Last Updated on November 26, 2025 by Bilal Hasdemir

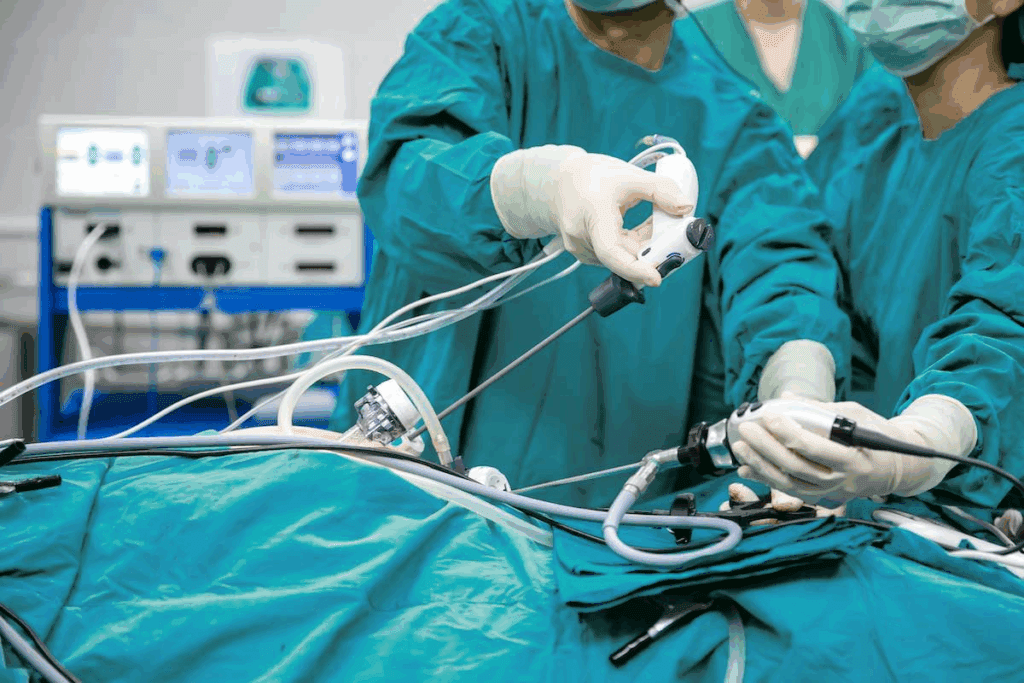
Understanding cholecystectomy anatomy is essential for surgeons to safely and successfully remove the gallbladder. It involves a clear knowledge of key structures such as the cystic duct, cystic artery, and the triangle of Calot.
The triangle of Calot is a critical landmark, located where the cystic duct, common hepatic duct, and the liver edge meet. Mastery of this area helps prevent complications during surgery and ensures better outcomes.
At Liv Hospital, precision and patient safety come first. Our surgeons perform each cholecystectomy with deep anatomical understanding and advanced techniques, ensuring optimal care and recovery.
Cholecystectomy anatomy is key to the success of gallbladder removal surgery. It’s important for surgeons to know the basics well. This helps them handle the surgery’s challenges.
The success of cholecystectomy depends on knowing the lap cholecystectomy anatomy well. Important parts include the cystic duct, cystic artery, and the triangle of Calot. These are vital for safe cutting and tying off.
The triangle of Calot is a key landmark. It’s bordered by the cystic duct, common hepatic duct, and the liver edge. It holds the cystic artery and other important parts. Knowing these relationships helps avoid problems.
Knowing these structures well makes cholecystectomy safe and successful.

The gallbladder’s anatomy, including its location and peritoneal coverings, is key in cholecystectomy. Knowing these details is vital for surgeons to handle the complexities of laparoscopic cholecystectomy anatomy.
The gallbladder sits under the liver, in a fossa between liver segments IVb and V. It can grow up to 10 cm long. Its spot in the hepatic fossa is key for knowing its attachments and blood flow. The hepatic bed relationship is important for the surgical method during cholecystectomy.
The gallbladder has peritoneum on its free side, linked to the liver’s peritoneum. The peritoneal coverings and ligamentous attachments, like the cystic plate, are vital for understanding the gallbladder’s anatomical relationships. These must be managed with care during surgery to prevent damage to nearby areas.
Surgeons need to know these details for a safe and successful cholecystectomy. This shows the critical role of lap chole anatomy in planning the surgery.
Knowing the triangle of Calot’s borders and contents is key for a successful cholecystectomy. This triangle is a vital landmark. It helps surgeons avoid harming important structures during surgery.
