Last Updated on November 14, 2025 by Ugurkan Demir
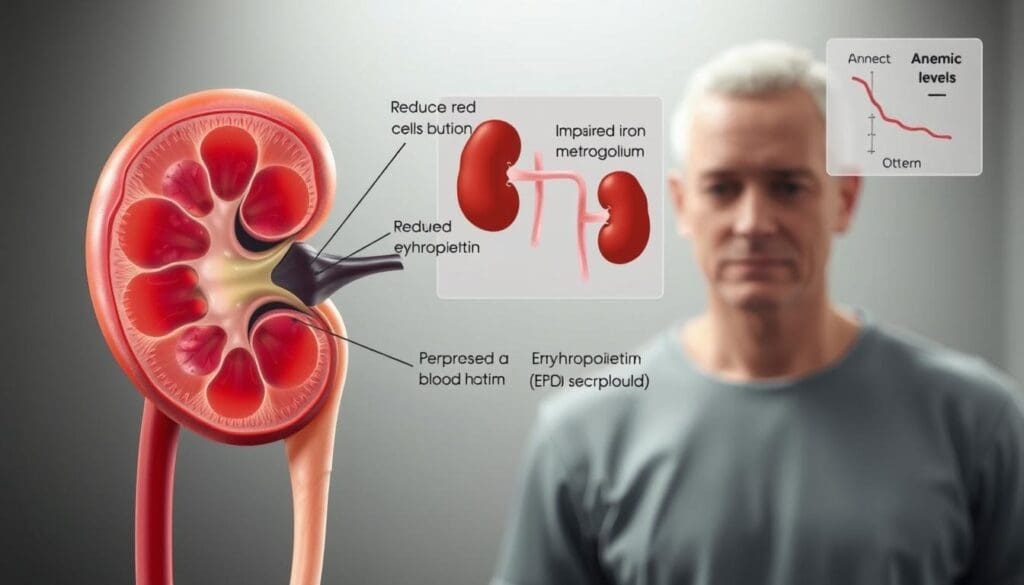
Chronic Kidney Disease (CKD) often leads to anemia, a lack of red blood cells. This happens because the kidneys can’t make enough erythropoietin. Erythropoietin is key to makingg red blood cells.
As CKD gets worse, less erythropoietin is made. This means fewer red blood cells are produced. This makes anemia worse.
The link between CKD and anemia is complex. It’s not just about less erythropoietin. Iron metabolism issues also play a part. Knowing these details helps manage anemia better in CKD patients.
Today, there are many ways to treat anemia in CKD. These treatments aim to improve life quality for those affected.
Key Takeaways
- CKD is a big reason for anemia because of less erythropoietin.
- Anemia in CKD is caused by more than just less erythropoietin. Iron issues also matter.
- Managing anemia well is important for better life quality in CKD patients.
- There are modern treatments for anemia in CKD.
- Liv Hospital provides expert care for managing anemia linked to CKD.
Understanding Chronic Kidney Disease (CKD)

It’s important to know about CKD to manage it well. CKD means your kidneys slowly lose function over time.
Definition and Stages of CKD
CKD is when your kidneys don’t filter well or are damaged. It has five stages. Stage 1 is the least severe, and Stage 5 means your kidneys have failed.
- Stage 1: Kidney damage with normal or increased GFR (>90 ml/min).
- Stage 2: Mild reduction in GFR (60-89 ml/min).
- Stage 3: Moderate reduction in GFR (30-59 ml/min), divided into 3A and 3B.
- Stage 4: Severe reduction in GFR (15-29 ml/min).
- Stage 5: Kidney failure (GFR
Prevalence and Risk Factors
CKD is common worldwide, with different rates in different places. Risk factors include diabetes, high blood pressure, family history, and being overweight.
The CDC says about 15% of U.S. adults have CKD. You can lower your risk with lifestyle changes and medical care.
Normal Kidney Function in Red Blood Cell Production
Kidneys make erythropoietin (EPO), a hormone that helps make red blood cells. Healthy kidneys keep EPO levels right, helping your body make enough red blood cells.
“The kidneys are vital for maintaining homeostasis and regulating various bodily functions, including the production of red blood cells through erythropoietin.”
In short, knowing about CKD means understanding its stages, how common it is, and its role in making red blood cells. This knowledge is key to understanding CKD-related anemia and treatment options.
The Pathophysiology of CKD and Anemia
Understanding anemia in CKD is key to better treatment and outcomes. Anemia is common in CKD patients. It comes from a mix of factors related to kidney decline.
Prevalence of Anemia in CKD Patients
Anemia is very common in CKD patients. It gets worse as kidney function declines. Almost all patients with advanced CKD have anemia.
CKD stage and anemia are closely linked. Higher stages mean more severe kidney issues and a higher chance of anemia. Monitoring hemoglobin levels is vital. Early detection of anemia can improve patient outcomes and quality of life.
