For women facing infertility, knowing how Clomid works is key. Clomid, or clomiphene citrate, is a common drug that boosts ovulation. It does this by increasing the production of follicle-stimulating hormone (FSH). This hormone helps egg follicles grow, raising the chances of getting pregnant.
At Liv Hospital, we aim to give top-notch healthcare. We focus on ethical care and new ways to help with fertility. Our team is here to support women on their fertility journey, with personalized care and treatments like Clomid.
Key Takeaways
- Clomid is a first-line treatment for ovulation disorders, helping approximately 70% of anovulatory women achieve ovulation.
- Clomid works by stimulating the secretion of follicle-stimulating hormone (FSH) to promote egg follicle growth.
- Women under 35 have shown pregnancy rates of 20-25% monthly when treated with Clomid.
- Clomid is effective in treating anovulation and oligo-ovulation in women struggling with infertility.
- Our healthcare providers at Liv Hospital offer complete support and tailored fertility treatments.
Understanding Clomid: A Fertility Medication Overview
Clomid, also known as clomiphene citrate, is a key fertility treatment. It helps women conceive by solving ovulation problems.
What is Clomiphene Citrate?
Clomiphene citrate is a non-steroidal fertility drug. It’s a selective estrogen receptor modulator (SERM). It works by blocking estrogen in the brain, making it think there’s less estrogen. This makes the brain release hormones that help ovulation happen.
History and Development
Clomid has been used for fertility for decades. It was first made to treat breast cancer. But, it was found to help with ovulation during trials. Now, it’s a key part of treating infertility.
Classification as a Selective Estrogen Receptor Modulator
Clomid is a SERM, meaning it affects estrogen receptors. In fertility, it blocks estrogen in the brain, helping ovulation start. You need a doctor’s prescription for Clomid. It’s easy to take, making it a popular choice for many women.
How Clomid Works in the Female Reproductive System
Clomid works by affecting hormones in a complex way. It’s a drug that helps women with ovulation problems. It’s been used for many years to treat infertility.
The Science Behind Estrogen Receptor Blocking
Clomid binds to estrogen receptors in the hypothalamus. This blocks estrogen’s negative feedback on the hypothalamus and pituitary gland. This estrogen receptor blocking makes the hypothalamus think estrogen levels are low.
This leads to more Gonadotropin-Releasing Hormone (GnRH) production. GnRH then prompts the pituitary gland to release more follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Hormonal Cascade: GnRH, FSH, and LH
GnRH’s release starts a chain of hormonal events. It makes the pituitary gland release FSH and LH. FSH helps ovarian follicles grow and mature, which contain eggs.
As follicles grow, they make estrogen. This estrogen causes a surge in LH. This LH surge is key for ovulation, as it makes the egg release from the dominant follicle.
Follicle Development and Egg Release
FSH makes many follicles grow. But usually, only one follicle becomes the dominant one. This dominant follicle releases an egg during ovulation.
The LH surge makes the dominant follicle release the egg. This happens 5 to 10 days after taking Clomid. The egg then moves through the fallopian tube, where it can be fertilized by sperm.
In summary, Clomid works by boosting GnRH, FSH, and LH production. This hormonal cascade helps follicles grow and leads to egg release. It increases the chances of getting pregnant.
Who Can Benefit from Clomid Treatment
Clomid is often given to women with irregular ovulation or no ovulation at all. It’s a fertility drug that helps stimulate ovulation. This is for women who have trouble getting pregnant because of ovulation problems.
Diagnosing Anovulation and Oligo-ovulation
To see if Clomid is right, you need to find out what’s causing your fertility issue. Anovulation means no ovulation, and oligo-ovulation means ovulation that’s not regular or happens too rarely. Both can make it hard to get pregnant.
Doctors use your medical history, a physical check-up, and tests like basal body temperature charts, ovulation predictor kits, or ultrasounds to diagnose these issues.
Other Fertility Conditions Treated with Clomid
Clomid is also used for other fertility problems, as decided by your doctor. This includes polycystic ovary syndrome (PCOS), luteal phase defect, and unexplained infertility.
It’s very important to work closely with your healthcare provider to find out why you’re having fertility issues. Then, you can create a treatment plan together.
