At Liv Hospital, we know how important it is to manage heart rhythm problems well. Sodium channel blockers, or Class 1 antiarrhythmic drugs, are key in treating these issues.
Understand class 1 antiarrhythmic drugs and sodium channel blocker effects.
These medicines block sodium channels in the heart. This helps control irregular heartbeats. We divide them into three types: IA, IB, and IC, each used differently.
Knowing how these drugs work helps us use them better. This knowledge lets us treat patients more effectively. It also helps us understand any side effects, ensuring the best care for our patients.
Key Takeaways
- Class 1 antiarrhythmic drugs are sodium channel blockers used to manage cardiac arrhythmias.
- They are categorized into three subclasses: IA, IB, and IC.
- Understanding their mechanism of action is key for effective treatment.
- These medicines are vital in treating various heart rhythm disorders.
- Liv Hospital provides evidence-based, patient-centered care using the latest protocols.
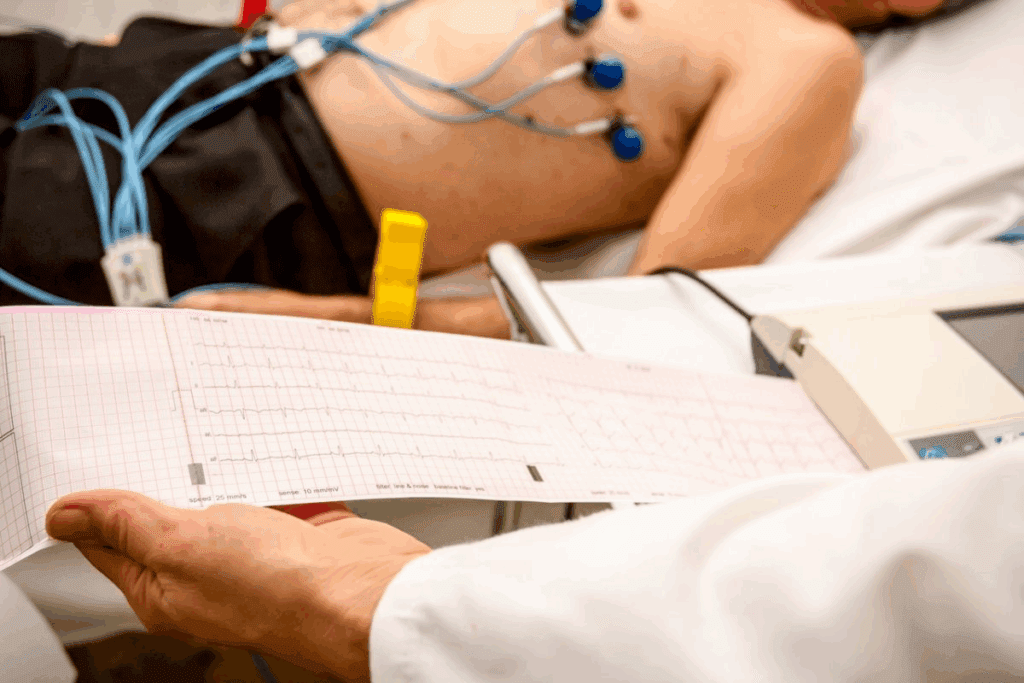
The Fundamentals of Cardiac Electrical Activity
To understand Class 1 antiarrhythmic drugs, we must first grasp the basics of heart electrical activity. The heart’s ability to pump blood efficiently depends on a complex electrical system.
Normal Cardiac Conduction System
The heart’s electrical system works in a coordinated way to contract. It starts with the sinoatrial (SA) node, the heart’s natural pacemaker. This node generates the electrical impulses.
The impulse then goes to the atrioventricular (AV) node, where it’s delayed a bit. Then, it moves to the ventricles through the bundle of His, bundle branches, and Purkinje fibers. This ensures the heart’s chambers contract together.
Pathophysiology of Cardiac Arrhythmias
Cardiac arrhythmias happen when the heart’s electrical system is disrupted. This can be due to problems with electrical impulse generation or propagation.
Arrhythmias can stem from several causes, like enhanced automaticity, triggered activity, or reentrant circuits. Knowing these causes helps us see how Class 1 antiarrhythmic drugs help restore normal heart rhythm.
| Component | Function |
| Sinoatrial (SA) Node | Acts as the heart’s natural pacemaker, generating electrical impulses. |
| Atrioventricular (AV) Node | Delays the electrical impulse before it reaches the ventricles. |
| Bundle of His and Bundle Branches | Conducts the impulse to the ventricles. |
| Purkinje Fibers | Distributes the impulse throughout the ventricles, ensuring synchronized contraction. |
“The complexity of cardiac electrical activity highlights the need for targeted treatments.”