Impact of Anemia on Quality of Life
Anemia greatly affects CKD patients’ quality of life. It causes fatigue, weakness, and shortness of breath. These symptoms can make it hard to function physically and reduce productivity.
“Anemia in CKD patients complicates their clinical management, necessitating a holistic approach to address both the anemia and the underlying kidney disease.”
Managing anemia well is essential. It can improvthe qualityty of life and slow CKD progression.
Correlation Between CKD Progression and Anemia Severity
Anemia severity often matches CKD progression. As kidney function worsens, anemia gets worse. This is due to reduced erythropoietin production, impaired iron metabolism, and chronic inflammation.
Understanding this link is critical for clinicians. It helps predict patient outcomes and tailor treatments. Effective anemia management can slow CKD progression and improve patient outcomes.
How Does CKD Cause Anemia?
Chronic Kidney Disease (CKD) often leads to anemia. This is due to low erythropoietin levels, poor iron use, and ongoing inflammation. Knowing how these happen helps doctors find better treatments.
Reduced Erythropoietin Production
Erythropoietin (EPO) is made mainly by the kidneys. It helps make red blood cells in the bone marrow. When kidneys are damaged, they can’t make enough EPO. This means fewer red blood cells and anemia.
Impaired Iron Metabolism
Iron is key to makingg hemoglobin, which carries oxygen. CKD can mess up how the body uses iron. This is because of chronic inflammation and other CKD-related issues.
Shortened Red Blood Cell Lifespan
Red blood cells in CKD patients don’t last as long. This is because kidney failure creates a bad environment. It damages red blood cells, causing them to die early.
Role of Inflammation in CKD-Related Anemia
Chronic inflammation is common in CKD. It plays a big part in anemia. Inflammation raises hepcidin levels, whiccontrolson. It also lowers iron for making new red blood cells. Plus, it can stop EPO production and red blood cell making.
These factors together make anemia common in CKD. To manage anemia well, we need to tackle these problems.
- Erythropoietin deficiency: Treating with erythropoiesis-stimulating agents (ESAs).
- Impaired iron metabolism: Managing with iron supplementation.
- Chronic inflammation: Addressing through anti-inflammatory strategies.
Understanding and tackling these issues helps doctors improve anemia care in CKD patients. This makes their lives better.
Erythropoietin and Kidney Disease: A Critical Relationship
Erythropoietin, a hormone made by the kidneys, is key totolonged blood cells. Kidney disease affects this hormone’s production. The kidneys help keep red blood cells healthy by making erythropoietin (EPO). This hormone tells the bone marrow to make more red blood cells.
Normal Erythropoietin Function
Erythropoietin is a hormone made by the kidneys. It’s mainly produced by the interstitial fibroblasts. When blood oxygen levels drop, EPO production increases. This tells the bone marrow to make more red blood cells.
This process ensures tissues and organs get enough oxygen. In healthy people, EPO production is controlled by oxygen levels. When oxygen is low, EPO production goes up. When oxygen levels are normal, EPO production goes down.
How Kidney Damage Affects EPO Production
In patients with Chronic Kidney Disease (CKD), the kidneys can’t make enough EPO. This is because kidney damage affects EPO production. As CKD gets worse, the kidneys make less EPO. This leads to fewer red blood cells and anemia.
The severity of anemia in CKD depends on kidney function. Studies show that as CKD gets worse, anemia gets more severe. This is because EPO production decreases with CKD progression.
Consequences of EPO Deficiency
EPO deficiency in CKD patients causes anemia. Anemia means fewer red blood cells or less hemoglobin. This reduces oxygen delivery to tissues and organs.
Symptoms include fatigue, weakness, and shortness of breath. These symptoms can lower the quality of life and increase heart disease. Treating EPO deficiency is key in managing CKD.
Clinical Manifestations of Anemia Related to Kidney Disease
Anemia linked to CKD can cause a wide range of symptoms. These symptoms can be mild, like fatigue, or severe, like heart problems. Anemia related to kidney disease affects many parts of a patient’s health.
Common Symptoms and Signs
People with CKD-related anemia often feel fatigue, weakness, and shortness of breath. These symptoms can make everyday tasks hard and lower their quality of life. Other signs include pale skin, dizziness, and cold intolerance.
Impact on Cardiovascular Health
Anemia can severely affect the heart in CKD patients. It can cause increased cardiac workload, left ventricular hypertrophy, and decreased oxygen delivery to tissues. This can lead to heart failure, angina, and other heart problems.
Cognitive and Neurological Effects
CKD-related anemia can also harm brain and nerve function. Patients might have cognitive impairment, memory loss, and decreased concentration. Anemia is also linked to increased risk of neurological disorders and decreased mental performance.
