Last Updated on December 2, 2025 by Bilal Hasdemir
Colorectal conditions often need surgery. Knowing about the colorectal surgery procedure can ease worries. Discover how the colorectal surgery procedure is performed and what recovery timeline to expect.
Surgeries for the anus, rectum, and intestine are complex. They use different colorectal surgery methods. These surgeries help treat colon cancer, diverticulitis, and inflammatory bowel disease.
The exact how colorectal surgery is done varies. It depends on the condition, the patient’s health, and the surgeon’s expertise. New techniques make surgeries less invasive. This cuts down recovery time and boosts success rates.
Key Takeaways
- Colorectal surgery includes many procedures.
- The choice of colorectal surgery technique depends on several factors.
- Minimally invasive surgeries are becoming more common.
- Understanding the steps in colorectal surgery can help patients prepare.
- Surgeons tailor their approach to each patient’s needs.
Understanding Colorectal Surgery
Colorectal surgery treats diseases of the colon and rectum. It uses various methods to fix problems in the digestive system. These methods are precise and effective.
Common Conditions Requiring Surgical Intervention
Many conditions need colorectal surgery. Knowing these conditions helps patients understand their treatment options.
Colorectal Cancer
Colorectal cancer is a common reason for surgery. The surgical process colorectal cancer involves removing the tumor. Early detection improves surgical outcomes.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) may need surgery when medicine doesn’t work. Colorectal surgery techniques depend on the disease’s extent and location.
Diverticulitis
Diverticulitis is inflammation of the colon’s diverticula. Severe cases may need surgery. The types of colorectal surgery for diverticulitis include removing the affected part.
| Condition | Common Surgical Interventions | Goals of Surgery |
| Colorectal Cancer | Tumor resection, colectomy | Remove cancerous tissue, restore bowel function |
| Inflammatory Bowel Disease | Colectomy, proctocolectomy, ileostomy | Remove diseased bowel, manage symptoms |
| Diverticulitis | Resection of affected colon segment | Remove inflamed diverticula, prevent complications |
When Surgery Becomes Necessary
Surgery is needed when other treatments fail. It’s also necessary when a condition is risky. The decision to have surgery depends on the patient’s health, the condition’s severity, and the surgery’s benefits and risks.
The steps in colorectal surgery are well-planned. Knowing the colorectal surgery technique and types of colorectal surgery helps patients make informed choices.
Pre-Surgical Evaluation and Diagnosis
Before surgery, doctors do a lot of tests to figure out what’s wrong and how to fix it. This is a key part of getting ready for colorectal surgery.
Diagnostic Tests and Imaging
Tests are very important in deciding if you need surgery and how to do it. They show how serious the problem is and what surgery is best.
Colonoscopy
A colonoscopy lets doctors see inside your colon and rectum. They use a special tube with a camera. It’s a key test for finding problems like polyps and tumors.
Benefits of Colonoscopy:
- Direct look at the colon and rectum
- Can take samples for more tests
- May remove polyps during the test
CT Scans and MRI
CT scans and MRI give detailed pictures of inside your body. They help doctors see how far the disease has spread. They also help plan the surgery and check if other tissues are affected.
| Imaging Test | Primary Use | Benefits |
| CT Scan | Checking how far the disease has spread and planning surgery | Fast and detailed pictures |
| MRI | Looking at soft tissue involvement | Clear images of soft tissues |
Consultation with Colorectal Surgeons
After tests, you’ll talk to a colorectal surgeon. They’ll go over the test results, if surgery is needed, and what surgery options you have.
“Talking to a colorectal surgeon helps you understand your diagnosis, the surgery plan, and what to expect after.”
This meeting is a chance to talk about your health history, test results, and surgery risks and benefits. It’s also a time to ask questions and learn about the surgery process.
Preparing for Colorectal Surgery
Getting ready for colorectal surgery is key to a smooth process. It involves making medical, dietary, and lifestyle changes. These steps help reduce risks and aid in recovery.
Bowel Preparation Process
The bowel prep is a vital step before surgery. It cleanses the bowel to lower infection risks and ensure a clear surgical area. This prep includes dietary changes, laxatives, and enemas, as directed by your doctor.
Bowel prep is key to lowering surgical risks. It starts a day or two before surgery. Following the prep instructions carefully is essential for success.
| Bowel Preparation Method | Description | Timing |
| Laxatives | Medication to induce bowel movements | Day before surgery |
| Enemas | Fluids introduced into the bowel to cleanse it | Evening before or morning of surgery |
| Dietary Changes | Clear liquid diet or specific foods to avoid | 1-2 days before surgery |
Dietary Restrictions
Changing your diet is a big part of getting ready for surgery. You might need to eat only clear liquids or avoid certain foods. It’s vital to follow your surgeon’s or dietitian’s advice closely.
Medication Management
Managing your medications is also important. Tell your healthcare team about all the drugs, supplements, and vitamins you take. Some might need to be changed or stopped before surgery to avoid problems.