Class 1 Antiarrhythmic Drugs: Definition and Overview
Class 1 antiarrhythmic drugs block sodium channels. They are key in treating heart rhythm problems. These drugs change how the heart’s electrical activity works.
The Vaughan Williams Classification System sorts these drugs. It helps us see how Class 1 drugs work.
The Vaughan Williams Classification System
The Vaughan Williams Classification System groups drugs into four classes. Class 1 drugs block sodium channels. This action reduces sodium ion flow during the heart’s electrical cycle.
“The Vaughan Williams Classification has been a cornerstone in understanding antiarrhythmic drug therapy, providing a simple yet effective way to categorize these complex medications.”
Medical Expert
| Class | Mechanism of Action | Examples of Drugs |
| Class I | Sodium Channel Blockade | Quinidine, Lidocaine, Flecainide |
| Class II | Beta-Blockade | Propranolol, Metoprolol |
| Class III | Potassium Channel Blockade | Amiodarone, Sotalol |
| Class IV | Calcium Channel Blockade | Verapamil, Diltiazem |
Common Properties of Sodium Channel Blockers
Sodium channel blockers have some common traits. They slow heart conduction and can lengthen the action period.
Key properties of sodium channel blockers:
- Modulation of sodium channel activity
- Effects on cardiac conduction velocity
- Influence on action period duration
- Variability in subclassification based on specific effects
Knowing about Class 1 antiarrhythmic drugs helps doctors treat heart rhythm issues better. This leads to better patient care.
Key Fact #1: Mechanism of Action of Sodium Channel Blockers
It’s important to know how sodium channel blockers work. They help manage heart rhythm problems. We’ll look at how these drugs affect the heart’s electrical activity.
Fast Voltage-Gated Sodium Channels in Cardiac Tissue
Fast voltage-gated sodium channels start and spread action potentials in heart cells. They cause the heart to contract quickly. Sodium channel blockers work by blocking these channels.
Preferential Binding to Open or Inactivated States
Sodium channel blockers bind better to open or inactivated channels. This is key to their action. It helps them reduce sodium flow, slowing down the heart and stopping arrhythmias.
Effects on Action Potentials and Conduction
Blocking sodium channels changes how long action potentials last and how fast they move. This slows down the heart’s electrical signals. It’s how these drugs help control arrhythmias.
| Effect | Description | Clinical Implication |
| Reduced Sodium Influx | Decreased rate of depolarization | Slowed conduction velocity |
| Prolonged Refractory Period | Increased time before the next action can occur | Reduced likelihood of reentrant arrhythmias |
| Altered Action Potentials Duration | Changes in the length of the action potentials | Variable effects on arrhythmia suppression |
Understanding how sodium channel blockers work helps us see their role in heart rhythm management. It shows their impact on the heart’s electrical activity.
Key Fact #2: Subclassification of Class 1 Antiarrhythmic Drugs
Class 1 antiarrhythmic drugs are divided into subclasses. This division helps doctors pick the right drug for each arrhythmia. It makes treatments work better and reduces side effects.
Class IA: Moderate Sodium Channel Blockade
Class IA drugs block sodium channels moderately. They also affect potassium channels, which makes the action time longer. Key characteristics include:
- Moderate sodium channel blockade
- Prolongation of action duration
- Examples include quinidine, procainamide, and disopyramide
Class IB: Weak Sodium Channel Blockade
Class IB drugs have a weak effect on sodium channels, mainly in healthy heart tissue. They work better in sick or ischemic heart. Notable features are:
- Weak sodium channel blockade
- Shortening of action duration
- Lidocaine and mexiletine are examples of Class IB drugs
Class IC: Strong Sodium Channel Blockade
Class IC drugs block sodium channels strongly. They slow down how signals move without changing the action time much. Important aspects include:
- Strong sodium channel blockade
- Significant slowing of conduction velocity
- Flecainide and propafenone are prominent Class IC agents
Knowing these subclasses is key to choosing the right antiarrhythmic treatment. The differences in how they block sodium channels and affect the heart help doctors manage arrhythmias well.
Key Fact #3: Class IA Antiarrhythmic Agents in Detail
Class IA antiarrhythmic drugs, like quinidine, procainamide, and disopyramide, are key in treating heart rhythm issues. They block sodium channels moderately. This helps manage different arrhythmias.
