Pregnancy changes a woman’s body in many ways. For some, these changes can lead to serious blood clotting issues. At Liv Hospital, we focus on managing these disorders with care. We use advanced medical skills and put our patients first.
During pregnancy, the risk of blood clots goes up fivefold. This is because of changes in the body and less blood flow in the legs. These issues can cause problems like intrauterine growth restriction and stroke. They can harm both the mother and the baby.
We know how important it is to handle clotting disorders during pregnancy. We’re here to give you the best care to reduce these risks.
Key Takeaways
- Pregnancy increases the risk of blood clots fivefold.
- Clotting disorders during pregnancy can lead to serious complications.
- Liv Hospital provides advanced medical care for clotting disorders.
- Our approach combines medical expertise with patient-centered care.
- Effective management of clotting disorders is key for both mother and baby.
Understanding Blood Clotting During Pregnancy
Blood clotting during pregnancy is a complex issue. It’s influenced by various physiological changes. As pregnancy progresses, the body prepares for childbirth by changing blood clotting mechanisms.
Physiological Changes That Increase Clotting Risk
During pregnancy, the body’s blood volume and clotting factors increase. This can lead to a higher risk of blood clots. The risk is also higher because of decreased blood flow in the legs due to the expanding uterus. These changes help prevent bleeding during childbirth but also raise the risk of blood clots.
The U.S. Surgeon General has issued a Call to Action on DVT and PE. This aims to raise public awareness and increase research on these blood conditions. It shows how important it is to understand the risks of blood clotting during pregnancy.
The Fivefold Increase in Blood Clot Risk
Pregnancy increases the risk of clotting fivefold due to these physiological changes. The risk is even higher after childbirth, and more so after a cesarean section. It’s vital for pregnant women to know these risks and the signs of blood clots to get medical help quickly.
| Physiological Change | Effect on Blood Clotting |
| Increased blood volume | Increased risk of blood clot formation |
| Increase in clotting factors | Enhanced clotting tendency |
| Decreased blood flow in legs | Increased risk of deep vein thrombosis |
Common Clotting Disorder Pregnancy Conditions
Women are at higher risk of clotting disorders during pregnancy. These can harm both the mother and the baby. We will look at common clotting disorders, their symptoms, risks, and how to manage them.
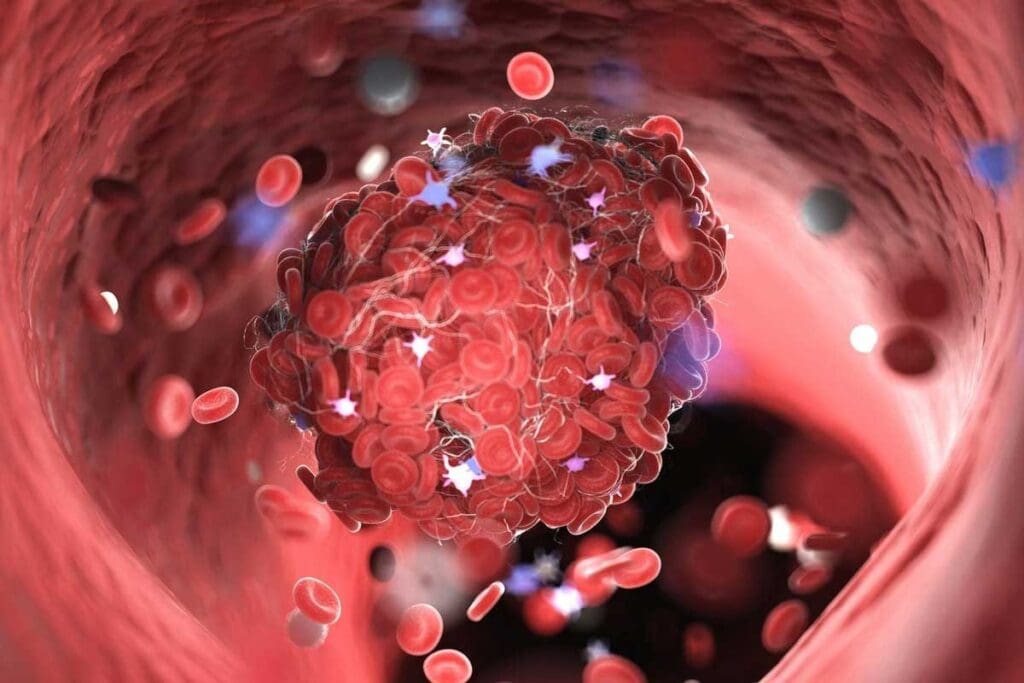
Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) is when a blood clot forms in the deep veins, usually in the legs. Pregnancy raises the risk of DVT because of increased blood volume and vein pressure. Symptoms include leg pain, swelling, and redness.
Management of DVT includes using anticoagulants to stop the clot from growing and to lower the risk of pulmonary embolism.