When Clomid Is Not Recommended
Even though Clomid works well for many, there are times when it’s not advised. This includes if you’re allergic to clomiphene citrate, have liver disease, or abnormal bleeding. It’s also not good for women with ovarian cysts or uncontrolled thyroid or adrenal problems.
Clomid is also not for women who have had many pregnancies or are at risk for having twins or more. This is because it can increase the chance of having twins or higher-order multiples.
Knowing who can use Clomid and when it’s not a good idea helps women make better choices about their fertility care.
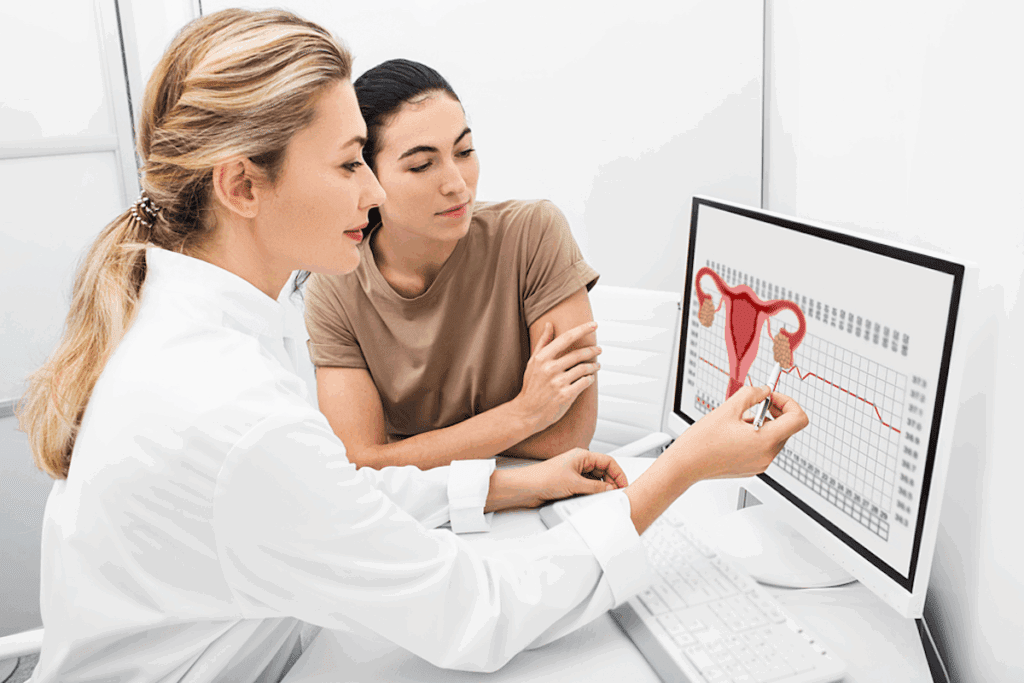
Preparing for Your First Clomid Cycle
Getting ready for your first Clomid cycle means several key steps. This includes medical checks and hormone tests. Your doctor will look at your fertility health to find the best treatment for you.
Required Medical Evaluations
Before starting Clomid, you’ll go through some medical checks. These tests find any health issues that might affect treatment success. These evaluations include looking at your medical history, a physical check-up, and tests to check your reproductive health.
Your doctor will look at your medical history. They’ll check for anything that might change how you react to Clomid. This includes past fertility treatments, health conditions, and any medicines you’re taking.
Baseline Hormone Testing
Testing your hormones before Clomid is very important. This testing shows your hormone levels and finds any problems that could affect your fertility. Tests might check for follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and more.
These tests are done on specific days of your cycle. They give your doctor the info they need to adjust your Clomid treatment just for you.
Partner Evaluation
Your partner’s fertility will also be checked. This might include a semen analysis to look at sperm quality. Good sperm quality is key for fertilization, and any problems found can be fixed before starting Clomid.
By checking both partners’ fertility, your doctor can create a detailed treatment plan. This plan aims to increase your chances of success with Clomid.
Being well-prepared is essential for a successful Clomid treatment. Knowing what steps and evaluations are needed helps you feel more ready for your journey to conceive.
