
Chronic Lymphocytic Leukemia (CLL) is a type of leukemia that is currently considered incurable with existing treatments.
We’re learning more about CLL and its treatment challenges. Even with medical progress, CLL is a big worry for patients and doctors.
Key Takeaways
- Chronic Lymphocytic Leukemia (CLL) is a type of leukemia that is currently considered incurable with existing treatments.
- It affects the blood and bone marrow.
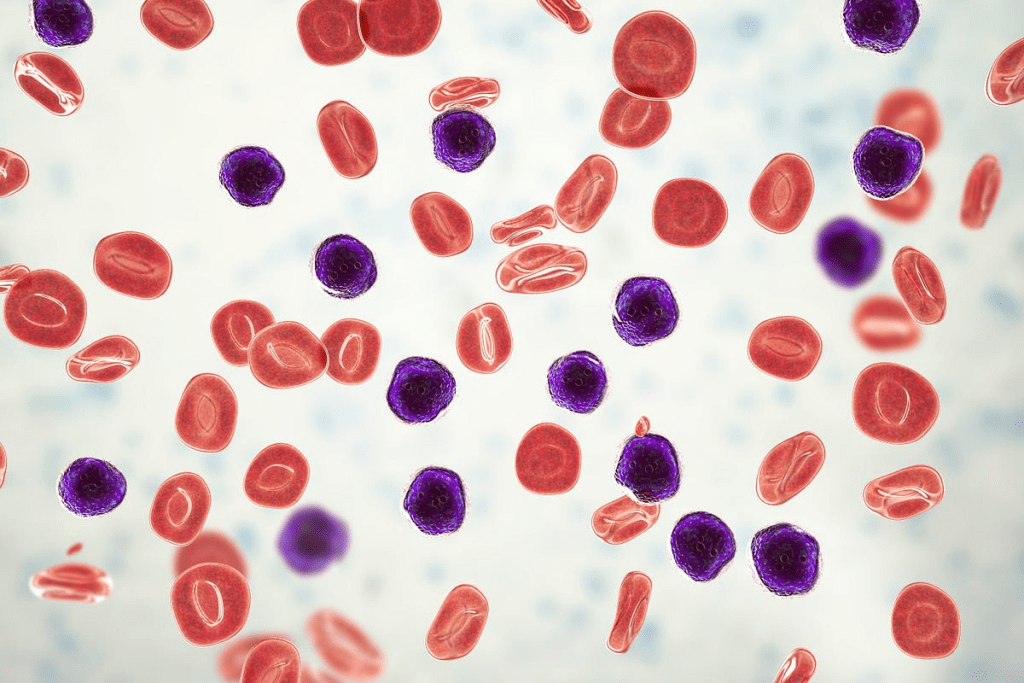
- CLL is characterized by excessive production of immature white blood cells.
- Treatment challenges persist despite medical advancements.
- CLL remains a significant concern for patients and healthcare providers.
The Nature of Blood Cancers
Blood cancers are complex diseases. They affect the blood, bone marrow, and lymphatic system. We will look at what they are, how they are classified, and why they develop.
Definition and Classification of Blood Malignancies
Blood malignancies are divided into three main types: leukemia, lymphoma, and multiple myeloma. Leukemia is when abnormal white blood cells grow too much in the bone marrow. Lymphoma affects the lymphatic system, where lymphocytes are found. Multiple myeloma is a cancer of plasma cells in the bone marrow.
Doctors classify blood cancers based on the affected cell type and disease stage. Knowing this helps choose the right treatment.
| Type of Blood Cancer | Cells Affected | Primary Characteristics |
| Leukemia | White blood cells | Uncontrolled proliferation in bone marrow |
| Lymphoma | Lymphocytes | Originates in the lymphatic system |
| Multiple Myeloma | Plasma cells | Cancer of plasma cells in bone marrow |
The Biology of Blood Cancer Development
Genetic and environmental factors play a role in blood cancer development. Genetic changes can turn normal cells into cancer cells. Exposure to radiation and certain chemicals also increases the risk.
Understanding how blood cancers develop is key to finding effective treatments. Scientists are studying the genetic and molecular causes. They aim to find new ways to treat these diseases.
Types of Blood Cancers and Their Curability
It’s important to know the different blood cancers to understand their cure rates. Blood cancers, or hematologic malignancies, fall into several categories. Each has its own traits and treatment success rates.
