
It’s important to know about coagulation bleeding disorders and hemostasis disease. This is key for quick diagnosis and good care, mainly for kids. These issues make it hard for the body to stop bleeding or form blood clots, which can harm health.Learn coagulation bleeding disorders signs, causes, and medical insights.
Liv Hospital is dedicated to using the latest methods and focusing on the patient. They offer full support for those dealing with these complex problems. The main inherited bleeding disorders are hemophilia A, hemophilia B, and von Willebrand disease.
It’s vital to know the causes, signs, and tests for these conditions. This knowledge helps manage and treat them properly.
Key Takeaways
- Coagulation bleeding disorders affect the body’s ability to stop bleeding or form blood clots.
- Hemophilia A, hemophilia B, and von Willebrand disease are the most common inherited bleeding disorders.
- Understanding these conditions is key for quick diagnosis and effective care.
- Liv Hospital offers full support with advanced methods and patient-focused care.
- Diagnostic testing is vital for managing and treating bleeding disorders well.
Understanding Normal Hemostasis and Blood Clotting

Normal hemostasis is a complex process that stops bleeding when a blood vessel is injured. It balances procoagulant and anticoagulant factors. This ensures bleeding stops without forming too many clots.
The Three Phases of Normal Blood Clotting
The blood clotting process has three phases: primary hemostasis, coagulation, and fibrinolysis. Primary hemostasis is the immediate response to injury. Platelets stick to the injury site, forming a plug.
The coagulation phase makes this plug stable by forming a fibrin clot. This happens through a series of reactions involving clotting factors. “The coagulation cascade is a complex series of reactions that ultimately lead to the formation of a stable fibrin clot.”
Fibrinolysis, the final phase, dissolves the clot. This restores normal blood flow. It’s vital for keeping blood vessels open and preventing too much clotting.
Key Clotting Factors and Their Functions
Clotting factors are proteins in blood that are key to coagulation. There are 13 clotting factors, each with a unique role. For example, Factor VIII and Factor IX are important for the intrinsic pathway. Factor VII is vital for the extrinsic pathway.
- Factor I (Fibrinogen): Converts to fibrin to form the clot.
- Factor II (Prothrombin): Converts to thrombin, which then converts fibrinogen to fibrin.
- Factor VIII and IX: Essential for the intrinsic pathway.
The Role of Platelets in Hemostasis
Platelets are key in starting hemostasis. When a blood vessel is injured, platelets stick to the injury site. They become activated and clump together to form a plug. This plug temporarily stops blood loss.
“Platelet activation and aggregation are critical for forming a hemostatic plug, which is then stabilized by the fibrin clot.”
Platelets have many roles in hemostasis, including sticking, activating, and clumping. Understanding platelet function is key to understanding both normal hemostasis and bleeding disorders.
Coagulation Bleeding Disorders: Definition and Classification
Coagulation bleeding disorders are medical conditions that disrupt normal blood clotting. This leads to excessive bleeding. These disorders can greatly affect a person’s quality of life. It’s important to understand their causes and types.
Inherited vs. Acquired Disorders
Bleeding disorders are divided into two main types: inherited and acquired. Inherited bleeding disorders are passed down through generations. Hemophilia A and B are examples. Acquired bleeding disorders develop later in life. They can be caused by vitamin K deficiency, liver disease, or anticoagulant medications.
- Inherited Disorders: Hemophilia A, Hemophilia B, von Willebrand Disease
- Acquired Disorders: Vitamin K deficiency, Liver disease, Anticoagulant therapy
How Bleeding Disorders Affect Normal Hemostasis
Bleeding disorders disrupt the body’s ability to stop bleeding. In these disorders, blood clotting is impaired. This leads to prolonged or spontaneous bleeding. It’s important to understand how these disorders affect blood clotting to develop effective treatments.
Overview of Clotting Factor Deficiencies
Clotting factor deficiencies are common in bleeding disorders. Hemophilia A is caused by a lack of factor VIII. Hemophilia B is caused by a lack of factor IX. Other factors, like von Willebrand factor, can also be deficient or dysfunctional, leading to various bleeding disorders.
| Condition | Deficient Clotting Factor |
| Hemophilia A | Factor VIII |
| Hemophilia B | Factor IX |
| von Willebrand Disease | von Willebrand Factor |
Von Willebrand Disease: The Most Common Inherited Bleeding Disorder
Von Willebrand disease is caused by a lack or problem with Von Willebrand factor. It’s the most common inherited bleeding disorder. This condition makes it hard for blood to clot, leading to bleeding issues. Knowing about it is key for diagnosis and treatment.
