Last Updated on October 31, 2025 by

We aim to give you all the details about carcinoma in situ (CIS) of the bladder. It’s a serious, aggressive form of early-stage cancerRadio Waves and Cancer Treatment Explained with big risks.
CIS can turn into invasive disease if not treated. If ignored, up to 60 percent of people might get muscle-invasive disease in five years. Knowing about CIS’s biology, detection, and treatment is key to better patient care.
We want to talk about CIS, why it matters, and why we need to know how to diagnose and treat it. Our aim is to help both patients and doctors understand this complex issue better.
To manage CIS bladder cancer well, we need to know what it is, how it’s classified, and how it differs from other bladder cancers.
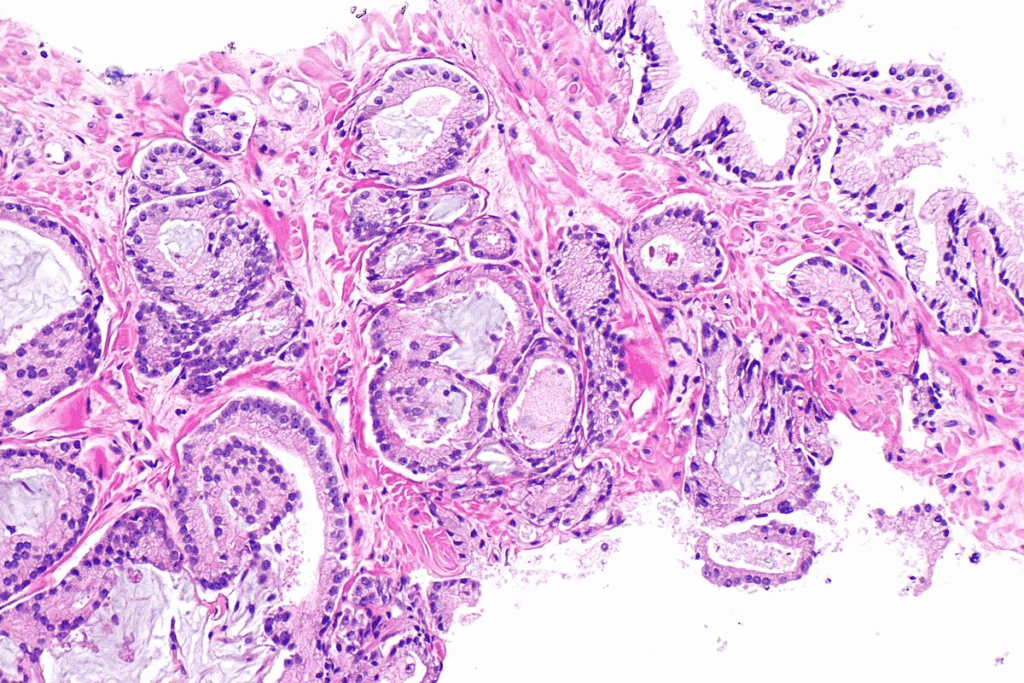
CIS bladder cancer, or carcinoma in situ, has high-grade malignant cells with severe changes. It looks flat and doesn’t form papillae like other cancers. This makes it hard to spot during regular cystoscopy.
Knowing the early stages of CIS bladder cancer is key for treatment. It’s a high-grade lesion from the start, which means it can quickly turn into invasive cancer if not treated right. Doctors look at how much of the bladder is affected and if there’s any invasive cancer too.
Here are the main differences between CIS bladder cancer and other types:
These differences are important for diagnosis and treatment. For example, CIS’s flat look means doctors need special tools like enhanced cystoscopy with fluorescence or narrow-band imaging to find it.
Key Fact #1: CIS Is a High-Grade, Flat Urothelial Lesion
Carcinoma in situ (CIS) bladder cancer is a high-grade, flat urothelial lesion. It’s different from other bladder cancers. Knowing this helps us understand CIS better.
