Last Updated on November 20, 2025 by Ugurkan Demir

At Liv Hospital, we know that adenocarcinoma treatment is complex and tailored to each patient. Chemotherapy is a key part of this treatment, often paired with surgery or radiation therapy.Learn about chemotherapy for adenocarcinoma, including the most effective drugs, regimens, and side effects.
Chemotherapy uses medicines to kill cancer cells. It’s a vital treatment for those seeking effective care. We’ll look at seven important drugs for treating adenocarcinoma, a cancer that starts in glandular cells.
It’s important for patients to understand these chemotherapy options. Our team is here to offer support and guidance every step of the way.

Adenocarcinoma is a complex cancer type. It needs a detailed treatment plan based on its location and stage. We will look into the specifics of adenocarcinoma and the different treatment options available.
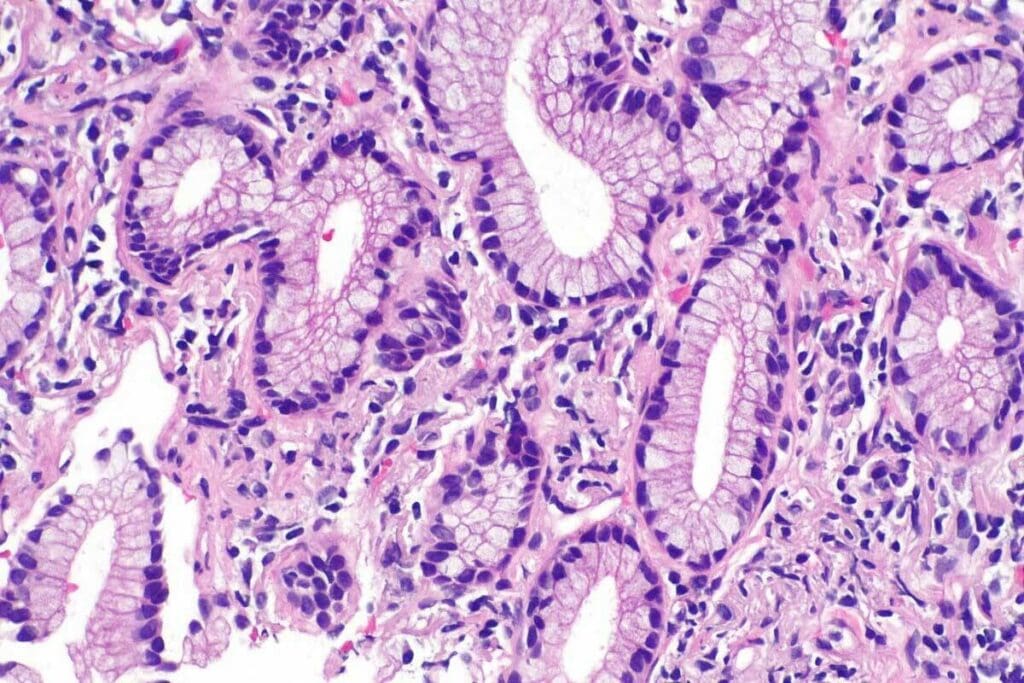
Adenocarcinoma starts in gland cells. It can happen in places like the breast, colon, lung, and prostate. Studies show it’s the most common cancer in some groups. Where it occurs affects how it’s treated.
Because it starts in gland cells, adenocarcinoma can show up differently. For example, lung adenocarcinoma is not the same as breast adenocarcinoma. This means each type needs its own treatment plan.
Treatment for adenocarcinoma depends on several factors. These include where the cancer is, its stage, and the patient’s health. Important chemotherapy drugs include cisplatin, oxaliplatin, paclitaxel, gemcitabine, fluorouracil (5-FU), pemetrexed, and irinotecan. These drugs are often mixed and used in different orders to work best.