- Blood thinners may need to be stopped to reduce bleeding risks.
- Diabetes medications may require adjustment based on dietary changes.
- Certain supplements can increase the risk of bleeding and may need to be discontinued.
Mental and Physical Preparation
Mental and physical readiness are key to surgery success and recovery. Stay hydrated, rest well, and manage stress with relaxation techniques or counseling if needed. Being mentally prepared can greatly impact recovery.
Types of Colorectal Surgery Procedures
Colorectal surgery includes many procedures for the colon and rectum. The right procedure depends on the patient’s health and the surgeon’s advice.
Colectomy (Colon Removal)
A colectomy removes part or all of the colon. It’s needed for colon cancer, severe diverticulitis, or inflammatory bowel disease.
Total Colectomy
A total colectomy removes the whole colon. It’s for severe conditions like FAP or ulcerative colitis that covers the whole colon.
Partial Colectomy
A partial colectomy removes only the sick part of the colon. It’s used for localized issues like colon cancer or diverticulitis.
Rectal Resection
Rectal resection removes part or all of the rectum. It’s for rectal cancer or severe disease. The surgery can be open, laparoscopic, or robotic-assisted.
Colostomy and Ileostomy
Colostomy and ileostomy create an opening in the abdomen for feces. They’re for severe colorectal disease or injury.
Temporary vs. Permanent Ostomies
Ostomies can be temporary or permanent. Temporary ones help the colon or rectum heal. Permanent ones are for severe or irreversible conditions.
Hemorrhoidectomy and Other Minor Procedures
Hemorrhoidectomy removes swollen veins in the lower rectum or anus. Other minor procedures treat anal fissures or abscesses.
Knowing about colorectal surgery procedures helps patients make better choices. Each procedure has its own reasons, benefits, and risks. Patients should talk to a healthcare professional about these.
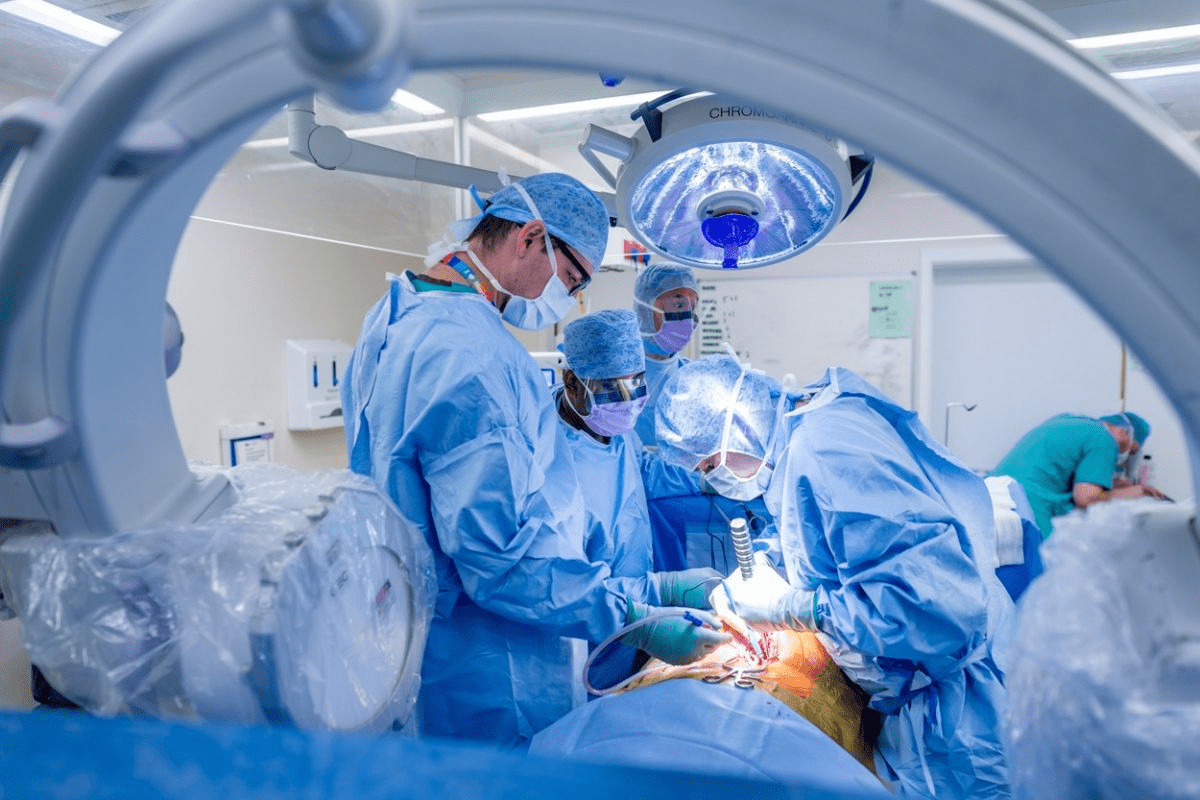
Open Colorectal Surgery Technique
Open colorectal surgery is a traditional method. It involves making a big incision to reach the colon or rectum. This approach has been around for decades and is used for many colorectal issues.
