Last Updated on October 31, 2025 by

Diagnosing congestive heart failure (CHF) needs a detailed approach. This includes looking at the patient’s history, physical check-ups, and different tests. At Liv Hospital, we stick to international standards and focus on the patient to make sure we check every important test.
Getting the diagnosis right and treating it well is key. It helps avoid more hospital stays, lowers sickness and death rates, and makes patients feel better. We use many important tests to get a full view of a patient’s health.
A detailed diagnostic workup helps doctors create specific treatment plans. This makes patients’ lives better and improves their health.
Heart failure means the heart can’t pump enough blood for the body’s needs. This calls for detailed tests to understand and manage it. It’s caused by problems with the heart’s ability to pump blood, making tests key to treatment.
Congestive heart failure (CHF) is a complex issue. It happens when the heart can’t pump enough blood. This leads to changes in the heart and body, making it hard to manage.
The main causes of CHF are:
These factors make CHF worse, showing why detailed tests are needed to check the heart’s function and plan treatment.
Diagnosing heart failure early and correctly is key to better patient care. Tests help doctors see how much the heart is strained and if other organs are affected. This info is vital for creating a treatment plan that fits the patient’s needs.
The benefits of early diagnosis are:
| Benefit | Description |
| Improved Patient Outcomes | Early action can slow disease and improve life quality. |
| Targeted Treatment | Right diagnosis means treatments can be more effective. |
| Reduced Healthcare Costs | Early care can cut down on expensive treatments and hospital stays. |
A leading cardiologist says, “Early diagnosis and treatment of heart failure can greatly improve patient outcomes, lowering sickness and death rates.”
“Finding heart failure early lets us start the right treatment, which can change the disease’s course.”
Medical Expert, Cardiologist
Tests like B-type natriuretic peptide (BNP) and NT-proBNP are key in diagnosing and managing heart failure. They help measure how much the heart is strained and how severe the condition is. This guides treatment and improves care.
B-type natriuretic peptide (BNP) is key in diagnosing congestive heart failure (CHF). It’s a hormone made by the heart’s ventricles when they’re stretched too much. We’ll look at how BNP helps diagnose CHF, its levels, and its limits.
BNP levels show how severe heart failure is. When the heart is strained, it releases BNP into the blood. High BNP levels mean the heart is working too hard, often because of CHF. Doctors use BNP to understand the heart’s condition and how much strain it’s under.
Understanding BNP levels is important. A BNP under 100 pg/mL is normal, and over 400 pg/mL suggests heart failure. Values in between need careful thought, considering the patient’s symptoms and other tests. BNP is very useful in urgent situations where quick diagnosis is needed.
BNP has its downsides. Age, obesity, and kidney problems can change BNP levels. Doctors must think about these when looking at BNP results. Also, some medicines can affect BNP levels, which is important when treating CHF.
Knowing BNP’s role and its limits helps us use it better in treating CHF. This leads to better care for patients.
NT-proBNP is another important marker for heart failure, giving insights beyond BNP. Both BNP and NT-proBNP are key in diagnosing and managing congestive heart failure (CHF). NT-proBNP is getting more attention for its role in diagnosing and predicting outcomes.
BNP and NT-proBNP are heart peptides released under strain. They differ in how they are made and cleared. NT-proBNP is the N-terminal part of BNP’s pro-hormone. It’s more stable in blood, making it a reliable marker.
NT-proBNP is important for diagnosing heart failure and predicting outcomes. It shows how severe heart failure is. Cut-off values for NT-proBNP help diagnose heart failure; levels over 300 pg/mL suggest it. But, these values can change with age and other factors.
NT-proBNP helps not just in diagnosing but also in predicting patient outcomes. High levels mean a higher risk of bad outcomes. Monitoring NT-proBNP levels helps see if treatments are working and predicts patient outcomes. This makes NT-proBNP a key tool in managing CHF.
In summary, NT-proBNP is a valuable marker for heart failure diagnosis and management. Its stability, clinical significance, and predictive value make it essential in CHF care.
Cardiac troponins are key in finding heart muscle damage. They are proteins that get into the blood when the heart muscle is hurt. This makes them important for diagnosing heart failure.