The Standard Clomid Treatment Protocol
Understanding Clomid treatment is key for women trying to get pregnant. Clomid, or clomiphene citrate, helps women who don’t ovulate often. It’s designed to make ovulation regular and boost chances of getting pregnant.
Typical Dosage Guidelines
The usual Clomid dose is 50 mg a day for 5 days. It starts on the third, fourth, or fifth day of your period. But, the dose might change based on how you react to it. Some women might need up to 100 mg or more if the first dose doesn’t work.
Key considerations for dosage include:
- Initial dosage: 50 mg/day for 5 days
- Adjustment based on response: up to 100 mg/day or more
- Monitoring for ovulation and side effects
Timing Within the Menstrual Cycle
When you take Clomid is very important. It starts after your period, on days 3-5. This timing helps grow follicles in your ovaries, where eggs are.
The benefits of proper timing include:
- Enhanced follicular growth
- Increased chances of ovulation
- Better synchronization with the natural menstrual cycle
Administration Methods: Oral vs. Injectable
Clomid is usually taken by mouth. This method is easy and works well. There’s no injectable Clomid. The pill form makes it easy to change doses and is usually safe.
| Administration Method | Characteristics |
|---|---|
| Oral | Easy to administer, adjustable dosage |
| Injectable | Not available for Clomid |
Duration of Treatment
How long you take Clomid can vary. It’s usually for 3-6 cycles. If you don’t get pregnant after 3-6 cycles, you might need other treatments. Deciding to keep or stop treatment depends on how you react and any side effects.
Factors influencing treatment duration include:
- Response to treatment
- Presence of side effects
- Underlying fertility issues
Clomid and Late Ovulation: What to Expect
Women taking Clomid need to know about normal and late ovulation. Clomid helps women who don’t ovulate regularly. The timing of ovulation can change with Clomid.
Normal Ovulation Timeline with Clomid
Ovulation usually happens 5 to 10 days after the last Clomid dose. This time can change based on how well the body responds to Clomid and the length of the menstrual cycle. Knowing this helps plan for conception.
Causes of Delayed Ovulation During Treatment
Many things can cause late ovulation with Clomid. These include hormonal imbalances, the Clomid dose, and how each person reacts to the drug. Health issues like PCOS can also play a role.
The table below lists common reasons for delayed ovulation:
| Cause | Description |
|---|---|
| Hormonal Imbalance | Disruptions in the normal balance of hormones necessary for ovulation. |
| Clomid Dosage | The amount of Clomid prescribed can influence ovulation timing. |
| Underlying Health Conditions | Conditions like PCOS can affect how Clomid works. |
Managing and Addressing Late Ovulation
Managing late ovulation means watching ovulation closely and adjusting treatment as needed. This might mean changing the Clomid dose or adding other drugs. Ultrasound and ovulation predictor kits help track ovulation.
When Late Ovulation Becomes Problematic
Late ovulation can be a problem if it delays conception a lot or shows a health issue. If ovulation doesn’t come on time with Clomid, it might be time to try other fertility treatments.
Understanding how Clomid affects ovulation timing helps women manage their fertility better. This knowledge aids in making informed decisions about their care.
Tracking Ovulation During Clomid Cycles
To get pregnant with Clomid, it’s key to track ovulation well. We suggest using a few ways to track ovulation accurately during Clomid cycles.
Basal Body Temperature Charting
Basal body temperature (BBT) charting is a classic way to track ovulation. It means taking your temperature every morning before getting up. A small rise in BBT shows ovulation has started. This method works best when combined with other tracking methods.
Ovulation Predictor Kits
Ovulation predictor kits (OPKs) are also useful for tracking ovulation. They find the LH surge in urine, which happens 24-48 hours before ovulation. OPKs give a more exact ovulation prediction than BBT charting alone. OPKs help pinpoint the best time for sex.
Ultrasound Monitoring
Ultrasound monitoring is a more detailed way to track ovulation. It uses regular scans to watch follicle growth and when it ruptures, showing ovulation. This method gives exact ovulation timing and is often paired with Clomid treatment. Ultrasound helps your doctor tweak your treatment plan.