Types and Subtypes of Von Willebrand Disease
Von Willebrand disease has different types and subtypes based on how much or how well Von Willebrand factor works. The main types are Type 1, Type 2, and Type 3. Type 2 is split into subtypes.
Type 1 is the mildest, with only a little less Von Willebrand factor. Type 2 has a quality problem, and Type 3 is the worst, with almost no Von Willebrand factor.
| Type | Description | Severity |
| Type 1 | Partial deficiency of Von Willebrand factor | Mild |
| Type 2 | Qualitative defect in Von Willebrand factor | Moderate |
| Type 3 | Significant deficiency or near-absence of Von Willebrand factor | Severe |
Clinical Presentation and Symptoms
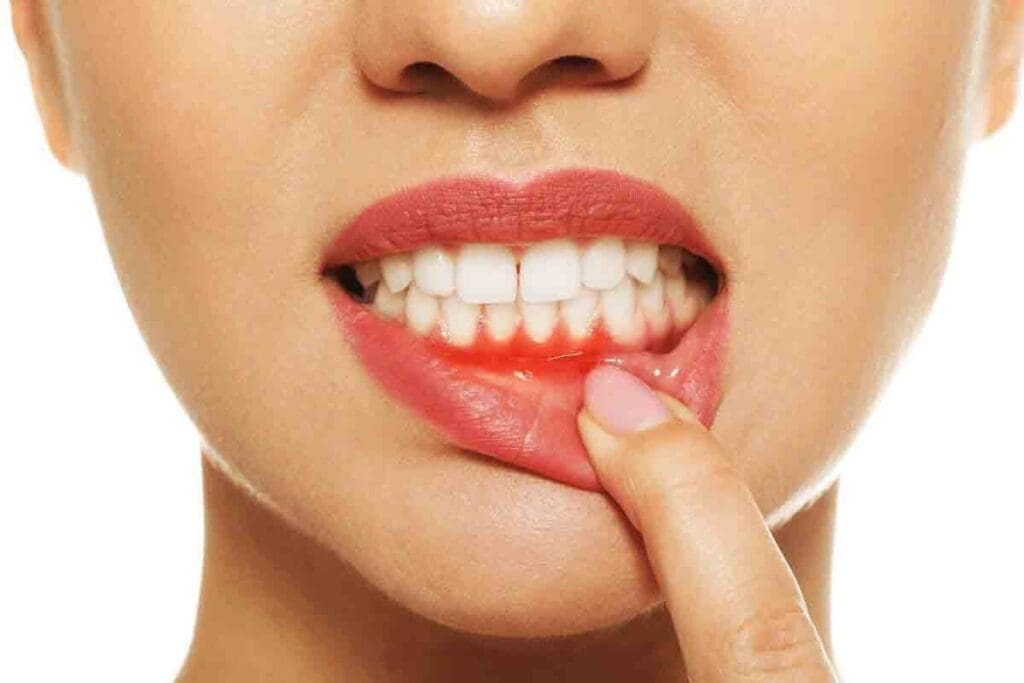
Symptoms of Von Willebrand disease vary by type and severity. Common signs include easy bruising, nosebleeds, and heavy periods. Some people bleed a lot after surgeries or dental work.
Doctors say symptoms can be mild or severe, affecting life quality. Early diagnosis and proper treatment are vital to reduce symptoms.
Distinguishing Features from Other Bleeding Disorders
Von Willebrand disease is often compared to hemophilia A because of factor VIII involvement. But, it’s different because of Von Willebrand factor’s role in platelet adhesion and factor VIII stability. It has unique symptoms and treatments.
The main difference is Von Willebrand factor’s role in platelet function. This sets it apart from disorders like hemophilia A and B, which mainly affect clotting factors.
Hemophilia A: Understanding Factor VIII Deficiency
Hemophilia A is a genetic disorder caused by a lack of clotting Factor VIII. It greatly affects the lives of those with it, leading to various bleeding issues.
Genetic Inheritance Patterns
Hemophilia A follows an X-linked recessive pattern. The gene for Factor VIII is on the X chromosome. Males, with only one X chromosome, are more likely to have it. Females can be carriers but rarely have two defective X chromosomes.
