Last Updated on November 26, 2025 by Bilal Hasdemir
A colonoscopy is a test to check the colon for cancer or other issues. It’s important to find problems early to prevent cancer. Medicare helps make this test available to many people in the U.S.
Medicare pays for colonoscopies at certain times for people at risk of colorectal cancer. Knowing what to expect and how your coverage works is key. Liv Hospital is here to help you understand and prepare for your test.
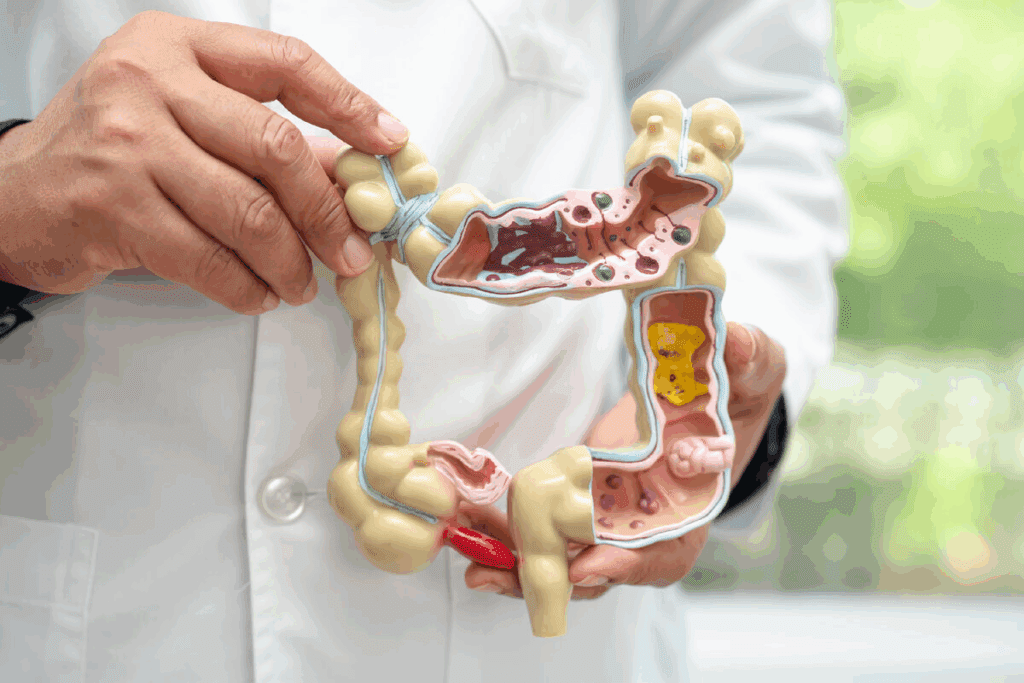
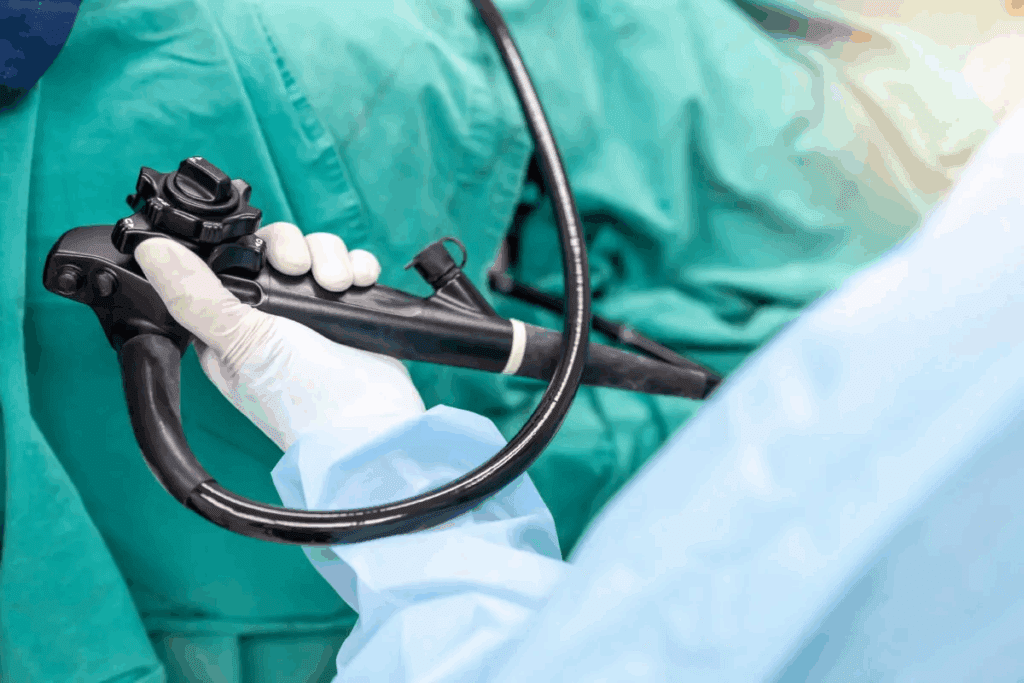
Millions of colonoscopies are done every year. It’s key for Medicare users to know what it is. A colonoscopy lets doctors see inside the colon and rectum. They look for polyps, cancer, and other issues.
