varies from person to person. Looking at real-world timelines and case studies helps us understand the different paths to recovery and treatment.
Case Studies of Different Recovery and Treatment Paths
Every breast cancer patient’s journey is unique. It depends on the cancer stage, overall health, and treatment type. For example, some patients start chemotherapy right after surgery. Others may wait longer due to complications or more treatments.
Lessons Learned from Breast Cancer Survivors
Breast cancer survivors share important lessons about treatment. They stress the need to prepare emotionally and mentally during the waiting period. As one survivor said,
“The waiting game is the hardest part. Staying positive and focused on your recovery is key.”
They also talk about making practical arrangements, like arranging for transportation and preparing meals. Learning from their experiences helps patients deal with treatment challenges.
Coping Strategies During the Waiting Period
The wait between lumpectomy and chemotherapy can be tough. Many find joy in hobbies or spending time with family. Mindfulness practices, like meditation or yoga, can also help manage stress and anxiety.
It’s vital to keep talking to your healthcare team during this time. Patients should ask questions and share any concerns. This way, they can feel more in control and confident as they wait.
Questions to Ask Your Healthcare Team About Your Treatment Timeline
Understanding your breast cancer treatment timeline is key. Knowing what to ask your healthcare team can help a lot. It makes you know what to expect.
Important Timeline Questions for Your Surgeon
Your surgeon is important at the start. It’s vital to ask about your recovery and how it affects your chemotherapy schedule.
- What is the expected recovery time after my lumpectomy?
- Are there any possible complications that could delay my chemotherapy?
- How will we know if I’m healing right?
Key Questions for Your Oncologist
Your oncologist will lead you through chemotherapy. The right questions can clear up your treatment plan and timeline.
- What chemotherapy regimen is best for my cancer type and stage?
- How many chemotherapy cycles will I need, and how often?
- Are there any side effects I should watch out for, and how can they be managed?
Coordinating Care Among Multiple Specialists
Breast cancer treatment involves many specialists. It’s important to coordinate their care for a smooth process.
- Who will be my main contact during treatment?
- How will my treatment plan be coordinated among my surgeon, oncologist, and other providers?
- What support services are available to help with my treatment and recovery?
By asking these questions, you can understand your treatment timeline better. This ensures you’re ready for what’s next.
Conclusion: Navigating Your Personal Treatment Journey
Going through treatment after a lumpectomy can be tough. It often includes chemotherapy and radiation therapy. Knowing the timeline for breast cancer treatment is key to getting ready for what’s next.
Chemotherapy usually starts 2-6 weeks after surgery. This depends on your health, how advanced the cancer is, and how well you’re healing.
Getting good guidance means knowing your treatment choices, asking important questions, and talking openly with your doctors. Your oncologist will check if you’re ready for chemo. They look at how you’re doing after surgery and the cancer test results.
Being active and involved in your care helps you face the challenges of treatment. Remember, everyone’s journey is different. Getting care that fits you is important for the best results.
FAQ
How long after a lumpectomy does chemotherapy typically start?
Chemotherapy usually starts 2–6 weeks after a lumpectomy. This allows time for healing and to assess the cancer.
What factors influence the timing of chemotherapy after a lumpectomy?
The timing depends on the cancer’s stage and type, how well you’re healing, and the pathology report.
Why is there a waiting period before starting chemotherapy?
The waiting period helps with recovery, understanding the cancer, and planning the best treatment.
Can chemotherapy be delayed after a lumpectomy?
Yes, chemotherapy can be delayed if there are surgical complications, infections, or health issues.
How do oncologists determine the timing of chemotherapy?
Oncologists use medical assessments and consider the team’s input to plan the best timing for chemotherapy.
What are the different chemotherapy regimens used after a lumpectomy?
There are adjuvant and neoadjuvant chemotherapy protocols. Each has its own schedule and duration based on the case.
How is radiation therapy coordinated with chemotherapy?
Radiation therapy can be given before, during, or after chemotherapy. It depends on the treatment plan and the patient’s needs.
What can I expect at my first chemotherapy appointment?
At the first appointment, you’ll have pre-treatment testing and a detailed overview of the treatment process.
How are side effects managed during chemotherapy?
Side effects are managed with medication, lifestyle changes, and talking to your healthcare team.
How is treatment effectiveness monitored?
Effectiveness is monitored through follow-up appointments, testing, and adjusting the treatment plan as needed.
What questions should I ask my healthcare team about my treatment timeline?
Ask about the treatment sequence, managing side effects, and how specialists work together for your care.
How long does chemotherapy last after a lumpectomy?
Chemotherapy’s length varies by regimen and individual factors. It usually lasts from a few months to several months.
Can I prepare for chemotherapy during the waiting period?
Yes, you can prepare physically, emotionally, and practically for chemotherapy during the waiting period. Follow your healthcare team’s advice.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6123282/