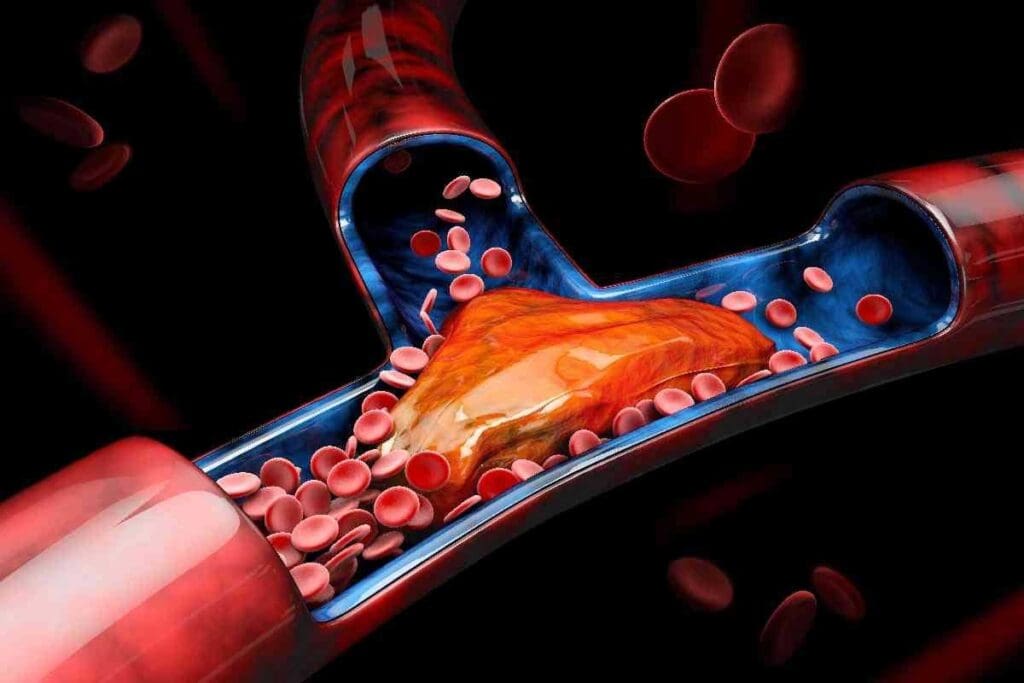
Pulmonary Embolism
Pulmonary Embolism (PE) happens when a blood clot travels to the lungs and blocks blood flow. It’s a serious condition that needs quick medical help. Symptoms include trouble breathing, chest pain, and a fast heart rate.
Treatment of PE includes anticoagulation and, in severe cases, thrombolytic therapy.
Thrombophilia
Thrombophilia is a condition that makes blood clotting more likely. It can be inherited or acquired. Inherited types include factor V Leiden and antithrombin deficiency.
Managing thrombophilia during pregnancy means careful monitoring and, in some cases, using anticoagulants to prevent clots.
| Condition | Symptoms | Management |
| DVT | Leg pain, swelling, redness | Anticoagulant therapy |
| PE | Difficulty breathing, chest pain, rapid heart rate | Anticoagulation, thrombolytic therapy |
| Thrombophilia | Varies, often asymptomatic | Monitoring, anticoagulant prophylaxis |

It’s important to understand these clotting disorders to manage risks during pregnancy. Early detection and proper management can greatly improve outcomes for both mother and baby.
Risk Factors for Developing Blood Clots During Pregnancy
Blood clots during pregnancy can be caused by genetics, medical conditions, and lifestyle. Knowing these risks helps in early detection and management.
Genetic and Family History Factors
Women with a family history of clotting disorders are at higher risk. Inherited thrombophilias can greatly increase this risk. It’s important for pregnant women to tell their healthcare providers about any family history of blood clots or clotting disorders.
Previous Blood Clot History
Having had a blood clot before increases the risk of another one during pregnancy. Blood becomes more coagulable, making it more likely for clots to form. Close monitoring and preventive measures may be necessary for these women.
Lifestyle and Medical Risk Factors
Several factors can raise the risk of blood clots during pregnancy. These include:
- Obesity
- Smoking
- Age over 35 years
- Cesarean delivery
- Prolonged bed rest or immobility
Changing these risk factors, when possible, can help lower the chance of blood clots.
Autoimmune Conditions Like Antiphospholipid Syndrome
Autoimmune conditions, such as antiphospholipid syndrome (APS), greatly increase the risk of blood clots during pregnancy. APS is marked by antiphospholipid antibodies, which can cause clotting and pregnancy complications.
“Women with APS are at an increased risk of recurrent miscarriage, preeclampsia, and thrombosis,”
Understanding and addressing these risk factors helps healthcare providers offer targeted interventions. This can reduce the risk of blood clots and related complications during pregnancy.
Potential Complications of Blood Clotting Disorders in Pregnancy
Blood clotting conditions in pregnancy can lead to serious health issues for both mom and baby. We will look at these problems and what they mean.