Colonoscopies mainly check for colorectal cancer. This is a common cancer in the U.S. Early detection can greatly improve treatment results. It can also stop cancer by removing polyps before they turn into cancer.
Screenings also find other problems like diarrhea and rectal bleeding. Finding these early can help doctors start treatment. This can lower the chance of serious problems.
Medicare pays for screenings for those at risk for colorectal cancer. People with a family history of cancer, those who’ve had polyps or cancer before, and those with certain genetic syndromes are at higher risk. They might need more tests.
About 15 million colonoscopies are done in the U.S. every year. This shows how important it is for our health.
A colonoscopy is used to find the cause of symptoms like bleeding. It’s also used to prevent cancer by removing polyps.
Knowing how colonoscopies help diagnose and prevent problems helps Medicare users. They can take steps to stay healthy.

Medicare’s policies on colonoscopies aim to support preventive care. It’s key for Medicare recipients to grasp the basics of coverage. This knowledge helps them navigate the process smoothly.
Original Medicare (Parts A and B) pays for colonoscopy screenings if the doctor accepts Medicare. This is a big help for those needing the test, as it reduces financial stress.
Medicare Part B covers colonoscopies for medical or preventive reasons. It pays 100% of the Medicare-approved amount for preventive screenings if the doctor accepts Medicare.
“The Centers for Medicare & Medicaid Services (CMS) highlights the role of preventive screenings like colonoscopies in catching colorectal cancer early,” their guidelines say.
Medicare Advantage plans, or Part C, must include all Original Medicare services, including colonoscopies. But, the details like copays and coinsurance can differ by plan. It’s important for beneficiaries to check their plan’s specifics.
It’s vital to know the difference between preventive and diagnostic colonoscopies for Medicare coverage. Preventive colonoscopies are covered fully without extra costs if the doctor accepts Medicare. But, diagnostic colonoscopies might have extra fees if polyps are removed or if it’s not just a screening.
People should talk to their doctors to figure out the type of colonoscopy they need. This helps understand the costs and what’s covered.
The frequency of Medicare-covered colonoscopy screenings depends on the beneficiary’s risk factors. Medicare covers these screenings at safe and effective intervals. This helps detect colorectal cancer early and prevent it by removing precancerous polyps.
For those at average risk of colorectal cancer, Medicare covers screenings every 10 years. This is based on guidelines that say a 10-year cycle is enough for early cancer detection. It applies to those without a history of colorectal cancer or other risk factors.
Those at high risk for colorectal cancer can get screenings more often. Medicare covers colonoscopies every 24 months for those with a history of colorectal cancer or adenomatous polyps. It also covers those with other risk factors.
It’s important to know that Medicare doesn’t have age limits for colonoscopy coverage. Beneficiaries can get covered colonoscopies as long as they’re in Medicare, no matter their age. This lets older adults keep getting preventive care and surveillance.
Knowing when Medicare covers colonoscopy screenings helps with planning preventive care. By understanding their eligibility, individuals can stay healthy and catch issues early.
Getting a positive Cologuard test result can raise many questions. Luckily, Medicare covers colonoscopies after a positive test well. A positive test means there are abnormal cells or blood in the stool, needing more checks.