Choosing the right treatment is very personal. It’s based on each patient’s unique situation. Experts say,
“The treatment of adenocarcinoma must be tailored to the specific type and stage of the cancer.”
| Cancer Location | Common Chemotherapy Drugs | Treatment Approach |
| Colon | Fluorouracil (5-FU), Oxaliplatin | Combination chemotherapy |
| Lung | Gemcitabine, Cisplatin | Platinum-based chemotherapy |
| Breast | Paclitaxel | Taxane-based chemotherapy |
Understanding adenocarcinoma and its treatment helps doctors create better plans. This improves how well patients do.
Chemotherapy is key in treating adenocarcinoma. It targets fast-growing cancer cells. This treatment stops these cells from growing and spreading.
Chemotherapy drugs mess with DNA replication. This stops cancer cells from growing and dividing. Different types of chemotherapy agents target different stages of the cell cycle.
For example, cisplatin damages DNA to stop cell division. Paclitaxel, a taxane, disrupts microtubules to stop cell division. This multi-faceted approach helps manage adenocarcinoma well.
Chemotherapy is often used for adenocarcinoma at advanced stages or with metastasis. The choice to use chemotherapy depends on the cancer’s stage, the patient’s health, and genetic markers.
| Cancer Stage | Common Chemotherapy Regimens | Treatment Goals |
| Early-stage | Adjuvant chemotherapy (e.g., cisplatin, 5-FU) | Reduce recurrence risk |
| Advanced-stage | Palliative chemotherapy (e.g., gemcitabine, paclitaxel) | Improve quality of life, extend survival |
| Metastatic | Combination chemotherapy (e.g., FOLFOX, CAPOX) | Control tumor growth, manage symptoms |
Advances in drug delivery and immunotherapy are improving adenocarcinoma treatment. Tailoring chemotherapy to each patient boosts survival and quality of life.
Cisplatin is a key drug in treating adenocarcinomas. It works by linking DNA in cancer cells, stopping them from growing. This drug is a cornerstone in cancer treatment.
Cisplatin forms platinum-DNA adducts, which block DNA repair. This leads to cell death. It’s very effective against lung, ovarian, and testicular cancers.
Cisplatin’s success in treating cancer is well-known. It’s often paired with other drugs to boost its power. Its ability to target fast-growing cancer cells makes it essential in many treatments.
Cisplatin is given through an IV, alone or with other drugs. The dose and schedule depend on the cancer type and the patient’s health.
To lessen side effects, hydration, and diuretic protocols are used. These help avoid kidney damage, a common side effect.
Cisplatin can cause nausea, vomiting, and kidney problems. It’s important to manage these side effects to improve the patient’s life during treatment.
To handle side effects, antiemetic meds control nausea and vomiting. Monitoring kidney function is also key to avoiding kidney damage. By managing these issues, we help patients better tolerate cisplatin.
Oxaliplatin is a key drug in treating gastrointestinal adenocarcinoma. It’s a platinum-based chemotherapy that helps with various cancers, like colorectal and gastric adenocarcinomas.
Oxaliplatin is different from cisplatin in its structure and how it works. It has a diaminocyclohexane (DACH) carrier ligand that makes it unique. This uniqueness helps it work in cases where cisplatin might not.
Studies show oxaliplatin can overcome some resistance to cisplatin. This makes it a good choice in treatment plans.
Specific Applications in Colorectal and Gastric Adenocarcinomas
Oxaliplatin works well for colorectal and gastric adenocarcinomas. In colorectal cancer, it’s often paired with 5-FU and leucovorin in the FOLFOX regimen. This combo boosts survival and cuts down on cancer coming back.
In gastric adenocarcinoma, oxaliplatin is a better choice than cisplatin for some patients. It’s used with other drugs to improve treatment results for this tough cancer.
Oxaliplatin has some common side effects but also unique ones. A big concern is neurotoxicity, leading to peripheral neuropathy. This can be sudden or long-term and worsens in cold weather.
We use different approaches to handle these side effects, like adjusting doses and providing support. We also teach patients to avoid colds and manage symptoms. This way, we can make the most of oxaliplatin in treating gastrointestinal adenocarcinomas.
