Last Updated on November 13, 2025 by
Thanks to decades of medical progress, most childhood cancer survivors now live to adulthood and beyond. We have seen significant improvements in pediatric cancer survival rates. Recent childhood cancer survival statistics show that the five-year survival rate for childhood cancers now averages 85%, reflecting substantial advances in diagnosis and treatment.

We are making strides in understanding the long-term implications of childhood cancer and its treatment. This enables us to provide better care for survivors. As we continue to advance in diagnosis, treatment, and follow-up care, the outlook for these individuals is becoming more promising.
Key Takeaways
- Advances in medical care have significantly improved childhood cancer survival statistics.
- The average five-year survival rate for childhood cancers is now 85%.
- Ongoing challenges for survivors include long-term health risks.
- Better follow-up care is key to improving the quality of life for survivors.
- Continued research is needed to understand and mitigate the long-term effects of cancer treatment.
The Landscape of Childhood Cancer Today
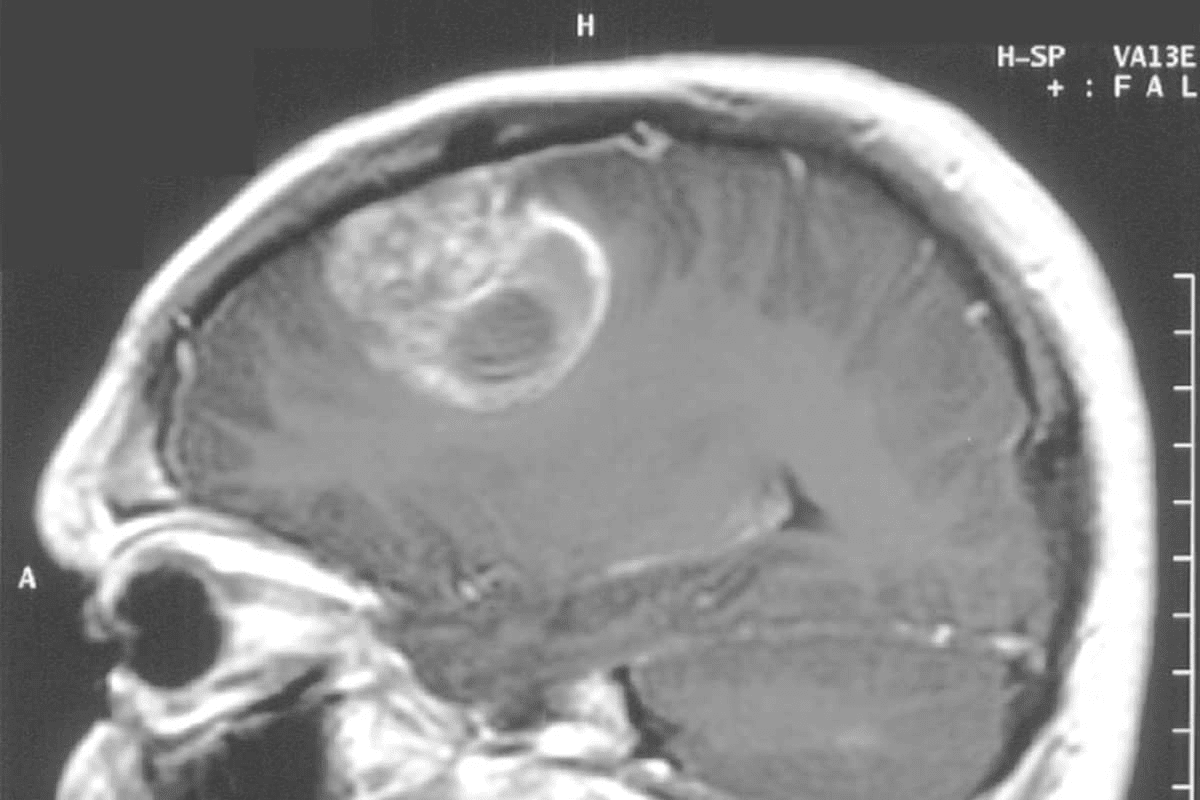
Understanding childhood cancer is key to helping survivors and their families. It’s a complex disease with many types, like leukemia and brain tumours.
In the U.S., over 500,000 people survived childhood cancer thanks to medical progress. Every year, about 16,000 kids from 0 to 19 get cancer. And more than 85% of them live for at least 5 years.
Common Types of Childhood Cancers
Childhood cancers vary a lot. Each type has its own challenges. Here are some common ones:
- Leukemia: It’s the most common, making up about 30% of childhood cancers. It affects the blood and bone marrow.
- Brain and Central Nervous System Tumors: These are the second most common. They can be very different in how severe they are.
- Lymphomas: This includes Hodgkin and non-Hodgkin lymphoma. They affect the immune system.
- Other Types: Like neuroblastoma and Wilms tumour. Each needs a special treatment plan.
A leading oncologist said,
“The diversity of childhood cancers means we need a custom treatment plan. Precision medicine is key.”