CIS bladder cancer has high-grade malignant cells. These cells are in the urothelium but don’t invade the bladder wall. They have big nuclei and prominent nucleoli, showing they are high-grade.
Doctors look closely at these cells to diagnose CIS. They use cystoscopy, biopsy, and histology. These cells can become aggressive and lead to invasive cancer if not treated.
CIS doesn’t form papillary structures like some bladder cancers do. Its flat appearance is a key diagnostic feature. This makes CIS different from low-grade papillary urothelial carcinomas.
Because CIS is flat, it’s hard to spot with cystoscopy alone. A detailed diagnosis is needed to find CIS.
| Characteristics | CIS Bladder Cancer | Low-Grade Papillary Bladder Cancer |
| Cellular Grade | High-grade | Low-grade |
| Lesion Appearance | Flat | Papillary |
| Invasiveness | Non-invasive but potentially aggressive | Typically non-invasive |
It’s important to know the differences between CIS and other bladder cancers. The high-grade and flat nature of CIS highlights the need for quick and effective treatment. This helps prevent it from becoming invasive.
Key Fact #2: Prevalence and Demographics of CIS Bladder Cancer
Knowing who is at risk for CIS bladder cancer is key. It helps us focus our screening efforts. The facts about who gets CIS bladder cancer tell us a lot.
About 10% of bladder cancer cases start as CIS. Most people with CIS are over 60. This matches the trend for all bladder cancers.
CIS bladder cancer is much more common in men, with a 7:1 ratio. This mirrors the gender gap in all bladder cancers. Both genes and environment play a part in this.
This imbalance means we need to target our awareness and screening at older men. Catching CIS early is vital. It helps stop it from becoming worse.
Key Fact #3: Primary vs. Secondary CIS Occurrence
The difference between primary and secondary CIS is key in bladder cancer. CIS, or carcinoma in situ, can start as a primary issue or come after other bladder tumors. Knowing when and why CIS happens helps doctors plan better care and talk to patients.
Primary CIS is found when bladder cancer is first diagnosed, with no past history of it. This type is rare, making up less than 3% of bladder cancers. People with primary CIS might have a different journey than those with secondary CIS.
Sometimes, CIS is found along with other bladder tumors. This makes treatment plans more complex. The presence of CIS can change how doctors choose treatments and how often to check up on patients.
Secondary CIS is found when checking up on bladder cancer that’s already been treated. It’s more common than primary CIS. Finding secondary CIS means the cancer might come back or grow, so doctors need to watch it closely and might use stronger treatments.
To understand the differences between primary and secondary CIS, let’s look at some key points in the table below:
| Characteristics | Primary CIS | Secondary CIS |
| Frequency | Less than 3% of urothelial neoplasms | More frequent, detected during follow-up |
| Timing of Diagnosis | At initial presentation | During follow-up for other bladder cancers |
| Clinical Implications | Different clinical course | May indicate higher risk of progression or recurrence |
It’s important to know the differences between primary and secondary CIS to tailor treatments. This way, doctors can give patients care that’s more suited to their needs, leading to better results.
Key Fact #4: Anatomical Distribution Within the Bladder
The way CIS spreads in the bladder is key to fighting it. It affects how we find and treat the disease. CIS bladder cancer shows up in many parts of the bladder, making it hard to manage.
CIS bladder cancer often shows up in multiple spots in the bladder. This makes it tough to diagnose and treat. It needs a detailed look and a solid plan to manage.
Research shows that CIS in many places raises the risk of coming back and getting worse. So, knowing where CIS is helps doctors come up with better treatment plans.
CIS bladder cancer often hits the trigone, lateral wall, and dome. The trigone is a key area because of its location at the bladder’s base.
| Location | Frequency of CIS Occurrence |
| Trigone | High |
| Lateral Wall | Moderate to High |
| Dome | Moderate |
The table shows CIS often hits the trigone, then the lateral wall and dome. Knowing this helps doctors during exams.
The way CIS spreads in the bladder affects how we find and treat it. Detailed cystoscopy and biopsies are needed for accurate diagnosis and staging.