Male carriers pass the affected X chromosome to all daughters, making them carriers. Sons won’t get it from him. Female carriers have a 50% chance of passing the mutated gene to each child.
Severity Classifications and Their Impact
The severity of Hemophilia A depends on the Factor VIII activity in the blood. It’s divided into mild, moderate, and severe. Severe Hemophilia A has less than 1% Factor VIII activity, causing frequent bleeding.
- Mild Hemophilia A: Factor VIII activity between 5% and 40% of normal.
- Moderate Hemophilia A: Factor VIII activity between 1% and 5% of normal.
- Severe Hemophilia A: Factor VIII activity below 1% of normal.
Common Symptoms and Joint Complications
People with Hemophilia A often get bleeding in their joints, known as hemarthrosis. This can cause long-term joint disease and disability if not treated. Symptoms include:
- Pain and swelling in the affected joints.
- Reduced mobility and range of motion.
- Recurring bleeding episodes.
Managing Hemophilia A involves replacing Factor VIII through infusions. This can be done on-demand or regularly to prevent bleeding.
Hemophilia B: Key Facts About Factor IX Deficiency
Hemophilia B, or Factor IX deficiency, is a bleeding disorder passed down through families. It makes it hard for blood to clot. This happens because there’s not enough factor IX, a key protein for clotting.
Distinguishing Features from Hemophilia A
Hemophilia B and Hemophilia A share some symptoms, but they’re different in cause. Hemophilia A lacks factor VIII, while Hemophilia B lacks factor IX. Knowing the difference is key for the right treatment.
Both diseases are inherited in an X-linked recessive pattern. But, they have different genetic mutations and affect different proteins.
Prevalence and Demographics
Hemophilia B is less common than Hemophilia A, making up about 15-20% of cases. It affects roughly 1 in 20,000 to 1 in 30,000 males globally.
| Population | Prevalence of Hemophilia B |
| Global | 1 in 20,000 to 1 in 30,000 males |
| United States | Approximately 3,000 individuals |
| Europe | Varied, with higher prevalence in some countries |
Clinical Manifestations and Long-term Outcomes
Hemophilia B symptoms can vary from mild to severe. Those with severe cases often bleed into joints and muscles. This can cause chronic pain and disability if not treated.
Long-term outcomes have gotten better with new treatments. Prophylactic therapy can stop many bleeding complications.
Early diagnosis and treatment are vital for a better life with Hemophilia B.
Laboratory Diagnosis of Hemostasis Disease
Diagnosing hemostasis diseases needs a detailed approach with many lab tests. These tests are key to finding the cause of bleeding disorders. They also help in choosing the right treatment.
PT and aPTT in Hemophilia and von Willebrand Disease
The prothrombin time (PT) and activated partial thromboplastin time (aPTT) are first tests to check coagulation. PT checks the extrinsic and common pathways. aPTT looks at the intrinsic and common pathways.
In hemophilia A and B, aPTT is usually long, but PT is normal. Von Willebrand disease can also make aPTT long because it affects factor VIII.
Specific Factor Assays and Their Interpretation
Specific factor assays measure the levels of clotting factors. These tests are key for diagnosing specific bleeding disorders. They help find out how severe the disorder is and guide treatment.
In hemophilia A, factor VIII assay levels show how severe the disease is. It can be mild, moderate, or severe based on the factor activity left.
Genetic Testing and Family Screening
Genetic testing is important for finding the genetic causes of inherited bleeding disorders. This info is vital for family screening and counseling. It helps identify carriers and affected family members, allowing for better management and prevention.
Genetic testing is also used for prenatal diagnosis in families with a history of severe bleeding disorders.
Bleeding Disorders in Childhood: Recognition and Management
Spotting bleeding disorders in kids is key to bettering their lives. These conditions can show up in many ways, making diagnosis and treatment tricky.
Early Warning Signs and Symptoms
Kids with bleeding disorders might bruise easily, get frequent nosebleeds, or have joint pain. These signs can point to conditions like hemophilia or von Willebrand disease.
Common early warning signs include:
- Frequent or prolonged bleeding after minor injuries
- Easy bruising without apparent cause
- Nosebleeds that are difficult to stop
- Bleeding into joints, causing pain and swelling
Diagnostic Approach to Pediatric Bleeding Tendencies
Diagnosing bleeding disorders in kids takes a detailed look. This includes a medical history, physical check-up, and lab tests. First, tests like the prothrombin time (PT) and activated partial thromboplastin time (aPTT) are used to check for clotting issues.