Diagnosing Anemia in CKD Patients
Diagnosing anemia in patients with chronic kidney disease (CKD) is a detailed process. It involves lab tests and a clinical check-up. Anemia is common in CKD patients, and finding it early is key to managing the disease well.
Laboratory Tests and Evaluation
Labs are essential in finding anemia in CKD patients. The first step is to check the patient’s hemoglobin through a complete blood count (CBC). Other tests include:
- Iron studies to check for iron deficiency
- Reticulocyte count to see how the bone marrow is doing
- Erythropoietin level to see if the kidneys are making enough
- Vitamin B12 and folate levels to check for deficiencies
Differentiating CKD-Related Anemia from Other Types
CKD-related anemia is mainly due to low erythropoietin from kidney damage. But other anemia,s like iron deficien,cy can also happen in CKD patients. It’s important to tell them apart for the right treatment.
When figuring out if it’s CKD-related anemia, consider:
- The patient’s CKD stage and erythropoietin levels
- Presence of iron deficiency or other nutritional deficiencies
- Chronic inflammation, which can affect iron metabolism
When to Suspect Anemia in CKD Patients
Anemia might be suspected in CKD patients with symptoms like fatigue, weakness, pale skin, or shortness of breath. It’s important to regularly check hemoglobin levels, more so in advanced CKD stages.
Doctors should watch for anemia signs and start tests quickly. This ensures timely treatment.
Chronic Kidney Disease Anemia Treatment: Iron Management
Managing iron deficiency is key in treating anemia in CKD patients. Iron supplements are vital to help make red blood cells, whiare importantant for those taking erythropoiesis-stimulating agents (ESAs).
Assessing Iron Status
It’s important to check iron levels before starting treatment. This means looking at serum ferritin and transferrin saturation (TSAT). The CKD Non-Dialysis Anemia Management Protocol says levels below 100 ng/mL for ferritin and 20% for TSAT show iron deficiency.
Oral vs. Intravenous Iron Supplementation
Choosing between oral and IV iron depends on how severe the deficiency is, how well the patient can tolerate it, and if there’s inflammation. Oral iron is usually the first choice, but IV iron is better for severe cases or when oral iron doesn’t work well.
- Oral iron is easy to take and affordable,b utit can upset the stomach.
- IV iron, like ferric carboxymaltose, raises iron levels faster and is easier for some to take.
Monitoring Response to Iron Therapy
It’s important to keep an eye on iron levels, hemoglobin, and how the patient feels. This helps see if the iron therapy is working. If not, the treatment might need to be changed.
Clinical Guidelines for Iron Supplementation
Guidelines suggest making a treatment plan that fits each patient. This includes how severe the anemia is, the patient’s iron levels, and any other health issues. The goal is to keep iron levels right while avoiding side effects.
- Start iron supplements when ferritin is under 100 ng/mL or TSAT is under 20%.
- Decide between oral and IV iron based on how well the patient can handle it and how bad the deficiency is.
- Check iron levels and hemoglobin often to adjust treatment as needed.
Good iron management is key in treating anemia in CKD patients. It helps improve their health and quality of life.
Erythropoiesis-Stimulating Agents (ESAs) in Kidney Failure Anemia
ESAs are key in treating anemia in kidney failure. They help make red blood cells by mimicking a hormone the kidneys make. This hormone is vital for blood cell production.
Types of ESAs Available
There are several ESAs used in medicine, including:
- Epoetin alfa
- Darbepoetin alfa
- Methoxy polyethylene glycol-epoetin beta
Each ESA has a different use and dosing. Doctors choose based on the patient’s needs and guidelines.
Dosing Strategies and Administration
Getting the right dose of ESAs is very important. The dose starts with the patient’s weight and hemoglobin level. It then changes based on how well the patient responds and their iron levels.
Key considerations for ESA dosing include:
- Starting dose based on the patient’s weight and hemoglobin level
- Regular monitoring of hemoglobin and adjustment of dose as necessary
- Adequate iron supplementation to support erythropoiesis
Benefits and Potential Risks
ESAs have many benefits. They reduce the need for blood transfusions and improve the quality of life. They may also lower the risk of heart problems. But, there are risks too, like:
- Increased risk of blood clots
- Potential for pure red cell aplasia
- Risk of high blood pressure
Choosing the right patients and monitoring them closely is key to avoiding these risks.
Target Hemoglobin Levels and Monitoring
The goal of ESA therapy is to keep hemoglobin levels right. This improves symptoms and quality of life without increasing risks. Guidelines suggest aiming for hemoglobin levels between 10 g/dL and 11 g/dL.
Regular monitoring of hemoglobin, iron, and blood pressure is vital. It ensures ESA therapy is both effective and safe.
Additional Therapeutic Approaches for Anemia Secondary to CKD
Managing anemia in CKD patients goes beyond iron supplements and ESAs. We need to tackle the complex nature of anemia in CKD. This helps improve patients’ quality of life and health.