Timing Intercourse for Optimal Results
Timing sex right is key when trying to conceive, even with Clomid. We advise having sex every other day in the fertile window. This window starts 5-7 days before ovulation and ends on ovulation day. Using BBT charting, OPKs, and ultrasound together boosts your chances of getting pregnant with Clomid.
By learning and using these tracking methods, you can improve your chances of getting pregnant with Clomid.
Success Rates and Expectations
When thinking about Clomid for fertility, it’s key to look at success rates and what they mean for you. Clomid, or clomiphene citrate, helps women who don’t ovulate often. It’s a common treatment for this issue.
Statistical Outcomes for Different Patient Groups
About 70% of women with anovulation start ovulating with Clomid. But, pregnancy rates are lower, from 40% to 50% after six cycles. Success rates change based on age, infertility cause, and health.
| Patient Group | Ovulation Rate | Pregnancy Rate |
|---|---|---|
| Women with PCOS | 75% | 45% |
| Women with Hypothalamic Amenorrhea | 60% | 30% |
| Women with Other Causes of Anovulation | 65% | 40% |
Timeframe for Results
Results with Clomid can take different times. Ovulation usually happens 7-10 days after the last Clomid dose. If ovulation doesn’t happen first time, doctors might change the dosage or treatment plan.
“The chance of getting pregnant with Clomid is best in the first three cycles. If not pregnant after three to six cycles, more tests and treatments might be needed.”American Society for Reproductive Medicine
Multiple Pregnancy Risk
Clomid treatment can lead to multiple pregnancies. The chance of twins is about 7%, and higher-order multiples are less than 1%. Doctors can adjust the treatment to lower this risk.
Factors Affecting Success
Many things can affect how well Clomid works. These include the reason for infertility, age, and reproductive health. For example, younger women with no other fertility problems tend to have better success rates than older women or those with more fertility issues.
- Age: Women under 35 tend to have higher success rates.
- Cause of Infertility: Clomid is more effective for women with anovulation or oligo-ovulation.
- Overall Reproductive Health: Presence of other fertility issues can affect success rates.
Knowing these factors and talking to a healthcare provider can help set realistic hopes and guide treatment.
Managing Side Effects of Clomid
It’s important for women on fertility treatment to know about Clomid’s side effects. While most women find Clomid easy to take, some may face side effects. These can range from mild to severe.
Common Side Effects
Some common side effects of Clomid include hot flashes, mood swings, and breast tenderness. These symptoms are usually mild and go away once treatment ends.
- Hot Flashes: Sudden feelings of heat, often accompanied by sweating and flushing.
- Mood Swings: Emotional changes that can range from irritability to feelings of sadness.
- Breast Tenderness: Hormonal changes can cause breast discomfort.
Mood Changes and Emotional Impact
Mood changes are a common side effect of Clomid, affecting some women more than others. These changes can be challenging, but there are strategies to manage them.
To mitigate mood swings, we recommend:
- Keeping a mood diary to track emotional changes.
- Engaging in stress-reducing activities like yoga or meditation.
- Seeking support from friends, family, or a professional counselor.
Rare but Serious Complications
While rare, Clomid can cause serious complications such as Ovarian Hyperstimulation Syndrome (OHSS). OHSS can be life-threatening and requires immediate medical attention.
Symptoms of OHSS include:
- Severe abdominal pain.
- Nausea and vomiting.
- Rapid weight gain.
- Difficulty breathing.
When to Contact Your Doctor
It’s essential to know when to seek medical help. If you experience any of the following, contact your doctor immediately:
- Severe pelvic pain.
- Vision disturbances.
- Shortness of breath.
- Signs of OHSS.
By being aware of the possible side effects and knowing when to seek help, you can manage your treatment more effectively and minimize risks.
Combining Clomid with Other Fertility Treatments
Using Clomid with other fertility treatments is a smart way to tackle fertility issues. It lets doctors create treatment plans that fit each patient’s needs. This approach boosts the chances of getting pregnant.
Clomid with Intrauterine Insemination (IUI)
Clomid and IUI together are a common and effective treatment for infertility. Clomid helps start ovulation. IUI places sperm directly in the uterus, making fertilization more likely.