Specific diagnostic tests may include:
- Factor VIII and IX assays for hemophilia A and B
- Von Willebrand factor antigen and activity tests
- Platelet function tests to assess platelet disorders
Finding the right diagnosis is vital for the right treatment plan.
Impact on Growth, Development, and Physical Activity
Bleeding disorders can affect a child’s growth, development, and physical activities. For example, joint bleeds can lead to chronic disease and mobility problems if not managed well.
| Aspect | Impact of Bleeding Disorders | Management Strategies |
| Growth | Potential for delayed growth due to chronic illness | Regular monitoring of growth parameters |
| Development | May experience developmental delays due to recurrent bleeding episodes | Early intervention programs and physical therapy |
| Physical Activity | Limited participation due to risk of injury and bleeding | Prophylactic factor replacement therapy, safe exercise recommendations |
Managing bleeding disorders in kids needs a team effort. This includes doctors, pediatricians, physical therapists, and sometimes genetic counselors. They work together to tackle all parts of the condition.
Gender-Specific Aspects of Hemorrhagic Disorders
Women with hemorrhagic disorders face unique challenges. These include gynecological and obstetric issues. Symptoms can change throughout a woman’s life, from first period to menopause.
Menorrhagia and Other Gynecological Manifestations
Menorrhagia, or heavy menstrual bleeding, is common in women with bleeding disorders. It can cause iron deficiency anemia, affecting daily life. Other symptoms include:
- Prolonged menstrual bleeding
- Frequent bleeding episodes
- Severe dysmenorrhea
Table 1: Gynecological Manifestations in Women with Bleeding Disorders
| Symptom | Prevalence | Impact on Quality of Life |
| Menorrhagia | High | Significant |
| Dysmenorrhea | Moderate | Moderate |
| Ovulatory dysfunction | Variable | Variable |
Pregnancy Considerations and Management
Pregnancy for women with hemorrhagic disorders needs careful planning. The risk of bleeding increases during and after pregnancy. Key considerations include:
- Close monitoring of clotting factor levels
- Planning for delivery and postpartum care
- Availability of clotting factor replacement therapies
Challenges in Diagnosis Among Different Populations
Diagnosing hemorrhagic disorders can be tough. Symptoms vary, and other health issues can complicate diagnosis. Each population has unique challenges, needing specific approaches.
Diagnosing and managing hemorrhagic disorders in women requires a team effort. It’s important to consider each patient’s unique needs and situation.
Treatment Approaches for Bleeding Disorders
Managing bleeding disorders well is key. Conditions like hemophilia and von Willebrand disease can really affect someone’s life if not treated right.
Factor Replacement Therapies: On-Demand vs. Prophylaxis
Factor replacement therapy is a mainstay in treating bleeding disorders. It uses products to replace missing clotting factors. There are two main ways to use it: on-demand and prophylaxis.
On-demand treatment is given when someone bleeds. It helps stop the bleeding but might not prevent long-term damage.
Prophylaxis, or regular infusions, aims to prevent bleeding. It has been shown to reduce bleeds and protect joints, improving life quality.
| Treatment Approach | Description | Benefits |
| On-Demand | Treatment administered at the time of a bleeding episode | Effective for acute bleeds |
| Prophylaxis | Regular infusion of clotting factors to prevent bleeding | Reduces frequency of bleeds, minimizes joint damage |
Non-Factor Replacement Options
New treatments are being explored for bleeding disorders. These include ways to enhance clotting or stabilize clots, not just replacing factors.
Epicizumab is a promising therapy. It’s a monoclonal antibody that helps with hemophilia A. It has shown to reduce bleeding in patients, even those with inhibitors.
“The introduction of non-factor replacement therapies represents a significant advancement in the treatment of bleeding disorders, providing new options for those who don’t respond to traditional treatments.”
Gene Therapy: Current Status and Future Prospects
Gene therapy is a new way to treat bleeding disorders. It aims to fix the genetic issue causing the disorder. This could offer a lasting solution.
Trials for gene therapy in hemophilia A and B are showing promise. It has the power to cut down on bleeding and improve life quality for those with severe hemophilia.
Gene therapy is in its early days but looks very promising. More research and trials are needed to make it safe and effective for everyone.