“The multifocal nature of CIS bladder cancer necessitates a meticulous approach to diagnosis and treatment, stressing the need for advanced diagnostic tools and tailored treatment plans.” – Dr. [Last Name], Urologist
Treatments like BCG must consider where CIS is. The goal is to get rid of the disease without harming the bladder.
In summary, knowing where CIS is in the bladder is key to managing it. By understanding its spread and common spots, doctors can create better plans for diagnosis, treatment, and follow-up.
Key Fact #5: Progression Risk of CIS Bladder Cancer
The risk of CIS bladder cancer turning into invasive disease is a big worry for patients and doctors. CIS bladder cancer has a high chance of getting worse, leading to muscle-invasive bladder cancer if not treated right.
Research shows that 40% to 60% of CIS bladder cancer patients will get invasive disease in 5 years. This high rate of progression highlights the need for careful watching and quick action.
The rate of progression can change based on several things. These include the presence of other bladder tumors and how well the first treatment works. Knowing these factors is key to creating a good treatment plan.
Several things can affect how likely CIS bladder cancer is to turn into invasive disease. These include:
Looking at these factors helps doctors guess the risk of progression. They can then plan treatments that fit each patient’s needs.
| Factor | Influence on Progression |
| Multifocal CIS Lesions | Increases the risk of progression |
| Concurrent High-Grade Papillary Tumors | Higher risk of progression to invasive disease |
| Failure to Respond to BCG Therapy | Indicates a higher risk of progression |
| Genetic and Molecular Characteristics | Can indicate a higher or lower risk of progression |
By knowing what affects CIS bladder cancer progression, we can improve patient care. We can make better choices about treatments.
To find CIS bladder cancer, doctors use many steps. These include checking symptoms, doing cystoscopy, and special tests. We’ll talk about how to spot CIS bladder cancer. This includes looking at symptoms, the tests used, and lab work.
CIS bladder cancer can show up with symptoms like hematuria (blood in urine), dysuria (pain when you pee), and needing to pee a lot or right away. These signs can also show up in other bladder problems. So, it’s hard to tell if it’s CIS just by symptoms.
Doctors need to look at these signs along with other tests to find CIS bladder cancer. A good check-up is key to decide what tests to do next.
Cystoscopy lets doctors see inside the bladder. They can spot CIS or other cancers by looking at the bladder’s lining. Fluorescence cystoscopy uses a special dye to make cancer cells stand out.
A biopsy is needed to confirm CIS. Doctors take samples from the bladder during cystoscopy. These are then checked under a microscope. Finding high-grade urothelial carcinoma without papillary formation means it’s CIS.
Urine cytology checks urine for cancer cells. It’s good for finding high-grade urothelial carcinomas like CIS. But, it might miss low-grade tumors.
Biomarkers for bladder cancer are getting more use. Tests like UroVysion and NMP22 find bladder cancer cells or proteins. These tests help cystoscopy and urine cytology, making diagnosis better.
| Diagnostic Method | Description | Advantages |
| Cystoscopy | Visual examination of the bladder | Direct visualization of CIS lesions |
| Biopsy | Histological examination of bladder tissue | Confirms diagnosis of CIS |
| Urine Cytology | Examination of urine for cancer cells | Non-invasive, sensitive for high-grade tumors |
| Biomarkers | Detection of specific proteins or genetic markers | Aids in diagnosis and surveillance |
Intravesical BCG therapy is key in treating CIS bladder cancer. It has changed how we manage this disease, making treatments more effective.
Intravesical BCG (Bacillus Calmette-Guérin) therapy is the main treatment for CIS bladder cancer. This immunotherapy involves directly instilling BCG into the bladder through a catheter, which helps fight cancer cells. The treatment starts with an initial phase and then maintenance to keep the cancer under control.
Studies show that BCG therapy is very effective in treating CIS bladder cancer. It greatly reduces the chances of the cancer coming back or getting worse. But, some patients might face side effects or not respond well.