Maternal Health Risks
Blood clotting disorders in pregnancy can cause big health problems for the mom. One major risk is deep vein thrombosis (DVT), which can turn into a deadly pulmonary embolism (PE). Women with these disorders also face a higher chance of preeclampsia and other pregnancy issues.
Women with a history of blood clotting or diagnosed with thrombophilia need extra care. We suggest they get close monitoring during their pregnancy to lower these risks.
Fetal Health Risks
Blood clots in the placenta can block blood flow and harm the baby. This can cause placental insufficiency, leading to poor oxygen and nutrient delivery to the fetus. In bad cases, it might cause miscarriage or preterm birth.
Also, blood clotting disorders can raise the risk of growth restriction and preterm birth. It’s key to have regular prenatal visits to check on the baby’s health and fix any problems fast.
Knowing the risks of blood clotting disorders in pregnancy helps us manage them better. This way, we can improve health outcomes for both mom and baby.
Diagnosis and Management of Clotting Disorders During Pregnancy
Diagnosing and managing clotting disorders in pregnancy is complex. Early detection and proper treatment are key to avoid risks to both mother and baby.
Early Detection Methods and When to Seek Medical Help
Spotting clotting disorders early is essential. Signs like leg pain, swelling, or redness might mean DVT. Shortness of breath could signal PE. Women with clotting history or past events should watch closely.
Prenatal visits are a chance for doctors to check for clotting risks. It’s important for women to share any unusual symptoms right away.
Anticoagulant Therapy Options
Anticoagulant therapy is key for managing clotting disorders in pregnancy. Low-molecular-weight heparin (LMWH) is often chosen because it’s safe and works well. It doesn’t pass through the placenta, so it’s safe for the baby.
Other anticoagulants might be used in some cases, but they need careful thought. It’s important to watch how well the treatment is working and to avoid bleeding.
Regular Monitoring Protocols and Follow-up Care
Women on anticoagulants need regular checks. Blood tests help see if the treatment is working and if there are any bleeding risks.
Follow-up care also means watching for signs of blood clots and adjusting treatment as needed. A team of doctors, including obstetricians and hematologists, can offer the best care.
Recent Advances in Treatment Approaches
New anticoagulants with better safety profiles have been developed. Research on direct oral anticoagulants (DOACs) in pregnancy is ongoing. But, their use is limited because of safety concerns.
Understanding genetic factors in clotting disorders is also growing. This could lead to more tailored treatments in the future.
Conclusion: Advances in Managing Pregnancy Clotting Disorders
Recent breakthroughs have greatly improved how we handle blood clotting issues in pregnancy. Early detection and regular checks are key. So is the right anticoagulant therapy for each patient.
At Liv Hospital, we aim to give top-notch care. We support international patients with detailed guidance. Our team creates custom care plans for each patient, aiming for the best results.
Knowing the risks of blood clotting disorders in pregnancy is vital. With new medical care, we can lower risks. This helps keep both mom and baby healthy.
FAQ
What are the main causes of blood clots during pregnancy?
Blood clots in pregnancy happen due to changes in the body. These changes include more blood and pressure on veins from the growing uterus. There’s also a rise in clotting factors and a drop in natural anticoagulants.
How does pregnancy affect the risk of developing blood clots?
Pregnancy makes blood clotting five times more likely. This is because of changes like more blood, increased vein pressure, and changes in clotting factors.
What are the common clotting disorders that occur during pregnancy?
Deep Vein Thrombosis (DVT), Pulmonary Embolism (PE), and thrombophilia are common during pregnancy. These can be deadly if not treated quickly.
What are the risk factors for developing blood clots during pregnancy?
Risk factors include family history, previous clots, obesity, smoking, and certain medical conditions. Knowing these helps us spot high-risk patients.
How are clotting disorders during pregnancy diagnosed?
We use clinical checks, imaging tests like ultrasound, and lab tests to diagnose. Early detection is key for effective treatment.
What are the possible complications of blood clotting disorders during pregnancy?
Complications can harm both mom and baby. They include high risk of death for the mom, issues with baby growth, and early labor. Quick treatment is vital to avoid these risks.
How are clotting disorders during pregnancy managed?
We use anticoagulant therapy, regular checks, and follow-up care. We also look into new treatments to help our patients.
Can blood clotting disorders during pregnancy be prevented?
While not all cases can be stopped, knowing risks and taking steps like anticoagulants can help lower clotting chances.
What is the role of anticoagulant therapy in managing clotting disorders during pregnancy?
Anticoagulant therapy is key in treating clotting disorders. It helps stop new clots and prevents existing ones from growing.
How does Liv Hospital approach the management of clotting disorders in pregnancy?
At Liv Hospital, we use detailed protocols for managing clotting disorders. This includes early detection, anticoagulant therapy, and regular monitoring. We aim for the best outcomes for our patients.
References
- National Health Service. (2025). Deep vein thrombosis in pregnancy.