erroneous text on image
Prevalence and Incidence Rates
The numbers of childhood cancers are important to understand. The rate hasn’t changed much in years. But, more kids are surviving thanks to better treatments.
Today, over 85% of kids with cancer live for at least 5 years. This is thanks to better treatments like chemotherapy and surgery.
More survivors mean more challenges. We need to keep up with their care and manage long-term effects. It’s vital for their health.
As we keep improving survival rates, we must also focus on survivors’ long-term health. We want them to live happy, healthy lives.
Understanding Childhood Cancer Survival Statistics
It’s key to know the survival stats of childhood cancer. This helps us see how well treatments work and where we can get better. We’ve made big steps forward, and it’s important to look at trends and what affects survival rates.
Historical Trends in Survival Rates
Survival rates for childhood cancer have greatly improved over time. Back in the mid-1970s, the five-year survival rate was about 58%. Now, it’s over 85%. This shows how far we’ve come in treatments and healthcare.
Also, life expectancy for survivors has grown. In the 1970s, it was 48.5 years extra. By the 1990s, it jumped to 57.1 years. This shows how modern treatments are helping kids live longer.
erroneous stats on image
Current Five-Year Survival Rates
Today, the five-year survival rate for kids with cancer is over 85%. This rate changes based on the cancer type. For example, acute lymphoblastic leukemia (ALL) survival rates have soared, now over 90% in many cases.
- Improved Treatment Protocols: Better chemotherapy, radiation, and surgery have helped a lot.
- Early Detection: Catching cancer early and acting fast has greatly improved survival.
- Multidisciplinary Care: A team approach to treatment has made care better.
Factors Affecting Survival Outcomes
Many things can affect how well a child with cancer does. These include the cancer type and stage, the child’s age, and health. Also, how well the treatment works and any genetic factors can play a role.
Knowing these factors helps us tailor treatments. We aim to improve survival chances and reduce side effects. We keep learning and improving to help more kids survive cancer.
Life Expectancy of Childhood Cancer Survivors
Medical treatments for childhood cancer have gotten better. This makes knowing how long survivors live very important. Survivors face special challenges that can affect their life span. We’ll look at how life expectancy has changed over time, the difference between survivors and others, and how cancer type and treatment play a role.
Comparing Life Expectancy Across Decades
Studies show that survivors’ life expectancy has gone up over the years. Those diagnosed in the 1990s can live up to 57.1 years, compared to 48.5 years for those in the 1970s. This better life expectancy comes from new treatments and care.
Key statistics highlighting the improvement in life expectancy include:
- Survivors from the 1990s live longer than those from earlier decades.
- Despite the progress, survivors’ life expectancy is lower than the general population’s.
- New treatments and care have helped increase life expectancy.
Gap Between Survivors and General Population
Even with progress, a gap in life expectancy between survivors and the general population remains. Survivors face higher risks of late effects from treatment, like secondary cancers and organ damage. These can shorten their life expectancy.
The factors contributing to this gap include:
- The type and intensity of the treatment received.
- The presence of late effects, such as secondary cancers or organ damage.
- Lifestyle and environmental factors that can influence overall health.
Variations by Cancer Type and Treatment
Life expectancy among survivors varies a lot based on cancer type and treatment. For example, leukemia survivors have different life expectancy compared to those with other cancers.
Our analysis shows the need to consider these factors when looking at survivors’ long-term outcomes. Healthcare providers can improve care and life expectancy by understanding these differences. This helps in making follow-up care more effective for survivors.
Long-Term Health Challenges for Survivors
Childhood cancer survivors often face many long-term health challenges. These challenges can greatly affect their quality of life. As survival rates improve, it’s key to understand and tackle these issues for better care.
Risk of Secondary Cancers
One big risk for survivors is getting secondary cancers. More than 95% of adults who have survived childhood cancer will develop a significant health problem related to their childhood cancer diagnosis or its treatment by age 45. Treatments like radiation and chemotherapy increase this risk.
It’s vital to have long-term follow-up care to manage these risks. Regular screenings and check-ups can help catch and treat secondary cancers early.
Chronic Health Conditions by Age 65
About 55% of childhood cancer survivors will have at least one major chronic health condition by age 65. These can include heart diseases and endocrine disorders, greatly affecting their quality of life.
- Cardiovascular diseases
- Endocrine disorders
- Neurological complications
- Musculoskeletal problems
Knowing about these conditions helps healthcare providers offer better care. They can target interventions to lessen their impact.
Organ-Specific Late Effects
Childhood cancer treatments can harm specific organs. For instance, radiation to the chest can cause heart problems. Certain chemotherapy can damage kidneys.
“The late effects of childhood cancer treatment can be profound, affecting multiple organ systems and requiring a multidisciplinary approach to manage effectively.”
Expert in Pediatric Oncology
A detailed care plan is essential. It should include monitoring for these late effects. This way, we can intervene early and improve survivors’ long-term outcomes.
Does Chemotherapy Shorten Life Expectancy?