Acute vs. Chronic Leukemias
Leukemias are cancers of the blood and bone marrow. They are split into acute and chronic types. Acute leukemias grow fast and need quick treatment. Chronic leukemias grow slower, sometimes allowing for watchful waiting before starting treatment.
Acute leukemias, like Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML), are aggressive. They need strong chemotherapy. Some, like kids with ALL, can be cured. Others might need bone marrow transplants.
| Chronic Lymphocytic Leukemia (CLL) is a type of leukemia that is currently considered incurable with existing treatments. | Characteristics | Curability |
| Acute Lymphoblastic Leukemia (ALL) | Aggressive, rapid progression | High cure rate, mostly in children |
| Acute Myeloid Leukemia (AML) | Aggressive, rapid progression | Variable cure rate, based on genetics |
| Chronic Lymphocytic Leukemia (CLL) | Slow progression, often no symptoms at first | Currently seen as incurable with standard treatments |
| Chronic Myeloid Leukemia (CML) | Slow progression, can speed up | Manageable with targeted therapy, but not curable |
Lymphomas: Hodgkin’s and Non-Hodgkin’s
Lymphomas are cancers of the lymphatic system. They are mainly Hodgkin’s lymphoma and Non-Hodgkin’s lymphoma. Hodgkin’s lymphoma has a high cure rate with the right treatment.
Non-Hodgkin’s lymphoma is more varied. It includes many subtypes, from slow-growing to aggressive. The cure rate for Non-Hodgkin’s lymphoma depends on the subtype and how early it’s caught.
Multiple Myeloma and Other Plasma Cell Disorders
Multiple myeloma is a cancer of plasma cells in the bone marrow. It makes abnormal proteins and can cause bone damage, anemia, and kidney problems. Despite better treatments, curing multiple myeloma is hard.
Other plasma cell disorders include monoclonal gammopathy of undetermined significance (MGUS) and Waldenström’s macroglobulinemia. These can sometimes turn into multiple myeloma or other cancers.
Understanding Chronic Lymphocytic Leukemia
Chronic Lymphocytic Leukemia (CLL) is a serious health issue. We need to look into its causes, genetic makeup, and how it progresses. This will help us understand CLL better, including its definition, traits, and what affects its growth.
Defining CLL and Its Characteristics
CLL is when too many lymphocytes build up in the blood, bone marrow, and lymph nodes. The disease can progress at different rates. Some people may have a slow-moving disease, while others face a faster-growing one.
- Accumulation of lymphocytes in the blood and bone marrow
- Variable clinical course, ranging from indolent to aggressive
- Presence of specific genetic and molecular markers
Epidemiology and Risk Factors
CLL’s occurrence varies worldwide, with more cases in Western countries. Genetic predisposition, family history, and exposure to toxins increase the risk. Knowing these factors helps in early detection and treatment.
Genetic and Molecular Features of CLL
CLL has unique genetic and molecular traits, like deletions and mutations. Key genetic features include deletions of 13q14, trisomy 12, and TP53 gene mutations. These traits affect how the disease progresses and help decide treatment options.
Studying CLL’s genetic and molecular traits helps us grasp its underlying causes. It also points to possible treatments.
Recognizing Chronic Lymphocytic Leukemia Symptoms
Knowing the common symptoms of CLL can help you get medical help sooner. CLL often starts slowly and may not show symptoms early on. But as it gets worse, you might notice different signs.
Early Warning Signs and Common Symptoms
The first signs of CLL can be hard to spot and may look like other illnesses. They include:
- Fatigue or feeling weak
- Weight loss
- Swollen lymph nodes
- Enlarged spleen
- Frequent infections
- Bleeding or bruising easily
These symptoms can be tricky to figure out on your own. Getting a proper diagnosis needs a full medical check-up.
When to Seek Medical Attention
If you keep getting symptoms like:
- Recurring infections
- Unexplained weight loss
- Significant fatigue
- Easy bruising or bleeding
It’s important to see a doctor. They can run tests to find out what’s wrong.