Addressing Nutritional Deficiencies
Nutritional gaps are key in anemia for CKD patients. It’s vital to get enough vitamin B12, folate, and iron. Dietary advice can guide patients to eat well. Sometimes, supplements are needed to fill nutritional gaps.
Managing Inflammation
Inflammation is common in CKD and affects anemia. Managing inflammation is essential. This can be done with meds and lifestyle changes. Checking C-reactive protein (CRP) levels helps gauge inflammation.
Blood Transfusions: Indications and Considerations
Blood transfusions are sometimes needed for severe anemia in CKD patients. They offer quick relief but come with risks like iron overload and immune sensitization. Transfusions should be carefully considered, weighing the benefits against the risks.
Patient Self-Management Strategies
Teaching patients to manage their anemia is critical. This includes sticking to treatment plans, making dietary changes, and watching for symptoms. Patient education and support are essential for success.
By using these strategies, healthcare providers can offer a more detailed and tailored treatment plan. This approach can significantly improve outcomes for patients with anemia due to CKD.
Emerging Therapies and Research in Renal Anemia
New treatments are changing how we manage anemia in patients with CKD. This brings hope for better lives. Research is creating new ways to tackle the root causes of renal anemia. This could lead to better ways to manage it.
HIF Stabilizers: Mechanism and Clinical Trials
HIF stabilizers are a new type of oral medicine. They mimic how our bodies handle low oxygen levels. This helps make more red blood cells.
Studies show they work well. They help increase hemoglobin levels. This means less need for iron shots and ESAs.
Novel Iron Formulations
New iron products aim to be safer and more effective. They are made to have fewer side effects than old iron treatments. Research is ongoing to see how well they work.
Future Directions in Research
Future studies will likely focus on personalized medicine. This means treatments will be based on each patient’s needs. New tests and genetic studies could help make treatments more precise.
Personalized Medicine Approaches
Using personalized medicine in treating renal anemia is very promising. It could lead to better treatments and fewer side effects. This could change how we treat anemia in CKD, making it more focused on the patient.
Conclusion: Optimizing Management of Anemia in Chronic Kidney Disease
Managing anemia in CKD needs a detailed plan. This plan should include iron supplements, ESAs, and fixing the root causes. It’s all about tackling the problem from different angles.
CKD and anemia go hand in hand. Anemia is a big issue for people with CKD. Knowing how anemia happens in CKD helps doctors create better treatment plans.
For anemia in CKD, a patient-focused approach is key. Doctors should keep a close eye on hemoglobin, iron levels, and how well ESAs work. This way, treatments can be made just right for each patient.
By taking a full and coordinated approach to anemia in CKD, doctors can make patients’ lives better. They can lower heart risks and slow down the disease’s progress.
FAQ
What is the relationship between chronic kidney disease (CKD) and anemia?
CKD can cause anemia because it reduces the production of erythropoietin. This hormone is key to making red blood cells.
How does CKD cause anemia?
CKD leads to anemia in several ways. It lowers erythropoietin, affects iron use, shortens red blood cell life, and causes inflammation.
What are the symptoms of anemia related to kidney disease?
Symptoms include feeling tired, weak, and short of breath. It can also cause heart problems, affecting your longevity.
How is anemia diagnosed in CKD patients?
Doctors use blood tests to check for anemia. These tests help find out how severe it is and what treatment is needed.
What is the role of erythropoietin in managing anemia in CKD?
Erythropoietin helps make red blood cells. Without enough, anemia occurs. Treatments like ESAs mimic its effects to help.
How is iron deficiency managed in CKD-related anemia?
Doctors check iron levels and give supplements. This can be through pills or injections, depending on the need.
What are the benefits and risks of using ESAs in kidney failure anemia?
ESAs can raise hemoglobin levels and reduce the need for blood transfusions. But, they can also increase blood pressure and heart risks.
What are emerging therapies for managing renal anemia?
New treatments include HIF stabilizers and better iron formulas. They aim to improve anemia care and patient results.
How does CKD progression correlate with anemia severity?
Anemia gets worse as CKD advances. Early detection and treatment are key to managing both conditions.
What is the impact of anemia on cardiovascular health in CKD patients?
Anemia can worsen heart disease. It increases heart work, leading to heart failure and other heart issues.
Can anemia related to kidney disease be treated?
Yes, anemia can be treated. This includes iron supplements, ESAs, and addressing nutritional and inflammation issues.
What is the importance of monitoring hemoglobin levels in CKD patients?
Checking hemoglobin levels is vital. It helps catch anemia early and guides treatment to avoid complications and improve life quality.
References
- Portolés, J. (2021). Anemia in Chronic Kidney Disease: From Pathophysiology to Treatment. Frontiers in Medicine, 8, 642296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8032930/