Troponin I and Troponin T are parts of the troponin complex. They help control the heart muscle’s contraction. They are very specific to heart muscle damage. Troponin I and Troponin T get into the blood after the heart is injured. This makes them great for spotting acute myocardial infarction and checking for heart damage in heart failure.
In acute heart failure, high troponin levels mean the heart is injured. But, in chronic heart failure, troponin levels can stay high or change. This shows the heart is stressed or damaged over time.
In chronic heart failure, troponin levels show how bad the disease is. If troponin stays high, it might mean the disease is getting worse.
The level of troponin shows how bad the heart injury is. This means how bad the heart failure is. Studies show that higher troponin levels mean more sickness and death in heart failure patients.
Knowing how cardiac troponins help find heart muscle damage helps us take better care of heart failure patients. This could lead to better results for them.
The electrolyte panel is key in CHF monitoring. It helps spot issues that can affect patient health. Electrolytes like sodium, potassium, magnesium, and calcium are important for heart rhythm and function.
Sodium levels help keep the body’s fluid balance right. Low sodium, or hyponatremia, is common in CHF patients. It’s linked to too much fluid and how severe the heart failure is.
We watch sodium levels closely. Problems can cause confusion, seizures, and even coma in bad cases.
Potassium is key for heart health. CHF meds, like diuretics, can change potassium levels. This can lead to too little or too much potassium.
We manage potassium levels carefully. Imbalances can cause serious heart rhythm problems.
Magnesium and calcium are vital but often missed. They’re important for heart function. Low magnesium can cause heart rhythm issues and muscle weakness.
Calcium is essential for heart muscle contraction. Its imbalance can cause heart problems.
To show why electrolyte monitoring is important, here’s a table. It lists key electrolytes and their roles in CHF:
| Electrolyte | Abnormality | Potential Complications |
| Sodium | Hyponatremia | Confusion, seizures, coma |
| Potassium | Hypokalemia/Hyperkalemia | Arrhythmias, cardiac arrest |
| Magnesium | Hypomagnesemia | Arrhythmias, muscle weakness |
| Calcium | Hypocalcemia/Hypercalcemia | Cardiac contraction abnormalities |
By keeping an eye on these electrolytes and fixing any issues, we can better manage CHF. This improves patient care and outcomes.
Checking how well the kidneys work is key for CHF patients. Kidney problems often go hand in hand with heart issues. We’ll look at the important tests for kidney function and why they matter in treating CHF.
Blood Urea Nitrogen (BUN) and creatinine tests are basic for kidney health checks. BUN shows how much urea is in the blood, and creatinine is a waste from muscles. High levels of either can mean the kidneys are not working right. For CHF patients, these tests help figure out how bad kidney problems are and help decide treatment.
Table: Interpretation of BUN and Creatinine Levels
| Parameter | Normal Range | Impaired Range |
| BUN | 7-20 mg/dL | >20 mg/dL |
| Creatinine | 0.6-1.2 mg/dL (male) | >1.2 mg/dL (male) |
| Creatinine | 0.5-1.1 mg/dL (female) | >1.1 mg/dL (female) |
The estimated Glomerular Filtration Rate (eGFR) is a key measure from creatinine levels, age, gender, and race. It gives a better look at kidney function than creatinine alone. For CHF patients, a low eGFR means serious kidney trouble, making heart failure harder to manage. We use eGFR to adjust medication and watch kidney disease progress.
Cardiorenal syndrome (CRS) is when heart and kidney problems affect each other. In CHF, CRS is very important because it can make things worse. By checking BUN, creatinine, and eGFR, we can spot CRS. Managing CRS needs a team effort, including better heart care, fluid management, and watching kidney function closely.
Understanding renal function tests helps us care for CHF patients better. Regular checks and adjusting treatment plans are key to meeting their complex needs.
Liver function tests are key in checking for liver issues in heart failure patients. When the heart can’t pump well, blood backs up into the liver. This can harm the liver, which tests can show.
Tests look at AST, ALT, and bilirubin levels. In heart failure, these might be higher because of liver congestion. But big jumps in these numbers usually mean serious liver damage, not just congestion. Bilirubin levels, mainly total bilirubin, also show how bad the heart failure and congestion are.