Differentiating CLL from Other Conditions
To tell CLL apart from other diseases, doctors use:
- Blood tests to check for abnormal lymphocyte counts
- Bone marrow examination to assess the extent of CLL cell infiltration
- Imaging studies to evaluate lymph node and spleen size
| Symptom | CLL | Other Conditions |
| Fatigue | Common in CLL due to anemia | Can be caused by various conditions including anemia, diabetes, and depression |
| Swollen Lymph Nodes | Often present in CLL | Can be caused by infections, other cancers, or autoimmune diseases |
| Frequent Infections | CLL impairs immune function | Can be due to immunodeficiency, diabetes, or other chronic conditions |
Getting the right diagnosis is key for the right treatment. If you’re worried about your symptoms, don’t wait to see a doctor.
Diagnosis and Staging of CLL
Diagnosing Chronic Lymphocytic Leukemia (CLL) requires a mix of clinical checks and special tests. We’ll look at the main tests and systems for understanding CLL’s extent and future outlook.
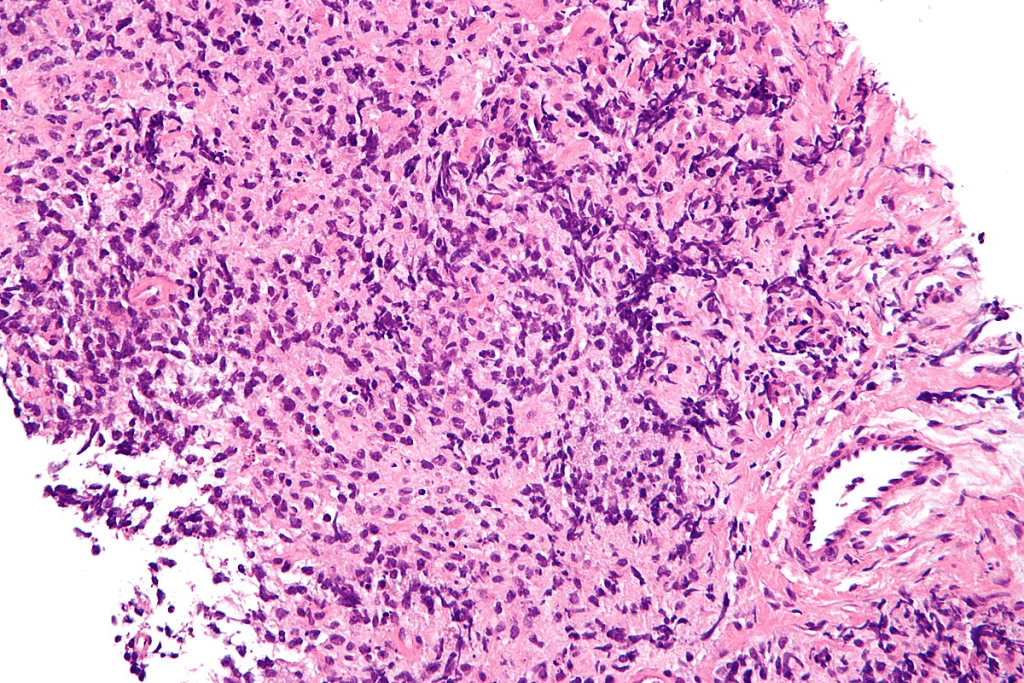
Blood Tests and Bone Marrow Examination
The first step in diagnosing CLL is blood tests. These tests check for lymphocytes, a type of white blood cell. A complete blood count (CBC) and flow cytometry are key for spotting CLL’s abnormal lymphocytes.
A bone marrow examination might also be done. It includes a biopsy and aspiration. These give detailed info on CLL’s effect on blood cell making.
Rai and Binet Staging Systems
After CLL is diagnosed, staging systems help figure out how far the disease has spread. The Rai and Binet systems are the two main ones.
- The Rai staging system has five stages (0 to IV). It looks at lymphocyte count, lymph nodes, spleen size, anemia, and low platelets.
- The Binet staging system has three stages (A, B, and C). It checks lymphoid areas, anemia, and low platelets.
Prognostic Markers and Risk Stratification
Prognostic markers are also key in CLL diagnosis. They include genetic changes, IGHV mutation status, and protein levels like CD38 and ZAP-70.
By using staging and markers together, we can better understand a patient’s risk. This helps in making treatment plans that fit each patient’s needs.
Why Chronic Lymphocytic Leukemia Remains Incurable
To understand why CLL is hard to cure, we need to look at its biology and treatment hurdles. Even with big steps forward in treatment, many patients can’t be cured.
Biological Resistance Mechanisms
One big reason CLL can’t be cured is its biological resistance to treatments. CLL cells can hide from the immune system and avoid dying, making them hard to kill with usual treatments.