Paclitaxel is a key chemotherapy drug in the battle against adenocarcinoma. It’s used in combination regimens to boost its fight against cancer cells.
Paclitaxel stops cancer cells from dividing by stabilizing microtubules. This is key in slowing adenocarcinoma growth.
Effectiveness: Research shows Paclitaxel works well against various adenocarcinomas. This includes cancers of the breast, lung, and ovaries.
Paclitaxel is often paired with other drugs to improve its impact. Common combinations include:
The exact dosage and schedule depend on the cancer type and the patient’s health.
Paclitaxel is effective but can cause side effects. These include:
| Side Effect | Management Strategy |
| Hair Loss | Counseling and scalp cooling techniques |
| Neutropenia | Monitoring blood counts, use of G-CSF |
| Neuropathy | Dose adjustment, symptom management |
Patients need to talk to their healthcare provider about possible side effects. This helps understand the benefits and risks of Paclitaxel treatment.
“Understanding the side effects of Paclitaxel and how to manage them is key to improving patients’ quality of life during chemotherapy.”
— Expert Oncologist
Gemcitabine is a key part of chemotherapy for pancreatic and lung adenocarcinomas. It stops cancer cells from growing by blocking DNA synthesis.
Gemcitabine gets into DNA and kills cells by stopping DNA synthesis. This is key in fighting pancreatic and lung adenocarcinomas.
Gemcitabine is very effective against pancreatic adenocarcinoma, improving survival rates. It’s also used for lung adenocarcinoma, often with other drugs.
Gemcitabine’s flexibility makes it a great choice for many adenocarcinoma treatments.
Gemcitabine is usually safe but can cause fatigue, nausea, and blood problems. It’s important to manage these side effects to keep patients’ quality of life good.
Doctors adjust doses and use supportive care to help. Keeping a close eye on patients helps catch side effects early.
The chemotherapy drug Fluorouracil (5-FU) is key in fighting gastrointestinal adenocarcinoma. It has been a mainstay in cancer treatment for decades. This shows its lasting value in fighting cancer.
Fluorouracil (5-FU) stops cancer cells from making DNA by blocking thymidylate synthase. This makes it effective against gastrointestinal adenocarcinomas. First used in the 1950s, 5-FU’s use has grown, thanks to better ways of giving it and combining it with other drugs.
5-FU was a big step forward in cancer treatment. It was one of the first drugs to really fight solid tumors, like colorectal cancer. Its introduction changed how we treat cancer today.
Today, 5-FU is given in ways that make it work better and cause fewer side effects. For example, giving it slowly over time keeps drug levels steady. This helps fight cancer more and hurts less. Also, mixing 5-FU with other drugs, like in FOLFOX, is now common for treating advanced colorectal cancer.
5-FU can cause side effects like stomach problems, low blood counts, and hand-foot syndrome. It’s important to manage these to keep patients’ quality of life good. Doctors adjust doses, use supportive care, and add drugs like leucovorin to lessen side effects.
Knowing how 5-FU works, its history, and how it’s given today helps doctors use it better. This improves how well patients do with gastrointestinal adenocarcinoma.
Pemetrexed and irinotecan are two drugs that show great promise in treating certain types of adenocarcinoma. They target specific ways cancer cells grow. This offers new ways to fight cancer.
Pemetrexed is a chemotherapy drug that targets folate-dependent processes. It’s very effective against lung adenocarcinoma. It stops cancer cells from making DNA, which slows down tumor growth.
Clinical Application: Pemetrexed is mainly used for non-small cell lung cancer (NSCLC). It’s best for patients with non-squamous histology. It’s often given with other drugs or as part of a maintenance plan.
Irinotecan works by stopping topoisomerase I, an enzyme that cancer cells need to copy their DNA. This stops cancer cells from dividing and leads to cell death.
Treatment Use: Irinotecan is often used for colorectal cancer and sometimes for gastric cancer. It’s usually given with other drugs to make it more effective.