When looking at liver tests in heart failure, it’s important to think about the whole picture. Small increases in liver enzymes don’t always mean big problems. But big changes or ongoing issues need more checking. It’s key to tell if liver issues come from heart problems or other diseases.
Bad liver test results in heart failure patients mean they might face more health problems and even death. These signs can show how serious the heart failure is and if there are other health issues. So, keeping an eye on liver health is very important for treating heart failure well.
In short, liver function tests are very helpful in managing heart failure. By understanding what liver test results mean, doctors can better help patients. This helps in finding the best ways to treat heart failure.
Managing congestive heart failure involves more than just checking for anemia. A complete blood count (CBC) gives a deeper look into a patient’s health. Anemia is common in heart failure patients, affecting their health and life quality. But, the CBC offers key information for better treatment and outcomes.
Hemoglobin and hematocrit values in the CBC are key. They show how well blood carries oxygen. In heart failure, anemia can reduce oxygen to tissues, making symptoms worse. Low hemoglobin levels are linked to higher risks of illness and death in heart failure patients. So, keeping an eye on these values is vital for managing anemia and improving heart failure treatment.
The white blood cell count (WBC) is another important CBC parameter. It shows how well the body fights off infections. Heart failure patients face a higher risk of infections due to weaker heart function and medication side effects. A high WBC count may signal an infection that needs treatment to avoid serious problems.
The platelet count is also critical in the CBC. Low platelet counts can be caused by heart failure medications like heparin. High platelet counts might suggest inflammation or other issues affecting heart failure care. Knowing these values helps doctors manage the risk of blood clots and decide on blood thinners.
In summary, the CBC is more than just a test for anemia. It helps doctors understand hemoglobin, hematocrit, white blood cell, and platelet counts. This information lets them create a more detailed treatment plan for each patient.
Urinalysis is often overlooked but it’s very useful in heart failure care. It gives important clues about kidney health, fluid balance, and how well medicines work. This makes it key for managing heart failure well.
Proteinuria, or too much protein in the urine, is a big warning sign in heart failure. Research shows it links to more sickness and death in these patients. Spotting proteinuria through urinalysis helps find patients at high risk, so they can get better care.
Proteinuria might mean kidney damage or problems, which is common in heart failure. It happens because the kidneys don’t get enough blood. Finding proteinuria helps doctors understand the patient’s risk better and plan treatments.
Urinalysis is key for checking fluid levels and kidney health in heart failure patients. It looks at urine concentration, specific gravity, and casts. Changes in these can show heart failure getting worse or kidney injury, leading to quick action.
Doing regular urinalysis helps see if treatments for fluid buildup are working. It also spots early signs of kidney problems, like injury from too much diuresis.
Some heart failure medicines can change how urine works. Diuretics, for example, can change urine output and electrolytes. ACE inhibitors and ARBs can affect potassium levels. Urinalysis checks these changes, making sure medicines work well and safely.
By watching urine closely, doctors can adjust or change medicines as needed. This helps avoid bad side effects and improves heart failure care.
Thyroid function tests are key in managing heart failure. They help find out how thyroid issues affect the heart. It’s important to check the thyroid in heart failure patients.
Thyroid-stimulating hormone (TSH) and free thyroxine (Free T4) are vital in thyroid tests. TSH shows if the thyroid is working right, and Free T4 shows the hormone levels. Together, they help find and treat thyroid problems that can harm the heart.
We look at TSH and Free T4 to spot thyroid issues. Overt problems have abnormal TSH and Free T4 levels. Subclinical problems have only abnormal TSH levels.
Thyroid problems and heart failure are closely linked. Both too much and too little thyroid hormone can hurt the heart. Too much can make the heart work too hard, while too little can make it work less efficiently.
Bad thyroid test results mean big changes in heart failure care. Finding and treating thyroid issues can help the heart. For example, treating too much thyroid can stop heart failure from getting worse. Giving thyroid hormone to those with too little can make the heart work better.