The way CLL cells interact with their environment also plays a role. They can create a safe space around themselves, protecting them from treatment.
Minimal Residual Disease Persistence
Another problem is minimal residual disease (MRD) staying in the body. Even when treatment seems to work, some CLL cells can stay hidden. These cells can cause the disease to come back, making a cure hard to find.
MRD staying around shows we need better ways to find and kill these hidden cells.
Challenges in Targeting Leukemic Stem Cells
Leukemic stem cells start and keep CLL going. These cells are very hard to kill with usual treatments. They are thought to be a big reason CLL comes back.
It’s tough to target these stem cells because they can hide and are hard to find. New treatments are being tried to find and kill these cells, hoping to cure CLL.
Other Incurable Blood Cancers
Beyond CLL, there are other incurable blood cancers like CML, myelodysplastic syndromes, and some non-Hodgkin lymphomas. These diseases are tough to cure with today’s treatments.
Chronic Myeloid Leukemia: Manageable But Not Curable
Chronic Myeloid Leukemia (CML) is a blood disorder where stem cells grow too much. It’s managed with special drugs, but it can’t be cured.
- TKIs have greatly helped CML patients.
- But, some patients may not respond well to these drugs.
- Stopping these drugs often means the disease comes back.
Myelodysplastic Syndromes and Treatment Limitations
Myelodysplastic syndromes (MDS) are a group of blood disorders. They make blood cells not work right and can turn into AML.
Key challenges in treating MDS include:
- We don’t fully understand what causes MDS.
- Most treatments don’t work well.
- There’s a big chance of turning into AML.
Indolent Non-Hodgkin Lymphomas
Indolent non-Hodgkin lymphomas, like follicular lymphoma, grow slowly. But, they can’t be cured with usual treatments.
Doctors try to control symptoms and slow the disease. New treatments, like targeted and immunotherapies, are being tested to help more.
Current Treatment Approaches for CLL
CLL is a complex disease, so treatments vary. They range from watching the disease to using targeted therapies. The right treatment depends on the disease stage, the patient’s age, and genetic markers.
Watch and Wait Strategy for Early-Stage CLL
For those with early-stage CLL and no symptoms, a “watch and wait” approach is common. This means regular blood tests and check-ups to catch any disease growth.
- Regular blood counts to monitor lymphocyte levels
- Physical examinations to check for lymphadenopathy or splenomegaly
- Periodic bone marrow biopsies to assess disease infiltration
This method avoids unnecessary treatment side effects. It allows for quick action when the disease gets worse.
Chemoimmunotherapy Regimens
For those needing treatment, chemoimmunotherapy is key. It combines chemotherapy with immunotherapy, like monoclonal antibodies targeting CD20 (e.g., rituximab) or CD52.
Common chemoimmunotherapy regimens include:
- FCR (fludarabine, cyclophosphamide, and rituximab)
- BR (bendamustine and rituximab)
- Chlorambucil-based regimens with obinutuzumab or rituximab
These treatments work well but can be tough on the body. They’re chosen based on the patient’s health.
Targeted Therapies: BTK and BCL-2 Inhibitors
Targeted therapies have changed CLL treatment. BTK inhibitors (e.g., ibrutinib, acalabrutinib) and BCL-2 inhibitors (e.g., venetoclax) are leading these changes.
- BTK Inhibitors: Block Bruton’s tyrosine kinase, stopping CLL cell growth and survival.
- BCL-2 Inhibitors: Make CLL cells die by blocking the BCL-2 protein.
These therapies work well, even for those with high-risk features or who’ve had treatment before.
Managing Incurable Blood Cancer Long-Term
Managing incurable blood cancer needs a detailed plan. It’s about finding the right balance between treatment and quality of life. Understanding long-term care is key.
Treatment Goals: Disease Control vs. Cure
For incurable blood cancers, treatment goals change. We aim to control the disease, not cure it. This means managing symptoms and slowing the disease’s growth.
Disease control is now the main goal. Treatments are chosen to lessen the cancer’s impact. Each patient gets a treatment plan that fits their needs.
Balancing Efficacy and Quality of Life
Finding the right balance between treatment and quality of life is vital. We aim to reduce side effects while keeping treatments effective. This is done through careful planning and constant monitoring.
Quality of life is a top priority. We focus on managing symptoms and reducing side effects. This helps patients live better despite their illness.