Quinidine: Mechanisms and Clinical Applications
Quinidine, from the cinchona tree bark, is an old antiarrhythmic drug. It blocks sodium channels, slowing down heart signals and making the heart pause longer. It’s used for arrhythmias like atrial fibrillation and ventricular tachycardia.
Key properties of quinidine include:
- Moderate sodium channel blockade
- Prolongation of the QT interval
- Anticholinergic effects
Procainamide: Properties and Uses
Procainamide is a Class IA drug used for quick treatment of arrhythmias. It works like quinidine but is less likely to cause stomach problems.
Procainamide’s clinical applications include:
- Treatment of ventricular arrhythmias
- Conversion of atrial fibrillation to sinus rhythm
- Maintenance therapy for recurrent arrhythmias
Disopyramide: Characteristics and Indications
Disopyramide is good for treating ventricular arrhythmias and keeping the heart in rhythm. But, it can weaken the heart, which is a problem for those with heart failure.
“Disopyramide’s unique property of having a negative inotropic effect makes it less ideal for patients with certain cardiac conditions.”
Important considerations for disopyramide include:
- Careful dosing in patients with renal impairment
- Monitoring for anticholinergic side effects
- Potential for proarrhythmic effects
Key Fact #4: Class IB Antiarrhythmic Medications
Ventricular arrhythmias are serious and can be managed with Class IB antiarrhythmic medications. These include lidocaine and mexiletine. They are great for treating ventricular arrhythmias because of how they work.
Class IB antiarrhythmic medications block sodium channels weakly. This makes them less good for atrial arrhythmias but perfect for ventricular ones. Lidocaine is a well-known Class IB drug used for years.
Lidocaine: Pharmacology and Clinical Uses
Lidocaine is given intravenously, making it great for emergencies. It starts working fast and doesn’t last long, which is good in urgent situations. It blocks sodium channels in the heart, mainly in the ventricles, to stop arrhythmias.
Lidocaine is mainly used for ventricular tachycardia and fibrillation. It’s also used after heart attacks to prevent dangerous arrhythmias. But, it needs to be watched closely because it’s not very forgiving.
Mexiletine: Oral Alternative to Lidocaine
Mexiletine is an oral Class IB drug like lidocaine. It’s for long-term treatment of ventricular arrhythmias. It’s good for patients who need ongoing treatment but can’t stay on intravenous lidocaine.
Mexiletine is taken by mouth, which means it can be used for longer. It’s great for patients with long-term arrhythmias. But, it can cause side effects like stomach problems and neurological issues.
Effectiveness for Ventricular Arrhythmias
Lidocaine and mexiletine are both good at treating ventricular arrhythmias. They stop abnormal heart activity, which is why they’re important in cardiology. The choice between them depends on the situation, with lidocaine for emergencies and mexiletine for long-term use.
In summary, Class IB antiarrhythmic medications like lidocaine and mexiletine are key for managing ventricular arrhythmias. Their unique properties make them perfect for this job, and they’ve been proven through lots of research and use.
Key Fact #5: Class IC Antiarrhythmic Agents
Flecainide and propafenone are Class IC antiarrhythmic drugs. They block sodium channels well. These drugs help manage arrhythmias, like supraventricular tachycardias and some ventricular arrhythmias.
Flecainide: Potent Sodium Channel Blockade
Flecainide is a strong Class IC antiarrhythmic drug. It blocks sodium channels a lot. This slows down heart tissue without changing action potentials much.
Key properties of flecainide include:
- High potency sodium channel blockade
- Minimal effect on action duration
- Significant slowing of conduction velocity
- Effective for supraventricular and ventricular arrhythmias
Propafenone: Dual Sodium Channel and Beta-Blocking Effects
Propafenone is a Class IC antiarrhythmic drug. It blocks sodium channels and has beta-blocking effects. This makes it good for many arrhythmias, from supraventricular tachycardias to ventricular arrhythmias.
Notable features of propafenone include:
- Dual sodium channel and beta-blocking effects
- Broad efficacy across various arrhythmia types
- Useful for both supraventricular and ventricular arrhythmias
CAST Trial and Safety Considerations
The Cardiac Arrhythmia Suppression Trial (CAST) looked at Class IC drugs like flecainide and encainide. It was stopped early because of more deaths in the treated group. This raised big safety concerns for these drugs in some patients.