The triangle of Calot is defined by the cystic duct, the common hepatic duct, and the edge of the liver. It’s important for surgeons to know these borders well. This knowledge helps them navigate the complex anatomy safely.
Inside the triangle of Calot are vital structures that need to be found and kept safe during surgery. These include the cystic artery and the lymph node of Lund. The cystic artery, often coming from the right hepatic artery, supplies blood to the gallbladder. It must be carefully tied off to prevent bleeding.
Safe dissection in the triangle of Calot is essential to avoid harming vital structures. Techniques include:
By understanding the anatomy of the triangle of Calot and using safe dissection techniques, surgeons can lower the risk of complications during laparoscopic cholecystectomy.
Knowing the anatomy of the cystic duct is key for surgeons doing cholecystectomy. It connects the gallbladder to the common bile duct. Its shape can change how surgeons operate.
The cystic duct usually meets the common bile duct at the gallbladder neck. This is important for bile to flow from the gallbladder. Differences in its length and size can make surgery harder.
The cystic duct’s length and size can differ a lot. A longer duct might need more careful cutting during surgery. A bigger size could mean using different tools.
| Cystic Duct Characteristic | Variation | Surgical Implication |
| Length | Short, Long | Dissection complexity |
| Diameter | Narrow, Wide | Instrument choice |
| Course | Direct, Tortuous | Ligation technique |
Changes in the cystic duct’s shape, like an extra duct or a weird path, can make surgery harder. Imaging before surgery and special tests during it can spot these issues. Surgeons need to adjust their methods.
Understanding the cystic duct’s shape and any changes is vital for safe gallbladder removal. This knowledge helps surgeons handle the challenges of removing the gallbladder.
The cystic artery is key in gallbladder surgery. It must be found accurately to prevent problems. Finding this artery right is essential for cholecystectomy success.
The cystic artery usually comes from the right hepatic artery. It goes through the Triangle of Calot to reach the gallbladder. Knowing this path is vital for surgeons.
Not all cystic arteries follow the same path. They can start from the left hepatic artery, the proper hepatic artery, or even the aorta. Knowing about these differences is key for safe surgery.
“The cystic artery’s variability highlights the importance of careful dissection and identification during cholecystectomy.”
Safe cystic artery ligation means knowing its start and path. Surgeons need to dissect carefully to avoid mistakes. Intraoperative imaging helps confirm the anatomy.
Understanding the usual anatomy, knowing about common changes, and using safe surgery methods help reduce risks during cholecystectomy.
Understanding the biliary tree’s relationships is key for surgeons doing cholecystectomies. The complex anatomy of the biliary tree is vital in laparoscopic surgeries. Knowing its structure helps avoid complications.
The common bile duct forms from the cystic duct and the common hepatic duct joining. Accurate identification of this area is critical to avoid bile duct injuries during surgery. Knowing about possible variations in anatomy is also important for surgeons.
Hepatic duct configurations vary among people. Usually, the right and left hepatic ducts merge to form the common hepatic duct. But, anatomical variations like extra hepatic ducts or wrong duct insertions can make surgery harder.
The junctions between the cystic duct and the common bile duct are very important for surgery. A low junction can raise the risk of bile duct injury if not spotted right. Knowing these junction patterns is key for safely cutting and tying the cystic duct during cholecystectomy.
By understanding the biliary tree’s anatomy and its variations, surgeons can make laparoscopic cholecystectomy safer and more effective.
For surgeons, knowing the anatomy of laparoscopic cholecystectomy is key. This procedure is complex due to the two-dimensional view from the laparoscope. It also requires precise dissection.
The laparoscope gives a special view of the gallbladder and its surroundings. Important landmarks include Calot’s triangle, the cystic duct, and the cystic artery. Knowing these is vital for safe surgery and avoiding problems.
Where the laparoscopic ports are placed is very important. They are usually in a subcostal position for better access. The exact placement must match the patient’s anatomy to avoid harming vital areas.
Creating pneumoperitoneum changes how organs are positioned in the belly. The use of carbon dioxide can move the liver and gallbladder. Surgeons need to understand these changes to safely perform the surgery.
Ensuring the critical view of safety is key to avoiding bile duct injuries during cholecystectomy. This method involves careful dissection to clearly see the cystic duct and artery before they are tied off.
The critical view of safety is met when three things happen: the hepatocystic triangle is cleared of all fibrofatty tissue, the lower end of the gallbladder is separated from the liver, and only two structures are seen entering the gallbladder. Clear identification of the cystic duct and artery is very important.
A stepwise dissection starts with cutting the peritoneum on both sides of the gallbladder. Then, the dissection clears the hepatocystic triangle of fibrofatty tissue, showing the cystic duct and artery. Careful dissection is key to avoid damaging these structures.