Cologuard is a test that looks for DNA changes and blood in stool. It’s for people at average risk of colorectal cancer. It’s less invasive than a colonoscopy.
Key aspects of Cologuard include:
Medicare pays for colonoscopies after a positive Cologuard test. This is important because a positive test means more tests are needed to find the cause.
Medicare’s coverage includes:
To get Medicare to cover a colonoscopy after a positive Cologuard test, you need some documents. You’ll need the positive Cologuard test result and a doctor’s order for a colonoscopy.
Required documentation may include:
Knowing about Medicare’s coverage and what to do after a positive Cologuard test can help. It makes the diagnostic process clearer and more confident.
It’s important to know about Medicare colonoscopy coverage in different parts of the U.S. Medicare is a federal program. But, knowing how it works locally can help you better.
Medicare’s rules for colonoscopies are set by National Coverage Determinations (NCDs). These decisions are made by Medicare to see if a service or procedure is covered. These rules are the same everywhere, so all Medicare users get the same care no matter where they are.
“NCDs are critical in ensuring that Medicare beneficiaries receive consistent and high-quality care across different regions.”
Source: Medicare.gov
NCDs cover things like how often you can get a colonoscopy, who can do it, and where. Medicare wants to make sure you get good and safe care.
Understanding how Medicare works in places like Texas is key. Even though Medicare’s rules are the same everywhere, how services are available can differ.
| State | Medicare Coverage for Colonoscopy | Average Cost to Beneficiary |
| Texas | Covered under Medicare Part B | $0 – $20 |
| California | Covered under Medicare Part B | $0 – $20 |
| New York | Covered under Medicare Part B | $0 – $20 |
The table shows that Medicare covers colonoscopies the same way in Texas, California, and New York. You can expect the same coverage and costs, no matter where you are.
To find Medicare-approved places for colonoscopies, use Medicare.gov or call your local Medicare office. It’s important to pick a place that Medicare has approved to make sure you’re covered.
By understanding regional differences and using the right resources, Medicare users can get the colonoscopy screenings they need. This helps them stay healthy.
It’s important for Medicare beneficiaries to know about the costs of colonoscopy screenings. Medicare does cover colonoscopies, but the cost can change based on the reason for the test and what services are included.
For people at average risk of colorectal cancer, Medicare pays for screening colonoscopies every 10 years. Preventive colonoscopies are usually covered without any extra costs if done by a Medicare-approved doctor. This means you won’t have to pay anything out-of-pocket for the test when it’s for screening.
If polyps or abnormal tissue are found and removed during a colonoscopy, it’s considered a diagnostic test. In these cases, you’ll have to pay 15% of the Medicare-approved cost. This is because removing polyps or tissue adds a diagnostic part to the test.
There’s also a 15% coinsurance for any diagnostic services during a colonoscopy. You should also know about deductibles and out-of-pocket maximums. For Medicare Part B, which covers colonoscopies, there’s an annual deductible. After you meet this deductible, the coinsurance kicks in. Some Medicare Advantage plans also have an out-of-pocket maximum, which can limit your yearly costs.
It’s a good idea to talk to your healthcare provider and check your Medicare coverage. This will help you understand the costs of your colonoscopy. Make sure your doctor is Medicare-approved and know about any extra fees for facility or anesthesia services.
It’s important for Medicare beneficiaries to know how supplements affect colonoscopy coverage. Most have extra coverage that helps with Medicare costs. The coverage can change based on the procedure, where it’s done, or who does it.
Medicare Supplement Insurance, or Medigap, can help with colonoscopy costs that Original Medicare doesn’t cover. This includes coinsurance, copayments, and deductibles. The right Medigap plan can lower your costs for colonoscopy screenings.
Some Medigap plans cover more for colonoscopy coinsurance than others. Plans F and G stand out because they cover Part B coinsurance for colonoscopies. It’s key to look at your options to find the best plan for you.
For example, if a colonoscopy leads to polyp removal, Medicare Part B covers it but might ask for a coinsurance payment. A good Medigap plan can cover this, saving you money.
When looking at Medigap plans, focus on their coverage for colonoscopies and other preventive services. Look for plans that cover Part B coinsurance and other costs for colonoscopies.
Before picking a Medigap plan, ask your provider these questions to understand colonoscopy coverage:
Knowing how Medicare supplements affect colonoscopy coverage helps beneficiaries plan their healthcare and finances better.