Living with Coagulation Disorders: Management Strategies
Living with a coagulation disorder can be tough, but the right strategies can help. Understanding your condition, making lifestyle changes, and being ready for emergencies are key. Also, using support resources is important.
Lifestyle Modifications and Activity Recommendations
Managing a coagulation disorder means making lifestyle changes. Avoid risky activities like contact sports and choose safer ones like swimming or cycling. Dietary adjustments are also key; eat a balanced diet full of vitamins and minerals.
Exercise is good, but it must fit your condition. Gentle exercises like yoga can help without putting too much strain.
Emergency Preparedness and Home Treatment
Being ready for emergencies is critical for those with coagulation disorders. Have a plan for emergencies, like knowing the nearest hospital. Keep necessary medications at home. Home treatment kits should be easy to find.
Teach family and caregivers about emergency responses. They should know how to give first aid and spot severe bleeding signs.
| Emergency Preparedness Steps | Action Items |
| 1. Know your emergency contacts | Keep a list of emergency numbers, including your doctor and family members. |
| 2. Have a home treatment kit | Ensure it’s easily accessible and that all family members know its location. |
| 3. Educate family and caregivers | Train them on administering first aid and recognizing severe bleeding signs. |
Support Resources and Patient Advocacy Organizations
Support from patient advocacy groups can greatly improve life for those with coagulation disorders. These groups offer resources, guidance, and community support.
Groups like the Hemophilia Federation of America and the World Federation of Hemophilia provide educational materials, advocacy, and networking chances.
Conclusion
It’s important to understand coagulation bleeding disorders and hemostasis disease. This knowledge helps in diagnosing and managing these conditions effectively. We’ve looked at how normal hemostasis works, the types of bleeding disorders, and how to treat them.
Bleeding disorders like von Willebrand disease and hemophilia can really affect people’s lives. Getting the right diagnosis and treatment is key. It helps reduce symptoms and prevents serious problems later on.
We’ve shared important information about these conditions. Our goal is to increase awareness and understanding of hemostasis disease. This will help improve care and outcomes for those dealing with coagulation bleeding disorders.
FAQ
What are coagulation bleeding disorders?
Coagulation bleeding disorders affect how the body makes blood clots. This leads to too much bleeding. They can be passed down or happen later in life. Examples include hemophilia A and B, and von Willebrand disease.
What is the difference between hemophilia A and hemophilia B?
Hemophilia A is caused by a lack of factor VIII. Hemophilia B is caused by a lack of factor IX. Both cause bleeding problems but are different in how they are inherited.
What is von Willebrand disease?
Von Willebrand disease is the most common bleeding disorder. It’s caused by not enough or not working von Willebrand factor. This protein helps platelets stick and protects factor VIII.
How are bleeding disorders diagnosed?
Doctors use tests like PT, aPTT, and specific factor assays. They also do genetic tests to find the cause.
What is the role of PT and aPTT in diagnosing hemophilia?
PT is usually normal in hemophilia. But aPTT is long. Specific tests confirm the type and how severe it is.
How do bleeding disorders affect children?
They can slow growth and limit physical activities. Finding and treating it early is key to avoiding serious problems.
What are the treatment options for bleeding disorders?
Treatments include replacing missing factors, non-factor options, and gene therapy. Gene therapy might cure it in the future.
How can individuals with bleeding disorders manage their condition?
They can change their lifestyle, avoid certain activities, and be ready for emergencies. Support groups also help a lot.
What is the opposite of hemophilia?
The opposite is thrombophilia. It’s when blood clots too easily.
What disorder is associated with a deficiency of clotting factors?
Disorders like hemophilia A and B, and von Willebrand disease are linked to a lack of clotting factors.
Which hereditary disorder involves impairment of the blood clotting mechanism?
Disorders like hemophilia A and B, and von Willebrand disease affect blood clotting.
How does hemophilia A affect the body?
It hampers blood clotting because of a factor VIII deficiency. This causes a lot of bleeding and can damage joints.
What are the clinical manifestations of von Willebrand disease?
Symptoms include easy bruising, nosebleeds, and heavy periods. These are signs of the disease.
Reference
- National Heart, Lung, and Blood Institute. (n.d.). Bleeding disorders: What are bleeding disorders? U.S. Department of Health and Human Services.https://www.nhlbi.nih.gov/health/bleeding-disorders


































