Last Updated on November 26, 2025 by Bilal Hasdemir

Learn 7 critical choledocholithiasis symptoms. These bad signs of a bile duct stone require urgent diagnosis and treatment.
Gallstones in the bile duct can cause abdominal pain, jaundice, and fever. Knowing these symptoms and how doctors diagnose them is important. This helps manage the condition well.
Liv Hospital offers multidisciplinary expertise and care focused on the patient. They ensure a complete treatment plan for this complex issue.
Key Takeaways
- Choledocholithiasis needs quick diagnosis and treatment.
- Common symptoms include abdominal pain, jaundice, and fever.
- Diagnostic approaches include ultrasound.
- Treatment options are available to manage the condition.
- Liv Hospital offers specialized care for choledocholithiasis.
Understanding Choledocholithiasis: Definition and Pathophysiology

To grasp choledocholithiasis, we must understand how stones form in the common bile duct. This condition occurs when gallstones block the common bile duct. This blockage can lead to serious health issues.
What is Choledocholithiasis?
Choledocholithiasis is when gallstones are in the common bile duct. It’s divided into primary and secondary types. Primary stones form in the bile duct, while secondary stones come from the gallbladder.
Pathophysiology and Stone Formation
The formation of stones in the biliary system is complex. Stones can form in the bile duct (primary) or move from the gallbladder (secondary). Factors like bile stasis, infection, and changes in bile composition play a role.
Types of Common Bile Duct Stones
There are different types of stones in the common bile duct. These include:
| Stone Type | Description | Characteristics |
| Cholesterol Stones | Primarily made of cholesterol | Usually not visible on X-rays, linked to supersaturated bile |
| Pigment Stones | Made of bilirubin and pigments | Linked to hemolysis, infection, or stasis |
| Mixed Stones | Both cholesterol and pigment | Most common, often seen in chronic inflammation |
Knowing about the different stones and how they form is key. It helps doctors diagnose and treat choledocholithiasis. Understanding the types of stones helps predict complications and guide treatment.
Choledocholithiasis Symptoms and Clinical Manifestations
People with choledocholithiasis often have symptoms like right upper quadrant pain, jaundice, and changes in stool and urine. These signs are key for diagnosing and treating the condition.
Right Upper Quadrant Abdominal Pain
Right upper quadrant pain is a common symptom. It can feel sharp or colicky. This pain might spread to the right shoulder or back, getting worse with fatty meals.
The pain comes from the blockage by bile duct stones.
Jaundice and Visible Symptoms
Jaundice, or yellow skin and eyes, is another symptom. It happens when bile flow is blocked, causing bilirubin buildup. Skin itching and dark urine with pale stools are also signs.
Systemic Symptoms: Fever and Chills
Fever and chills can happen if the condition leads to infection. These symptoms mean a more serious issue, like cholangitis, and need quick medical help.
Changes in Stool and Urine Appearance
Stools and urine color changes are signs of bile flow blockage. Stools may look pale or clay-colored, and urine darkens. These changes point to choledocholithiasis.
In summary, choledocholithiasis symptoms include abdominal pain, jaundice, fever, and changes in stool and urine. Spotting these signs is vital for early diagnosis and treatment.
Etiology and Risk Factors for Choledocholithiasis
Choledocholithiasis has many causes, including genetics and health conditions. Knowing these causes helps us find who’s at risk and how to prevent it.
Primary vs. Secondary Stone Formation
Choledocholithiasis can come from primary or secondary stones. Primary stones form in the bile duct, often due to blockages or infections. Secondary stones start in the gallbladder and move to the bile duct.
Primary stone formation is rare but complex, linked to bile duct issues. Secondary stone formation is more common, tied to gallstones.
Demographic and Genetic Predispositions
Some groups are more likely to get choledocholithiasis. Age, gender, and ethnicity matter a lot. It’s more common in older adults and women.
- Age: The risk goes up after 40.