Benefits of Clomid with IUI:
- Increased chances of conception due to precise sperm placement
- Enhanced effectiveness of Clomid through targeted insemination
- Less invasive compared to other fertility treatments like IVF
Clomid in IVF Protocols
In some IVF plans, Clomid is used to get more eggs. These eggs are then fertilized outside the body. This is great for women with ovulation problems.
| Treatment Aspect | Clomid Alone | Clomid in IVF |
|---|---|---|
| Ovulation Stimulation | Stimulates ovulation | Stimulates multiple egg production |
| Fertilization Method | Natural or IUI | IVF (external fertilization) |
| Success Rate | Variable, depending on individual | Generally higher due to controlled environment |
Injectable Medications with Clomid
For some, adding injectable fertility meds to Clomid boosts egg production. This is for women who don’t get enough eggs from Clomid alone.
Key Considerations:
- Monitoring is key to avoid too much stimulation
- Dosage is adjusted based on how the body responds
- Using both can increase the risk of having twins or more
Supplemental Hormones and Triggers
Supplemental hormones and triggers are sometimes added to Clomid. They help support the luteal phase or trigger ovulation at the best time. This can improve the chances of getting pregnant.
Knowing how Clomid can be used with other treatments helps both patients and doctors. Together, they can create better plans for each person’s fertility needs.
Conclusion: Making Informed Decisions About Clomid Treatment
Clomid is a well-known fertility drug that helps with ovulation issues. It’s important to know its benefits, risks, and how to use it correctly. This knowledge helps in making smart choices about treatment.
Understanding how Clomid works and who it helps is key. It’s also important to know how to handle any side effects. Clomid can help with ovulation and, when used with other treatments, can increase the chances of getting pregnant.
Patients should talk to their doctor about Clomid treatment. This way, they can watch how the medication works and make changes if needed. This approach helps in achieving success while avoiding risks.
FAQ
What is Clomid and how does it work to induce ovulation?
Clomid, also known as clomiphene citrate, is a special medicine. It helps women ovulate by affecting their hormones. It works by binding to estrogen receptors, which then triggers the release of important hormones.
This leads to the growth of follicles and the release of eggs.
What conditions is Clomid used to treat?
Clomid is mainly used for women who don’t ovulate or ovulate too little. It’s also for those with polycystic ovary syndrome (PCOS) and other ovulation issues.
How is Clomid administered, and what is the typical dosage?
Clomid is taken by mouth. The usual dose is 50mg to 100mg a day for 5 days. This starts on the third, fourth, or fifth day of your period. Your doctor might adjust the dose based on your health.
What are the common side effects of Clomid, and how can they be managed?
Side effects of Clomid include hot flashes, mood swings, and sore breasts. Rare but serious problems like ovarian hyperstimulation syndrome (OHSS) can also happen. If you have severe or lasting side effects, call your doctor.
How is ovulation tracked during Clomid cycles, and why is it important?
You can track ovulation with basal body temperature, ovulation predictor kits, and ultrasounds. It’s key to time sex right to increase your chances of getting pregnant.
What is the success rate of Clomid treatment, and what factors affect its effectiveness?
About 70% of women with anovulation ovulate with Clomid. For those with ovulation issues, 80% ovulate in the first three months. Your age, health, and fertility can influence how well Clomid works.
Can Clomid be used in combination with other fertility treatments?
Yes, Clomid is often paired with treatments like intrauterine insemination (IUI) and in vitro fertilization (IVF). It can also be used with injectables and hormones to boost treatment success.
What are the risks associated with Clomid treatment, and how can they be minimized?
Clomid can increase the risk of having twins or more. To lower this risk, follow your doctor’s advice on dosage and treatment length. Regular check-ups and monitoring are also important.
How does Clomid induce ovulation, and what is the normal ovulation timeline with Clomid?
Clomid works by releasing hormones that help follicles grow and eggs release. Ovulation usually happens 7-10 days after the last Clomid dose. But, this can vary from person to person.
What should I expect during my first Clomid cycle, and what preparations are necessary?
Before starting Clomid, you’ll have medical checks, hormone tests, and a check on your partner. Knowing what to expect and understanding the treatment can help you prepare and increase your chances of success.
References
National Center for Biotechnology Information. Clomid Use: Ovulation and Fertility Stimulation in Women. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20435548/