“The CAST trial highlighted the proarrhythmic risk of Class IC drugs, mainly in those with heart disease. This has led to more careful use and focus on choosing the right patients and monitoring them.” –
AHA Journal
The CAST trial’s findings have changed how we use Class IC drugs. Even though flecainide and propafenone are useful, we use them more carefully. We also watch patients closely to avoid risks.
| Drug | Primary Mechanism | Common Indications | Safety Considerations |
| Flecainide | Potent sodium channel blockade | Supraventricular tachycardias, ventricular arrhythmias | Proarrhythmic risk, mainly in heart disease |
| Propafenone | Sodium channel blockade with beta-blocking effects | Supraventricular tachycardias, certain ventricular arrhythmias | Proarrhythmic risk, bronchospasm (due to beta-blocking effects) |
Clinical Applications of Class 1 Antiarrhythmic Drugs
Class 1 antiarrhythmic drugs are used to treat many heart rhythm problems. They work by blocking sodium channels and changing how the heart’s electrical signals work. This helps manage different types of arrhythmias.
Treatment of Supraventricular Arrhythmias
These drugs are great for treating heart rhythm issues like atrial fibrillation and atrial flutter. Flecainide and propafenone are top choices for keeping the heart’s rhythm regular.
They slow down electrical signals in the heart’s upper chambers. This helps control supraventricular arrhythmias.
Management of Ventricular Arrhythmias
Class 1 drugs are also used for ventricular arrhythmias, like ventricular tachycardia and fibrillation. Lidocaine is a key drug for treating these issues quickly.
| Drug | Class | Primary Use |
| Lidocaine | 1B | Ventricular Arrhythmias |
| Flecainide | 1C | Supraventricular Arrhythmias |
| Propafenone | 1C | Supraventricular Arrhythmias |
Prevention of Reentrant Circuits
Class 1 drugs work by stopping reentrant circuits from forming. They do this by slowing down electrical signals and changing how long the heart’s cells can’t conduct signals.
Class 1C agents like flecainide are very good at this. They slow down electrical signals a lot.
Side Effects and Safety Profile
It’s important to know the side effects of Class 1 antiarrhythmic drugs. These drugs help manage arrhythmias but can have side effects. Doctors need to think about these effects carefully.
Common Adverse Effects
Class 1 antiarrhythmic drugs can cause different side effects. Some common ones are:
- Gastrointestinal disturbances
- Central nervous system effects such as dizziness and confusion
- Cardiac effects, including changes in heart rhythm
Not all patients experience side effects, and the severity can vary widely.
Proarrhythmic Potentia
One big risk with Class 1 antiarrhythmic drugs is their proarrhythmic effect. This means they can make arrhythmias worse or even cause new ones.
The risk is higher with Class IC agents, as shown by the CAST trial.
Cardiac and Non-Cardiac Toxicity
Class 1 antiarrhythmic drugs can cause both cardiac and non-cardiac toxicity. Cardiac toxicity can make heart failure worse or cause conduction problems. Non-cardiac toxicity can affect the liver, lungs, and other organs.
Drug Interactions and Special Considerations
Using Class 1 antiarrhythmic drugs needs careful thought about drug interactions and special cases. These medicines can mix with other drugs in ways that affect their safety and how well they work. It’s also important to consider their use in different groups of people to ensure they are safe and effective.
Important Drug-Drug Interactions
Class 1 antiarrhythmic drugs can interact with many other medicines. For example, Class IA agents like quinidine can raise the levels of digoxin, which might cause toxicity. On the other hand, Class IC agents such as flecainide can make beta-blockers work too much, which is not good.
To understand these interactions better, here’s a summary of key drug interactions for Class 1 antiarrhythmic drugs:
| Class 1 Antiarrhythmic Drug | Interacting Drug | Potential Effect |
| Quinidine (Class IA) | Digoxin | Increased digoxin levels, potentially leading to toxicity |
| Flecainide (Class IC) | Beta-blockers | Enhanced negative inotropic effect |
| Lidocaine (Class IB) | Cimetidine | Increased lidocaine levels due to reduced clearance |
Use in Special Populations
Using Class 1 antiarrhythmic drugs in special groups, like the elderly or pregnant women, needs extra care. For instance, dosage adjustments may be necessary for those with kidney problems, as these drugs are often cleared by the kidneys.
When using these drugs in pregnant or breastfeeding women, we must weigh the risks and benefits. For example, lidocaine is usually safe during pregnancy, but it should only be used when really needed.