- Gender: Women are more at risk, thanks to hormones.
- Ethnicity: Some groups get more gallstones, which can move to the bile duct.
Medical Conditions Increasing Risk
Some health issues raise the risk of choledocholithiasis. These include:
| Condition | Description | Risk Factor |
| Cholelithiasis | Presence of gallstones | High risk of stone migration into CBD |
| Biliary Strictures | Narrowing of the bile duct | Increased risk of primary stone formation |
| Parasitic Infections | Infections such as Clonorchis sinensis | Associated with primary stone formation |
Knowing about these risk factors is key to spotting and treating choledocholithiasis early. By finding at-risk individuals, doctors can take steps to prevent and treat it.
Diagnostic Approaches for Choledocholithiasis
Diagnosing choledocholithiasis involves several tools, from simple tests to advanced imaging. Getting the diagnosis right is key to managing the condition well and avoiding serious problems.
Laboratory Tests: Liver and Pancreatic Enzymes
Laboratory tests are essential in the early stages of diagnosing choledocholithiasis. Tests like serum bilirubin, alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT) show if the bile duct is blocked. High levels of pancreatic enzymes, like amylase and lipase, suggest pancreatitis.
Liver enzyme tests are important for spotting bile duct blockages, a common issue with choledocholithiasis. These tests help figure out how severe the blockage is and guide further steps.
Abdominal Ultrasound Findings in Choledocholithiasis
Abdominal ultrasound is often the first imaging test for suspected choledocholithiasis. It’s non-invasive and can spot dilated bile ducts and sometimes stones in the common bile duct. But, its ability to find stones depends on the skill of the operator and can be affected by bowel gas and body shape.
Advanced Imaging: MRCP and CT Scans
For those with a strong suspicion of choledocholithiasis, MRCP or CT scans are often needed. MRCP is very good at showing the biliary tree without contrast. CT scans can also show bile duct dilatation and stones, though they might miss small ones.
Risk Stratification Systems
Risk stratification systems help predict the chance of choledocholithiasis based on symptoms and lab results. These systems guide which tests and treatments to use. Patients are put into low, intermediate, or high-risk groups based on symptoms like jaundice, abnormal liver tests, and ultrasound results.
By accurately sorting patients, doctors can make the best use of tests and treatments. This means saving more invasive and expensive procedures for those who really need them.
Differential Diagnosis of Choledocholithiasis
Choledocholithiasis can look like other biliary and pancreatic issues. It’s important to do a detailed differential diagnosis. When checking patients for choledocholithiasis, we must think about other conditions that might show similar signs.
Biliary Colic and Cholecystitis
Biliary colic and cholecystitis are linked to choledocholithiasis in symptoms and causes. Biliary colic causes pain in the right upper area, often from fatty foods. Cholecystitis is inflammation of the gallbladder, with severe pain, fever, and high white blood cell count.
- Biliary colic is treated with pain relief.
- Cholecystitis might need antibiotics and sometimes surgery.
Acute Cholangitis
Acute cholangitis is a bile duct infection, often from blockage. It shows Charcot’s triad: fever, jaundice, and pain in the right upper area. It’s key to spot acute cholangitis because it can lead to serious problems like sepsis.
Pancreatitis and Other Pancreaticobiliary Disorders
Pancreatitis can happen when gallstones block the pancreatic duct. It’s diagnosed by high pancreatic enzymes, pain, and imaging. Other issues like sphincter of Oddi dysfunction and biliary dyskinesia should also be thought of.
- Pancreatitis treatment includes supportive care and pain relief.
- Sphincter of Oddi dysfunction might need surgery.