The table below shows how bad thyroid test results affect heart failure care:
| Thyroid Status | TSH Level | Free T4 Level | Management Implication |
| Euthyroid | Normal | Normal | Continue monitoring thyroid function |
| Hyperthyroidism | Low | High | Treat with antithyroid medications or radioactive iodine |
| Hypothyroidism | High | Low | Initiate thyroid hormone replacement therapy |
| Subclinical Hyperthyroidism | Low | Normal | Monitor closely; consider treatment if TSH is very low |
| Subclinical Hypothyroidism | High | Normal | Monitor; consider thyroid hormone replacement if TSH is very high or symptoms are present |
Knowing the thyroid status helps us make better care plans for heart failure patients.
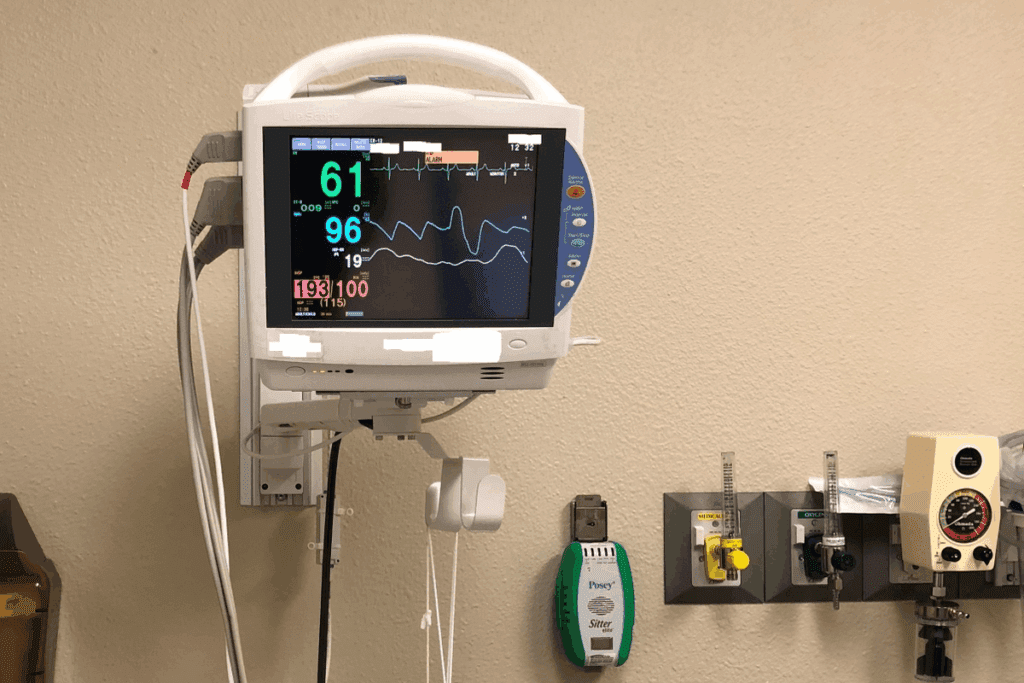
Electrocardiogram (ECG) findings are key in diagnosing heart failure. They show different heart problems. An ECG records the heart’s electrical signals. This gives important info about its rhythm, rate, and electrical activity.
Patients with heart failure often have arrhythmias and conduction problems. These include atrial fibrillation, ventricular tachycardia, and heart block. Identifying these is vital for managing their care and predicting their future.
Atrial fibrillation is common in heart failure patients. It raises the risk of blood clots. ECG monitoring helps spot these issues and guide treatment.
Atrial fibrillation causes an irregular heartbeat, leading to symptoms like palpitations and shortness of breath. Other rhythm problems, like ventricular tachycardia, can also be seen on an ECG. This shows why constant monitoring is key for high-risk patients.
| Arrhythmia Type | ECG Characteristics | Clinical Significance |
| Atrial Fibrillation | Irregularly irregular rhythm, absence of P waves | Increased risk of thromboembolic events |
| Ventricular Tachycardia | Wide QRS complexes, AV dissociation | Life-threatening, requires immediate intervention |
Left ventricular hypertrophy (LVH) makes the heart’s left ventricle muscle thicker. ECG signs of LVH include increased QRS complex voltage and repolarization issues. LVH is a big risk factor for heart problems, so finding it on an ECG is very important.
A study in the Journal of the American College of Cardiology found that ECG signs of LVH increase heart event risk.