Getting ready for your Medicare-covered colonoscopy involves a few key steps. Medicare does cover colonoscopy tests. But, knowing the prep work needed is important to avoid any problems.
First, check if your Medicare plan needs pre-authorization for your colonoscopy. Some Medicare Advantage plans might require a referral from your primary doctor.
Verify with your provider if a referral is needed. Also, find out what documents you’ll need for pre-authorization. This can prevent delays in your procedure.
Make sure to check your coverage and costs before the procedure. Medicare does cover colonoscopy tests. But, your out-of-pocket costs might vary based on your plan.
It’s a good idea to confirm exact costs with your doctor before. Knowing what you’ll pay can help you plan your finances better.
Collecting the right documents before your colonoscopy makes things easier. You’ll need your Medicare card, ID, and any medical history.
Having these documents ready helps your healthcare provider’s office process your procedure smoothly.
Learning about the colonoscopy procedure can ease worries and make the experience smoother for those on Medicare. This test is key for finding colon cancer and other gut problems. Medicare helps cover it, making it easier for those who need it.
Getting ready for a colonoscopy is a big step. You’ll need to stick to a special diet and bowel prep to clear your colon. This means:
Liv Hospital stresses the importance of following these steps closely. Right preparation is essential for a good colonoscopy.
On the day of your colonoscopy, you’ll:
The test itself is short, but the whole day might take a few hours. Medicare pays for the facility, doctor, and any needed tests.
After the test, you’ll be watched for a bit before going home. You might feel:
It’s vital to follow your doctor’s advice for aftercare, including what to eat and when to come back. Aftercare is key for the best results.
“A colonoscopy is a valuable tool for preventing colon cancer. By understanding what to expect, patients can feel more comfortable and prepared for the procedure.” – Dr. John Smith, Gastroenterologist
In summary, knowing about the colonoscopy can lessen anxiety and make the experience better for Medicare users. By getting ready, knowing what happens during the test, and following up, you can get the most out of this important screening.
It’s important to know about Medicare’s colonoscopy coverage. This is key for making smart health choices. Medicare helps a lot with colonoscopy costs, which is great for catching cancer early.
Medicare often covers colonoscopies without extra costs. But, if polyps are removed, you might have to pay a bit. Always check with Medicare to know the exact costs.
Knowing about Medicare’s colonoscopy coverage helps you stay healthy. Regular colonoscopies can stop cancer before it starts. With Medicare’s help, you can feel safe and sound about your health.
Yes, Medicare covers colonoscopy tests. Medicare Part B pays for them as a preventive service. Medicare Advantage plans also cover them.
Medicare pays for colonoscopies every 10 years for those at average risk. For those at high risk, it’s every 24 months. There’s no age limit for coverage.
Medicare pays 100% for preventive screening colonoscopies. This means no coinsurance or copayment. But, a 15% coinsurance might apply if polyps are removed.
Yes, Medicare covers a follow-up colonoscopy after a positive Cologuard test. Cologuard is a test for colorectal cancer. A positive result means a colonoscopy is needed for diagnosis.
Medicare’s colonoscopy coverage is the same everywhere due to national policies. But, you must use Medicare-approved facilities in your state, like Texas, to get coverage.
Medicare supplements, or Medigap plans, can help with costs for colonoscopies. Some plans cover the 15% coinsurance for removing polyps.
The rules for pre-authorization and referrals vary by Medicare plan. Always check with your plan before your procedure.
Before, you’ll get instructions and dietary rules. During, you’ll be sedated and a gastroenterologist will do the procedure. After, you’ll be watched and given care instructions.
Medicare Part B has a deductible for colonoscopies. Out-of-pocket maximums also apply, depending on your plan. Always check your plan’s details for costs.
Yes, Medicare covers colonoscopies for anyone, regardless of age. There’s no age limit for coverage.
If polyps are found and removed, Medicare might cover it as a diagnostic procedure. A 15% coinsurance might apply for removing polyps.
ShrEstha, G. (2023). Spigelian hernia: A rare case presentation and review of literature. Journal of Surgical Case Reports. Retrieved from https://www.sciencedirect.com/science/article/pii/S2210261223002079
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!