Non-Biliary Causes of Similar Symptoms
Other non-biliary problems, like peptic ulcers, hepatitis, and pneumonia, can also cause similar symptoms. A detailed history, physical check, and tests are needed to correctly diagnose choledocholithiasis and rule out other conditions.
| Condition | Key Features | Diagnostic Approach |
| Biliary Colic | Intermittent right upper quadrant pain | Ultrasound, clinical history |
| Cholecystitis | Severe pain, fever, leukocytosis | Ultrasound, laboratory tests |
| Acute Cholangitis | Fever, jaundice, right upper quadrant pain | Blood cultures, imaging studies |
Treatment Options for Choledocholithiasis
Understanding the treatment for choledocholithiasis is key. The right treatment depends on symptoms, health, and complications. Each case is unique.
Conservative Management Approaches
For mild symptoms, conservative management is often used. This includes:
- Monitoring: Regular check-ups to watch symptoms and complications.
- Antibiotics: Antibiotics to prevent or treat infections.
- Pain Management: Medication to manage pain and discomfort.
Endoscopic Interventions
ERCP is a main treatment for choledocholithiasis. During ERCP, doctors can:
- Stone Removal: Take out stones from the bile duct.
- Sphincterotomy: Make the ampulla of Vater wider for stone removal.
- Stent Placement: Use stents to keep the bile duct open.
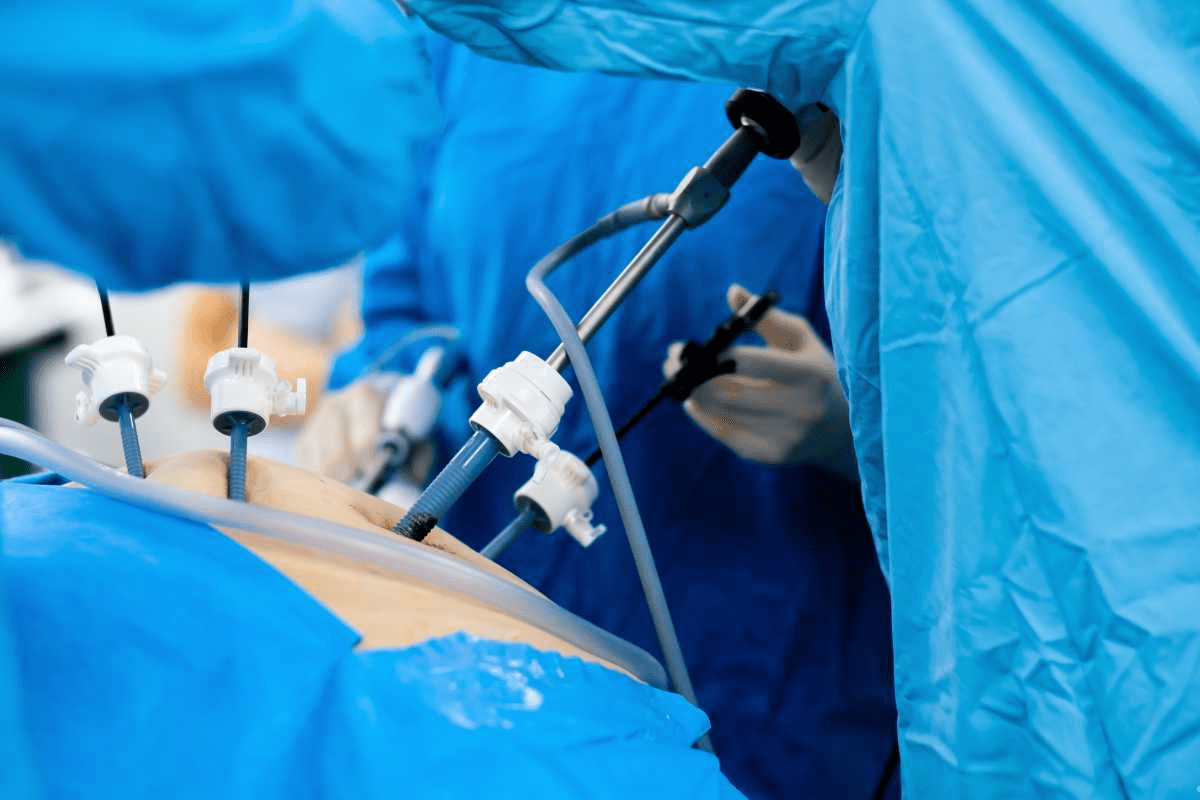
Surgical Management Options
Surgery is needed for complicated cases or when endoscopy fails. Surgical options include:
- Cholecystectomy: Removing the gallbladder, often done laparoscopically.