Addressing Treatment Side Effects
Dealing with side effects is a big part of long-term care. We work with patients to find and fix side effects. This makes treatments more bearable and effective.
We use different strategies to manage side effects. This includes adjusting treatments, using supportive care, and teaching self-care. By tackling side effects early, we improve patient comfort and treatment success.
Prognosis and Survival Rates for Incurable Blood Cancers
Knowing the prognosis for incurable blood cancers is key for both patients and doctors. It helps predict the disease’s outcome and shapes treatment plans.
Factors Affecting CLL Prognosis
Chronic Lymphocytic Leukemia (CLL) prognosis depends on several factors. These include the disease’s stage at diagnosis, genetic mutations, and the patient’s health. We’ll dive into these to grasp their impact on CLL prognosis.
- Genetic Mutations: Some genetic changes, like del(17p) or TP53 mutations, point to a worse prognosis.
- Stage at Diagnosis: CLL’s stage at diagnosis greatly influences its prognosis. Early stages are more hopeful than advanced ones.
- Patient’s Overall Health: Comorbidities and age can affect how well a patient can handle treatments, impacting prognosis.
Life Expectancy with Modern Treatments
Modern treatments have greatly boosted CLL patients’ life expectancy. Advances in targeted therapies and chemoimmunotherapy allow many to live for years with manageable disease.
Survival Rates: Recent studies show a big jump in CLL patients’ 5-year survival rates with today’s treatments. Yet, survival varies based on the factors mentioned earlier.
Indicators of Disease Progression
It’s vital to watch for signs of disease progression for timely action and treatment adjustments. Key signs include:
- Increasing lymphadenopathy or splenomegaly
- Worsening cytopenias
- Rising CLL cell counts
- Development of new symptoms or complications
Regular checks and quick action on these signs can greatly improve CLL patients’ quality of life and survival.
Living with Chronic Lymphocytic Leukemia
Getting a CLL diagnosis can change your life. It’s important to have a strong support network and make lifestyle changes. We’ll look at the psychological impact, coping strategies, and the need for support resources.
Psychological Impact and Coping Strategies
CLL can deeply affect your mental health. You might feel anxious, depressed, or scared. To deal with these feelings, try:
- Mindfulness and Meditation: These can help reduce stress and clear your mind.
- Counseling and Therapy: Getting help from professionals can address your emotional needs.
- Support Groups: Sharing experiences with others who understand can offer comfort and support.
Using these strategies can improve your life and help you manage CLL’s challenges.
Support Resources for Patients and Families
Having a strong support system is key for CLL patients. It provides emotional and practical help. Here are some resources:
- Family and Friends: They can offer emotional support and help with daily tasks.
- Patient Support Groups: These groups let patients share their stories and get support.
- Healthcare Professionals: Doctors and nurses can guide you medically and offer support.
These resources are essential for patients and their families to cope with CLL.
Lifestyle Modifications and Self-Care
Changing your lifestyle can improve your quality of life with CLL. Important changes include:
- Dietary Changes: Eating a balanced diet supports your health.
- Regular Exercise: Staying active helps keep you strong and mobile.
- Stress Management: Activities like yoga and meditation can reduce stress.
By making these lifestyle changes and practicing self-care, CLL patients can manage their condition better and improve their well-being.
Complications and Related Health Concerns
People with CLL often deal with many complications that affect their life quality. It’s important to know about these issues to manage the disease well.
Increased Infection Susceptibility
CLL makes people more likely to get infections. This happens because CLL weakens the immune system. So, patients are more at risk for infections from bacteria, viruses, and fungi.
- Immunosuppression: CLL weakens the immune system, making it hard to fight off infections.
- Frequent Infections: Patients often get infections over and over again. These can be serious and need hospital care.
To lower this risk, doctors suggest ways to prevent infections. This includes getting vaccinated and using antibiotics as needed.
Secondary Malignancies Risk
People with CLL are also more likely to get other cancers. This is because of the disease itself and the treatments used.
- Cancer Risk: There’s a higher chance of getting other cancers, like skin cancers and certain lymphomas.
- Surveillance: It’s important to check regularly for any new cancers early on.
Richter’s Transformation and Disease Evolution
Richter’s transformation is when CLL turns into a more aggressive lymphoma. This usually happens into a type called diffuse large B-cell lymphoma.
- Clinical Presentation: This change is often seen with fast disease growth, big lymph nodes, and other symptoms.