“The presence of LVH on an ECG should prompt further evaluation and management to reduce cardiovascular risk.”
Journal of the American College of Cardiology
Ischemic changes on an ECG, like ST-segment depression or T-wave inversion, show heart muscle problems. These signs are key in diagnosing heart disease, a common heart failure cause. Quickly spotting these changes helps in timely treatments, improving patient results.
Understanding ECG findings helps doctors make better care decisions. This includes adjusting medications and deciding on more tests or treatments.
Imaging studies are key in diagnosing and managing heart failure. They give detailed views of the heart’s structure and function. This helps doctors assess the heart, spot issues, and plan treatments.
A chest X-ray is a basic tool for heart failure diagnosis. It shows signs of Kerley B lines and alveolar edema in the lungs and an enlarged heart. These signs help doctors understand how severe the heart failure is and what treatment is needed.
Echocardiography is the top choice for checking the heart in heart failure patients. It gives detailed info on left ventricular ejection fraction (LVEF), valve health, and wall motion. This test is non-invasive and key for diagnosing and tracking heart failure, helping adjust treatments as needed.
For complex cases or when more detail is needed, cardiac MRI and cardiac CT scans are used. These give high-resolution images of the heart’s structure and function. They help diagnose complex heart conditions and plan surgeries.
The need for imaging studies in CHF management changes based on the patient’s condition and treatment response. Echocardiography is done at diagnosis and as needed to track changes. Advanced imaging is used for specific reasons, like checking for advanced treatments or assessing heart viability before surgery.
Managing congestive heart failure (CHF) well depends on using test results from different labs and tests. We talked about 12 key labs and tests for CHF, like B-type Natriuretic Peptide (BNP) and cardiac troponins. These include electrolyte panels and imaging studies too.
Healthcare providers can understand a patient’s condition fully by combining these test results. This helps in making accurate diagnoses and effective treatments. It’s important to avoid hospital visits, reduce sickness and death, and improve patient care in CHF management.
CHF management needs a team effort. It involves using lab values like BNP and NT-proBNP levels to make treatment choices. This way, we can better manage heart failure and give top-notch care to patients.
The main aim of congestive heart failure labs is to help make treatment plans that improve patient outcomes. By using test results and insights from congestive heart failure labs, we can make CHF management better. This improves the quality of life for patients with heart failure.
BNP is a key biomarker that shows how much stress the heart is under. It helps doctors diagnose and manage congestive heart failure.
NT-proBNP and BNP are both used to diagnose heart failure. But NT-proBNP has different levels and meanings, affecting how doctors predict outcomes.
Cardiac troponins, like troponin I and troponin T, are important for spotting heart damage in patients with heart failure. They show how severe the disease is and how it might progress.
An electrolyte panel is key for spotting imbalances like sodium and potassium issues. It also checks magnesium and calcium levels, which are often overlooked but very important for patient health.
Renal function tests, like BUN, creatinine, and eGFR, check how well the kidneys are working. They help doctors understand if there’s a link between heart and kidney problems.
Liver function tests, such as AST, ALT, and bilirubin, help see if the liver is affected by heart failure. They give clues about liver health and how it might affect the patient’s future.
A CBC does more than just check for anemia. It looks at hemoglobin, hematocrit, white blood cells, and platelets. This info is vital for patient care and treatment.
Urinalysis is important for checking protein levels, fluid balance, and kidney function. It also shows how certain medications affect the urine. This info is important for patient care and treatment planning.
Testing thyroid function, including TSH and free T4, helps find other health issues that might be affecting the heart. It’s important for managing both thyroid problems and heart failure.
ECG findings, like arrhythmias and left ventricular hypertrophy, are key for diagnosing heart failure. They help doctors understand the heart’s condition and plan treatment.
Imaging studies, like chest X-rays and echocardiography, show the heart’s structure and function. They help doctors diagnose and manage CHF.
Labs used for diagnosing and monitoring CHF include BNP, NT-proBNP, cardiac troponins, and more. These tests help doctors understand the heart’s condition and plan treatment.
National Center for Biotechnology Information. (2025). 12 Essential Labs and Tests for a Complete. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430873/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!