- Common Bile Duct Exploration: Surgery to clear the bile duct.
Emerging Treatment Modalities
New treatments for choledocholithiasis are being researched. These include:
- Laser Lithotripsy: Using laser energy to break stones.
- Cholangioscopy: Directly seeing the bile ducts to diagnose and treat stones.
Treating choledocholithiasis requires a personalized approach. It must be based on the patient’s needs and the latest research.
ERCP for Choledocholithiasis: Diagnostic and Therapeutic Applications
ERCP is key in diagnosing and treating choledocholithiasis. It lets gastroenterologists see the bile ducts, find blockages, and clear them. This endoscopic method is vital for treatment.
ERCP Procedure: What to Expect
The ERCP starts with an endoscope going through the mouth, stomach, and into the duodenum. A catheter injects dye into the bile ducts for clear images. The whole thing is done under sedation to keep you comfortable.
Key steps in the ERCP procedure include:
- Insertion of the endoscope and guidance to the duodenum
- Injection of contrast dye into the bile ducts
- Visualization of the bile ducts using fluoroscopy
- Performance of sphincterotomy to facilitate stone removal
Stone Removal Techniques
Removing stones during ERCP is a big deal. There are a few ways to do it:
- Sphincterotomy: A small cut in the ampulla of Vater to get the stones out
- Balloon extraction: A balloon catheter pulls out the stones
- Basket extraction: A wire basket catches and removes the stones
The method used depends on the stone’s size and where it is.
Biliary Drainage and Stent Placement
If stones can’t be taken out right away, or if there’s a big blockage, biliary drainage and stent placement might be needed. Stents keep the bile duct open, helping with drainage and preventing infection.
Types of stents used include:
| Stent Type | Description | Duration |
| Plastic Stents | Inexpensive, commonly used for temporary drainage | Several months |
| Metal Stents | More durable, often used for long-term drainage | Several years |
Success Rates and Limitations
ERCP works well for diagnosing and treating choledocholithiasis, with success rates of 85% to 95%. But, it’s not without risks like pancreatitis, bleeding, and infection.
ERCP’s limitations include needing special training and equipment, and the chance of complications. Yet, it’s a key tool in managing choledocholithiasis.
Potential Complications of Choledocholithiasis
Choledocholithiasis can cause serious problems if not treated right. Stones in the bile duct can lead to mild or severe health issues.
Acute Cholangitis and Sepsis
Acute cholangitis is a severe infection of the bile duct. It happens when bacteria get into the duct because of stones. If not treated, it can turn into sepsis, a life-threatening condition.
Symptoms include fever, jaundice, and pain in the right upper abdomen, known as Charcot’s triad. Quick treatment with antibiotics and removing the blockage is key to avoid worse problems.
Biliary Pancreatitis
Biliary pancreatitis is another serious issue. It occurs when a stone blocks the pancreatic duct, causing pancreas inflammation. This can be mild or severe, with severe cases being very dangerous.
Symptoms include severe pain, nausea, and vomiting. Treatment includes fluids, pain relief, and sometimes removing the stone.
Liver and Kidney Failure
Long-term blockage of the bile duct can harm the liver and lead to liver failure. It can also affect the kidneys, causing kidney failure.
Liver and kidney failure are serious and need immediate medical help. Treatment may include addressing the cause, supportive care, and in severe cases, organ transplant.
Post-ERCP Complications
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a common treatment for choledocholithiasis. While safe, it can cause pancreatitis, bleeding, infection, and perforation.