Choosing between pemetrexed and irinotecan depends on several things. These include the type of adenocarcinoma, the patient’s health, and past treatments. Both drugs are effective, but the choice depends on the patient’s specific needs and cancer type.
Understanding tumor genetics has led to personalized chemotherapy. This is a big change in treating adenocarcinoma. Now, we can make treatment plans that fit each patient’s tumor genetics.
Choosing chemotherapy based on tumor genetics is becoming common. We look at the genetic mutations in a patient’s tumor to find the best chemotherapy. This method makes treatments more effective and lowers side effects.
Key benefits of personalized chemotherapy include:
Chemo-immunotherapy combinations are showing promise in improving survival rates. By mixing traditional chemotherapy with immunotherapy, we boost the body’s cancer-fighting abilities. This mix has worked well for some adenocarcinoma types.
The synergy between chemotherapy and immunotherapy leads to a stronger attack on cancer cells. Chemotherapy can shrink tumors, making it easier for immunotherapy to target and kill cancer cells.
Protocols are being developed for different adenocarcinoma types, like gastric and duodenal. These protocols consider the unique traits of each cancer type and location. This allows for more targeted and effective treatments.
For instance, gastric adenocarcinoma needs a different treatment than duodenal adenocarcinoma. Knowing these differences helps us create better treatment plans.
One big challenge in treating adenocarcinoma is drug resistance. Researchers are exploring new ways to overcome this, like combination therapies and novel delivery methods.
Improving delivery methods is also key. Methods like nanoparticle delivery and targeted therapy are being looked into. They aim to make chemotherapy more effective while reducing side effects.
By advancing our knowledge of adenocarcinoma and developing new treatments, we can improve patient outcomes and quality of life.
Chemotherapy for adenocarcinoma has seen big improvements. This has led to better survival rates and quality of life for patients. New chemotherapy agents and treatment plans have grown our fight against this tough disease.
Liv Hospital is at the forefront of these advancements. We aim for top-notch care by following the latest academic protocols and teaming up with experts from different fields. Our goal is to provide personalized and effective treatments for adenocarcinoma.
Chemotherapy is a key part of treating adenocarcinoma. With ongoing research, we expect even better treatment options in the future. As we keep pushing forward, we hope to bring more hope to those fighting adenocarcinoma.
Adenocarcinoma starts in glandular cells. These cells are found in places like the breast, colon, and lung. It’s different from other cancers because it comes from glandular tissue.
To fight adenocarcinoma, doctors use drugs like cisplatin, oxaliplatin, and paclitaxel. They also use gemcitabine, fluorouracil (5-FU), pemetrexed, and irinotecan. These drugs are often mixed with surgery and radiation therapy.
Chemotherapy stops cancer cells from growing and dividing. This is key when the cancer has spread or grown a lot.
Cisplatin harms the DNA of cancer cells, stopping them from making copies. It’s a main drug for many adenocarcinomas.
Oxaliplatin is used for stomach and colon cancers. It works differently from cisplatin and has different side effects.
Paclitaxel stops adenocarcinoma cells from dividing. It’s used in many treatments for adenocarcinoma.
Gemcitabine stops DNA synthesis in cancer cells. It’s very effective against pancreatic and lung cancers.
Fluorouracil (5-FU) blocks an enzyme needed for DNA in cancer cells. It’s mainly used for stomach and colon cancers.
Pemetrexed targets lung adenocarcinoma. Irinotecan works on stomach and colon cancers. Both are special drugs for specific adenocarcinomas.
New treatments include personalized drugs based on tumor genetics and combining chemotherapy with immunotherapy. These advances are making treatments more effective and reducing side effects.
Chemotherapy is key for duodenum cancer, often with surgery and radiation. The treatment plan depends on the cancer’s stage and type.
Chemotherapy is a major treatment for adenocarcinoma; whether it can cure it depends on the cancer’s stage, location, and genetics. In some cases, it can greatly reduce tumor size or even lead to remission.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!