Verification of the critical view means confirming the cystic duct and artery are the only two structures entering the gallbladder. This can be helped by intraoperative imaging techniques. It’s also important to document the critical view for quality assurance.
By following these steps and ensuring the critical view of safety, surgeons can greatly reduce the risk of complications during cholecystectomy.
Knowing about high-risk anatomical variants is key for safe cholecystectomy procedures. Changes in biliary and vascular anatomy can raise the risk of complications during gallbladder removal surgery.
Surgeons must spot aberrant and accessory bile ducts to avoid injuries. These ducts are often in unusual spots, making them easy to damage during surgery.
Vascular anomalies, like changes in the cystic artery or aberrant hepatic arteries, can make cholecystectomy harder. It’s vital to understand these variations for safe ligation and dissection.
Key vascular anomalies include:
Congenital gallbladder variations, like a duplicated or intrahepatic gallbladder, can be tricky during cholecystectomy. Knowing about these variations before surgery helps surgeons plan a safer approach.
Surgeons need to be aware of these high-risk anatomical variants to avoid complications and ensure successful outcomes in cholecystectomy procedures.
Intraoperative imaging is key in making anatomy clear during cholecystectomy. It helps surgeons deal with complex biliary anatomy. This reduces the chance of complications.
Intraoperative cholangiography is a great tool for seeing the biliary tree during laparoscopic cholecystectomy. It involves putting contrast material into the bile ducts to spot anomalies or stones. Real-time imaging lets surgeons decide if more steps are needed.
Intraoperative ultrasound gives real-time feedback on anatomy and possible problems. It’s great for finding bile duct stones or issues that aren’t seen other ways.
Fluorescence imaging is a big step forward in intraoperative imaging. It makes biliary anatomy clearer. This is because it uses fluorescent dyes to light up important structures. It makes dissection more accurate and lowers the risk of harming key areas.
Using these imaging techniques together makes laparoscopic cholecystectomy safer and more effective.
Dealing with tough cholecystectomy anatomy is a big challenge for surgeons. They need to know about different anatomies and how to change their approach. Acute inflammation and fibrosis can make it hard to cut through tissues.
When there’s acute inflammation, it can cause swelling and adhesions. This makes it hard to find important structures. Surgeons have to be careful and use other landmarks to find their way.
Fibrosis and scarring from past problems or surgeries can hide key structures. Using intraoperative imaging can help see the anatomy better.
If the anatomy is too complex or risky for laparoscopy, surgeons might need to switch to open surgery. They should only do this if it’s safe and necessary.
Handling tough cholecystectomy anatomy needs skill, knowledge, and advanced techniques. Understanding the problems caused by inflammation, fibrosis, and complex anatomy helps surgeons do better in lap chole anatomy procedures.
Knowing the anatomy of the gallbladder is vital for surgeons. It helps them do the surgery safely and well. The gallbladder’s complex structure and its many variations mean surgeons need to know a lot about laparoscopic cholecystectomy anatomy.
Using anatomical knowledge is essential for the best results in cholecystectomy. Surgeons can handle the surgery’s challenges better. This includes dealing with different anatomies and possible problems.
The importance of gallbladder anatomy in surgery cannot be ignored. It greatly affects how well the surgery goes. Knowing the anatomy well helps surgeons spot and deal with risks. This leads to better care for patients.
Knowing cholecystectomy anatomy is key for surgeons. It helps them remove the gallbladder safely and well. This reduces risks and leads to better results.
Surgeons need to know about the cystic duct, cystic artery, and the triangle of Calot. These are important for the surgery.
The triangle of Calot is defined by the cystic duct, common hepatic duct, and the liver’s edge.
The triangle of Calot is a key area. It must be identified carefully to ensure the cystic duct and artery are safely cut and tied.
The cystic duct can vary in length and size. Knowing these variations is important for safe surgery.
The cystic artery is found by knowing its usual path and origin. Surgeons also look out for any unusual variations.
The critical view of safety means seeing the cystic duct and artery clearly. This ensures they are safely tied off, reducing the risk of injury.
Imaging like cholangiography and ultrasound helps during surgery. It clarifies the anatomy and lowers the risk of problems.
High-risk variations include unusual bile ducts, vascular issues, and congenital gallbladder changes. These need careful handling.
Dealing with tough anatomy requires a deep understanding of variations. Surgeons must be flexible and ready to adapt or switch to open surgery if needed.
Pneumoperitoneum changes how structures relate to each other. It’s important for surgeons to understand these changes for safe dissection and ligation.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!