It’s important to understand how chemotherapy affects life expectancy in childhood cancer survivors. Chemotherapy has greatly improved survival rates in kids with cancer. But, there’s ongoing debate about its long-term effects.
Short-term vs. Long-term Effects
Chemotherapy’s immediate effects are often managed well with supportive care. But, its long-term effects can be complex. Modern chemotherapy has reduced toxicity and improved outcomes.
Some chemotherapy agents can cause late effects like heart disease or secondary cancers. These effects might shorten life expectancy. We need to look at these factors when assessing chemotherapy’s impact.
Modern Protocols and Reduced Toxicity
New chemotherapy protocols have lowered toxicity without losing effectiveness. Modern treatments aim to reduce long-term risks while fighting cancer well. For example, targeted therapies and precision medicine have improved treatment precision.
Recent studies show these advancements are key to better quality of life for survivors.
Balancing Treatment Efficacy and Long-term Outcomes
It’s vital to balance chemotherapy’s effectiveness with its long-term effects. We aim to create treatments that cure cancer and minimize late effects. This involves a team effort, using the latest research and guidelines.
By optimizing treatment, we can improve survivors’ long-term health and life expectancy. Continuous healthcare advancements are essential for better survivorship outcomes.
Survivorship Care: Monitoring and Management
Comprehensive care is key for childhood cancer survivors. As more kids beat cancer, we focus on making their lives better. This means improving their quality of life.
Long-term Follow-up Guidelines
Good long-term care means watching and checking for late effects. It’s all about a plan that fits each child. This plan considers the cancer type, treatment, and risk factors.
- Regular check-ups with healthcare providers
- Screening for late effects
- Management of chronic health conditions
Screening for Late Effects
Screening for late effects is a big part of survivor care. It helps catch secondary cancers, heart issues, and other problems. These can come from cancer treatment.
- Annual follow-up visits
- Risk-based screening protocols
- Patient education on self-care and risk reduction
Multidisciplinary Approach to Survivor Care
A team effort is essential for childhood cancer survivors. Doctors, nurses, and specialists work together. They tackle the complex needs of survivors.
This team work and following guidelines boost the life expectancy of childhood cancer survivors. It also improves their quality of life.
Places like LivHospital show the value of full support. They help raise pediatric cancer survival rates.
Advancements Improving Long-Term Outcomes
New medical tech and treatment methods are making a big difference for childhood cancer survivors. These changes are not just raising survival rates. They’re also making life better for those who beat cancer.
Precision Medicine and Targeted Therapies
Precision medicine is changing how we treat childhood cancer. It tailors treatments to each patient’s cancer, making them more effective and less harsh. Targeted therapies focus on cancer’s growth drivers, a more precise method than old-school chemo.
For example, treatments for the BRAF gene in some leukemias are showing great results. This custom treatment is boosting survival chances and cutting down on long-term health problems for kids who’ve had cancer.
Reduced Intensity Treatments
Reduced intensity treatments are another big step forward. They aim to keep treatment effective but with fewer side effects. By making chemotherapy and radiation less intense, we lower the risk of late effects like secondary cancers and organ damage. This helps survivors stay healthy longer.
- Researchers are looking into reduced intensity chemo for some childhood cancers.
- New radiation therapy methods, like proton therapy, are protecting more healthy tissue from radiation.
Preventive Strategies for Late Effects
Preventing late effects is key to survivor care. Scientists are working on ways to lessen the long-term effects of cancer treatment. This includes finding ways to protect the heart from some chemotherapies and preserving fertility.
By tackling these late effects early, we can greatly improve the lives of childhood cancer survivors. Our goal is to give them care that goes beyond treatment. We want to help them live healthy, happy lives.
Conclusion: The Future for Childhood Cancer Survivors
Looking at childhood cancer, we see big steps forward. The five-year survival rate for kids with cancer is now about 85%. This shows how far we’ve come in treating childhood cancer survivors.
Over the years, pediatric cancer survival rates have gone up a lot. Thanks to new research and treatments, the outlook for childhood cancer survivors keeps getting better. We’re hopeful for even more progress in the future.
To keep moving forward, we need to keep improving care and treatments. Using precision medicine and targeted therapies can make a big difference. It’s also key to focus on preventing late effects. By working together, we can make sure childhood cancer survivors have the best possible life.
FAQ
What is the current 5-year survival rate for childhood cancers?
How has the survival rate for childhood cancer changed over the decades?
What are the most common types of childhood cancers?
Do childhood cancer survivors have a lower life expectancy than the general population?
How does chemotherapy impact life expectancy in childhood cancer survivors?
What are the long-term health challenges faced by childhood cancer survivors?
What is the importance of long-term follow-up care for childhood cancer survivors?
How are advancements in treatment improving long-term outcomes for childhood cancer survivors?
What is the life expectancy of childhood leukemia survivors?
Can modern chemotherapy regimens reduce the risk of long-term effects?
References
- Bhandari, R., Hudson, M. M., & Oeffinger, K. C. (2025). A report from the Childhood Cancer Survivor Study (CCSS). PubMed Central.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12342639/