Post-ERCP pancreatitis is a common issue, affecting up to 10% of patients. Risk factors include being young, female, and having a history of pancreatitis. Treatment involves supportive care, and severe cases may need hospitalization.
Antibiotic Therapy in Choledocholithiasis Management
Antibiotics are very important in treating choledocholithiasis, mainly when cholangitis is involved. Stones in the bile duct can cause infections. Antibiotics help prevent serious problems.
Indications for Antibiotic Treatment
Antibiotics are needed for those with choledocholithiasis and signs of cholangitis. This includes fever, jaundice, and pain. Starting antibiotics early is key to avoid sepsis, a serious condition.
Doctors decide on antibiotics based on symptoms, lab results, and risk factors for serious infections.
Recommended Antibiotic Regimens
For choledocholithiasis with cholangitis, antibiotics should fight many types of bacteria. Piperacillin-tazobactam is often the first choice because it works against many bacteria.
- Piperacillin-tazobactam
- Ciprofloxacin plus metronidazole
- Third-generation cephalosporins
Doctors may change the treatment based on local resistance and patient allergies.
Duration and Monitoring of Therapy
Antibiotics are usually given for 7 to 14 days, depending on the infection’s severity and how well the patient responds.
Doctors watch for improvement in symptoms, lab results, and overall health.
Preventing Progression to Sepsis
Starting antibiotics quickly is vital to stop sepsis in choledocholithiasis and cholangitis cases. Sepsis is a serious emergency that needs fast action.
Along with antibiotics, supportive care like fluids and managing organ issues is also important for sepsis treatment.
Conclusion: Multidisciplinary Approach and Future Directions
Managing choledocholithiasis needs a team effort. Gastroenterologists, surgeons, and other experts work together. This teamwork is key to the best patient care.
This team approach lets doctors create treatment plans that fit each patient. They use the newest diagnostic and treatment methods. This way, they can make more accurate diagnoses and better treatments.
Looking ahead, we’ll see more use of less invasive methods like ERCP and laparoscopic surgery. New imaging tech will also help doctors diagnose better.
By working together and using the latest technology, doctors can make care better. This will help avoid complications and improve patient outcomes. It will shape how we manage choledocholithiasis in the future.
FAQ
What is choledocholithiasis?
Choledocholithiasis is when stones block the common bile duct. This can lead to serious problems.
What are the symptoms of choledocholithiasis?
Symptoms include pain in the abdomen, jaundice, fever, and changes in stool and urine.
How is choledocholithiasis diagnosed?
Doctors use tests like liver and pancreatic enzyme tests. They also use imaging like ultrasound, MRCP, and CT scans.
What are the risk factors for developing choledocholithiasis?
Risk factors include certain genetic and demographic traits. Also, medical conditions like cholelithiasis and certain body shapes play a role.
What is the role of ERCP in managing choledocholithiasis?
ERCP is key for diagnosing and treating choledocholithiasis. It allows for removing stones and placing stents.
What are the possible complications of choledocholithiasis?
Complications include infections, pancreatitis, and liver and kidney failure. Post-ERCP issues are also possible.
When is antibiotic therapy indicated for choledocholithiasis?
Antibiotics are used when there’s infection or a high risk of sepsis.
What are the treatment options for choledocholithiasis?
Treatments include watching and waiting, ERCP, surgery, and new methods.
How is choledocholithiasis differentiated from other conditions?
It’s distinguished from similar symptoms like biliary colic and pancreatitis through tests.
What is the importance of prompt diagnosis and treatment of choledocholithiasis?
Quick diagnosis and treatment prevent serious issues and improve health outcomes.
What are the types of stones that can occur in choledocholithiasis?
Stones can be primary, forming in the bile duct, or secondary, coming from the gallbladder.
How does choledocholithiasis affect the body?
It blocks the bile duct, causing jaundice and infection. Untreated, it can lead to serious problems.