When BCG therapy doesn’t work or the cancer comes back, treatment gets harder. Alternative treatments and clinical trials are looked into for these cases. Options include other intravesical therapies, systemic treatments, or new methods in clinical trials.
Finding the right next treatment depends on the patient’s health, past treatments, and the cancer’s details.
New treatments for CIS bladder cancer are being developed. Immunotherapies beyond BCG, targeted therapies, and new ways to deliver treatments are being explored. These aim to help patients who don’t respond to BCG or face other challenges.
Clinical trials are important in this area. They offer new treatments that might work better or be safer. Participating in these trials helps patients and helps us learn more about treating CIS bladder cancer.
Keeping an eye on CIS bladder cancer is key. It helps catch any signs of trouble early. This way, we can act fast.
Checking the bladder and urine is essential. We suggest cystoscopy every 3-6 months for the first two years. This is after the first treatment.
At each check-up, urine cytology is also done. It helps spot cancer cells. How often we do cystoscopy can change based on the patient’s situation.
| Follow-up Interval | Cystoscopy Frequency | Urine Cytology Frequency |
| 0-2 years | Every 3-6 months | At each visit |
| 2-5 years | Every 6-12 months | At each visit |
| After 5 years | Annually | At each visit |
Managing CIS bladder cancer long-term means more than just watching. It’s also about teaching patients about signs of trouble. Like blood in the urine or changes in how they pee.
Risk stratification is important. It helps decide how closely to watch each patient. Those at higher risk need more checks.
It’s best to have a team for CIS bladder cancer care. This team should include urologists, oncologists, and others. This way, patients get the best care possible.
It’s key to know about CIS bladder cancer early for better treatment. Carcinoma in situ bladder cancer is a serious, flat growth in the bladder lining. If not treated, it can turn into invasive cancer.
Diagnosing CIS bladder cancer involves several steps. These include cystoscopy, biopsy, and urine tests. Treatment options include BCG therapy inside the bladder. New treatments are being looked into for cases that don’t respond to BCG.
Regular checks for bladder cancer are vital. A set schedule helps catch any changes early. This is important for managing the disease.
Good treatment for bladder cancer starts with quick diagnosis and right care. We stress the need for awareness and following check-up plans. This helps improve patient results. CIS bladder cancer needs a full approach to stop it from getting worse.
Knowing about CIS bladder cancer risks helps doctors give better care. It also helps patients manage their health better. Our talk shows how important ongoing research and awareness are in treating and watching bladder cancer.
CIS (Carcinoma in Situ) bladder cancer is an early-stage cancer. It has cancerous cells on the bladder’s surface but doesn’t invade the wall.
CIS bladder cancer is unique because of its flat cells and high-grade nature. It doesn’t form papillae like other cancers. This makes it more aggressive and needs quick treatment.
CIS bladder cancer mainly hits men, with a 7:1 male to female ratio. It’s also common in older adults. This group needs more awareness and screening.
Yes, CIS bladder cancer can be either primary or secondary. Primary is diagnosed first, while secondary occurs during follow-up for other cancers. Each type has different management needs.
Diagnosis includes clinical checks, cystoscopy, biopsy, urine cytology, and biomarkers. These help spot CIS and tell it apart from other bladder issues.
CIS bladder cancer has a high risk of turning into muscle-invasive cancer. This risk is 40-60% within 5 years if not treated well.
Intravesical BCG therapy is the main treatment for CIS bladder cancer. But, there’s also research on managing BCG-resistant cases and new treatments.
Regular checks with cystoscopy and urine cytology are key. They help catch early signs of recurrence or progression. This allows for timely treatment and better outcomes.
Carcinoma in situ means cancer cells are present but haven’t invaded deeper tissues. It’s an early-stage cancer that needs quick treatment to stop it from getting worse.
CIS bladder cancer’s multifocal nature makes complete removal hard. It requires detailed surveillance to catch and treat all affected areas.
National Center for Biotechnology Information. (2025). CIS Bladder Cancer 5 Key Facts About Carcinoma. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8617135/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!