In summary, knowing about drug interactions and special considerations is key for safely and effectively using Class 1 antiarrhythmic drugs. Healthcare providers can reduce risks and improve outcomes by understanding these factors.
Recent Advances and Future Directions
Breakthroughs in sodium channel research are changing how we treat heart rhythm problems. As scientists learn more about these channels, new treatments are being developed.
New Research on Sodium Channel Structure and Function
Our understanding of sodium channels has grown a lot. Recent studies have shown how these channels work and how drugs interact with them.
Key findings include:
- The identification of specific binding sites for Class 1 antiarrhythmic drugs on the sodium channel.
- Insights into the conformational changes that occur in sodium channels during the cardiac action potent.
- The role of sodium channel mutations in certain arrhythmogenic conditions.
Novel Compounds Under Investigation
New antiarrhythmic drugs are being developed. Several promising agents are being investigated to improve current treatments.
Some of the novel compounds under investigation include:
- Ranolazine, which has shown efficacy in treating certain arrhythmias by inhibiting late sodium current.
- GS-458967, a potent and selective inhibitor of the sodium channel.
- New formulations of existing drugs, designed to improve pharmacokinetics and reduce side effects.
Targeted Approaches to Arrhythmia Management
Our understanding of arrhythmias is growing. Targeted therapies aim to treat the specific cause of an arrhythmia, making treatments better and safer.
Examples of targeted approaches include:
- Genotype-guided therapy for certain arrhythmogenic syndromes.
- The use of advanced imaging techniques to guide ablation procedures.
- Personalized medicine approaches based on an individual’s genetic profile and drug metabolism.
These advances and future directions in Class 1 antiarrhythmic drugs are promising. As research keeps evolving, we’ll see better and safer treatments for heart rhythm problems.
Conclusion: The Evolving Role of Class 1 Antiarrhythmics in Modern Cardiology
We’ve looked into Class 1 antiarrhythmic drugs, key in managing heart rhythm issues. As research grows, these drugs’ role keeps changing, shaping cardiology’s future.
Class 1 antiarrhythmics are essential for treating many heart rhythm problems. Studies on sodium channels are leading to new drugs and better treatments.
The mix of old and new treatments will change how we treat heart issues. Knowing how these drugs work and their limits is key to better care.
In short, Class 1 antiarrhythmics will keep being important in cardiology. Their changing role shows how heart rhythm management is always evolving. Keeping up with new research helps us give patients the best care.
FAQ
What are Class 1 antiarrhythmic drugs?
Class 1 antiarrhythmic drugs are a type of medicine. They block sodium channels in the heart. This affects the heart’s electrical activity.
How do Class 1 antiarrhythmic drugs work?
These drugs interact with sodium channels in the heart. They change how the heart’s electrical activity works.
What is the Vaughan Williams Classification System?
The Vaughan Williams Classification System sorts antiarrhythmic drugs. It groups them by how they work, with Class 1 being sodium channel blockers.
What are the subclasses of Class 1 antiarrhythmic drugs?
Class 1 antiarrhythmic drugs are divided into subclasses. These are Class IA, IB, and IC. They differ in how they block sodium channels and affect the heart’s electrical activity.
What are some examples of Class IA antiarrhythmic agents?
Class IA antiarrhythmic agents include quinidine, procainamide, and disopyramide. They are used to treat heart rhythm problems.
What are the clinical applications of Class 1 antiarrhythmic drugs?
Class 1 antiarrhythmic drugs treat various heart rhythm issues. They also help prevent certain heart problems.
What are the possible side effects of Class 1 antiarrhythmic drugs?
Side effects of Class 1 antiarrhythmic drugs include heart and non-heart problems. They can also cause other issues.
How do Class 1 antiarrhythmic drugs interact with other medications?
Class 1 antiarrhythmic drugs can interact with other medicines. It’s important to consider these interactions when using them.
Are Class 1 antiarrhythmic drugs safe for use in special populations?
Using Class 1 antiarrhythmic drugs in special groups needs careful thought. Their safety and effectiveness must be considered.
What are some recent advances in the field of Class 1 antiarrhythmic drugs?
New research on sodium channels is advancing Class 1 antiarrhythmic drugs. New compounds and targeted treatments are also being explored.
What is the future of Class 1 antiarrhythmic drugs in modern cardiology?
The future of Class 1 antiarrhythmic drugs is promising. Ongoing research and development are leading to new treatments and strategies.
References:
National Center for Biotechnology Information. (2025). Class 1 Antiarrhythmic Drugs 5 Key Facts About. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482322/))