- Treatment Challenges: Treating Richter’s transformation is hard. It often needs strong treatments.
Breakthrough Research and Clinical Trials
The world of CLL treatment is changing fast, thanks to new clinical trials and research. Scientists are finding new ways to treat CLL, which could greatly help patients.
Novel Therapeutic Approaches Under Investigation
Researchers are looking into new ways to fight CLL. They’re working on targeted therapies that only harm cancer cells, not healthy ones. This could lead to treatments that are more precise and less harsh.
Another exciting area is combination therapies. This means using more than one treatment at a time. Early trials suggest this could make treatments more effective and last longer.
CAR-T Cell Therapy and Immunotherapy Advances
CAR-T cell therapy is a type of immunotherapy that’s showing great promise. It modifies T cells to attack cancer cells. This therapy has led to complete remissions in some CLL patients.
There’s also progress in immunotherapy. Scientists are looking into ways to boost the immune system’s fight against CLL. Early trials are promising, showing these methods could help patients who haven’t responded well to other treatments.
We’re hopeful that these advances will lead to better care for CLL patients. Ongoing trials will help figure out if these new treatments are safe and work well. This could make them available for more people in the future.
Conclusion
Understanding Chronic Lymphocytic Leukemia (CLL) and other blood cancers is key for patients and doctors. We’ve looked into what these diseases are, if they can be cured, and the treatments available.
Chronic Lymphocytic Leukemia (CLL) is a type of leukemia that is currently considered incurable with existing treatments. But, new research gives hope for better management and life quality. Supporting patients with incurable blood cancers is crucial, encompassing not only medical treatment but also mental health and lifestyle support.
As we face the challenges of blood cancer, staying updated on new treatments and research is critical. This way, we can aim for a future where patients get care that meets their specific needs.
For those with CLL and other blood cancers, staying strong and having a support system is vital. With ongoing research and better treatments, there’s growing hope for patients and their families.
FAQ
What is chronic lymphocytic leukemia (CLL)?
CLL is a cancer that affects the blood and bone marrow. It causes the body to make too many immature white blood cells.
Chronic Lymphocytic Leukemia (CLL) is a type of leukemia that is currently considered incurable with existing treatments.
CLL is not curable with today’s treatments. But, different therapies can help manage the disease and improve life quality.
What are the symptoms of CLL?
Symptoms of CLL include feeling very tired, losing weight, swollen lymph nodes, and getting sick often. Some people may not show symptoms early on.
How is CLL diagnosed?
Doctors use blood tests and bone marrow exams to find CLL. These tests help see if there are cancer cells and what stage the disease is.
What are the treatment options for CLL?
CLL treatments include watching and waiting, chemoimmunotherapy, and targeted therapies like BTK and BCL-2 inhibitors. Clinical trials are also an option.
What is the watch and wait strategy for CLL?
The watch and wait strategy is for early-stage CLL. It means not treating right away. Treatment starts when symptoms appear or the disease gets worse.
How does CLL affect quality of life?
CLL and its treatments can lower quality of life. This is due to symptoms, side effects, and the emotional burden of living with a chronic illness.
What are the complications associated with CLL?
CLL complications include getting sick more easily, risk of other cancers, and a rare but serious change called Richter’s transformation.
Are there any new treatments being developed for CLL?
Yes, new treatments like CAR-T cell therapy and immunotherapy are being researched. They aim to improve CLL treatment results.
How can patients with CLL manage their condition?
Patients can manage CLL by following treatment plans, staying healthy, getting support, and learning about their disease.
What is the prognosis for patients with CLL?
CLL prognosis depends on disease stage, genetics, and treatment response. Modern treatments have made life expectancy and quality of life better.
Can CLL be differentiated from other blood cancers?
Yes, CLL can be told apart from other blood cancers through tests and looking at specific genetic markers.
References
Keating, M. J. (2012). Is Chronic Lymphocytic Leukemia Still Incurable? Blood Reviews. Retrieved from
https://www.sciencedirect.com/science/article/pii/S0006497118566088
Hallek, M. (2025). Chronic Lymphocytic Leukemia: 2025 Update on the Diagnosis, Risk Stratification and Treatment. American Journal of Hematology. Retrieved from
https://pubmed.ncbi.nlm.nih.gov/39871707




