The Traditional Surgical Approach
This technique requires a big cut in the abdomen. It gives surgeons a clear view of the area they need to work on. It’s often chosen for complex cases where more access is needed.
Key aspects of the traditional approach include:
- A single large incision to access the colon or rectum
- Direct visualization of the surgical site
- The ability to perform complex procedures
When Open Surgery is Preferred
Open surgery is chosen for complex cases. This includes situations with big tumors, lots of adhesions, or when other methods won’t work. The choice depends on the patient’s condition and health.
Advantages and Limitations
The open method is good for complex surgeries and lets surgeons see the area clearly. But, it has downsides. These include a longer recovery, more pain, and a higher chance of complications compared to less invasive methods.
The advantages include:
- Direct access to the surgical site
- Ability to handle complex cases
The limitations include:
- Longer recovery period
- Increased postoperative pain
- Higher risk of complications
Recovery Expectations
Recovering from open colorectal surgery takes longer. Patients usually stay in the hospital for several days. They also need weeks at home to get better. Expect pain, tiredness, and a slow return to normal activities.
Key recovery expectations include:
- Hospital stay of several days to a week
- Several weeks of recuperation at home
- Gradual return to normal activities
Laparoscopic Colorectal Surgery Method
Laparoscopic colorectal surgery is a less painful option compared to traditional surgery. It uses small cuts for instruments and a camera. This way, the surgery is done without a big cut.
Minimally Invasive Approach
This method is less invasive, causing less damage and faster healing. Key benefits include less pain after surgery, lower infection risk, and shorter hospital stays.
- Smaller cuts mean less scarring.
- Less body trauma means quicker recovery.
- Less pain after surgery makes patients more comfortable.
Equipment and Technology Used
Advanced tools are key in laparoscopic surgery. These include high-definition cameras and special instruments. These tools help surgeons do precise work.
- High-definition cameras give clear views.
- Special instruments help with precise work.
- Advanced tools make dissection and stopping bleeding safe.
Benefits Over Open Surgery
Laparoscopic surgery has many advantages over open surgery. It causes less pain and faster recovery. Patients usually have less complications and can get back to normal faster.
| Aspect | Laparoscopic Surgery | Open Surgery |
| Pain Level | Less | More |
| Recovery Time | Faster | Slower |
| Scarring | Minimal | More extensive |
Limitations and Considerations
Despite its benefits, laparoscopic surgery has its limits. These include the need for special training, higher costs, and not being suitable for all cases.
- Surgeons need special training for this method.
- It costs more due to equipment and maintenance.
- Not all patients can have this surgery due to health reasons.
Robotic-Assisted Colorectal Surgery
Robotic-assisted colorectal surgery is a big step forward in surgery. It brings better precision, flexibility, and control than old methods.
Advanced Surgical Systems
At the heart of robotic-assisted surgery are advanced systems. These systems help surgeons do complex tasks more easily and accurately. They solve problems of old laparoscopic surgery, like less dexterity and motion limits.
The da Vinci Surgical System
The da Vinci Surgical System is a top choice for robotic surgery. It gives surgeons a clear, 3D view of the area being operated on. The system’s instruments mimic the human wrist, making dissection and suturing more precise.
Precision and Control Benefits
Robotic surgery brings many benefits to patients. These include less blood loss, fewer complications, and less pain after surgery. It also lets surgeons do more complex tasks with confidence.
Key benefits of robotic-assisted colorectal surgery include:
- Enhanced precision and control
- Reduced blood loss and fewer complications
- Less post-operative pain
- Shorter hospital stays
- Faster recovery times
Ideal Candidates for Robotic Surgery
Not everyone is a good fit for robotic surgery. The choice depends on the condition, the patient’s health, and the surgeon’s skill with robots.
Cost and Availability Factors
Robotic surgery costs more than traditional methods. This is because of the high cost of the systems and training staff. Not all places have these systems, which affects availability.
The future of colorectal surgery looks bright with robotic tech advancements. This could make these surgeries more common and affordable.
The Colorectal Surgery Procedure: Step by Step
Surgery for colorectal conditions involves a series of steps. Knowing these steps helps patients prepare for their procedure and recovery.
Anesthesia Administration
The first step is giving anesthesia. An anesthesiologist ensures the patient is comfortable and pain-free. The type of anesthesia depends on the procedure and the patient’s health.
Surgical Access and Exposure
After anesthesia, the team accesses the colorectal area. This can be through open surgery or minimally invasive methods like laparoscopy. The choice depends on the patient’s condition and the surgeon’s skill.
Resection and Removal Process
The main step is removing the diseased part of the colon or rectum. The surgeon carefully dissects and removes the affected area. They ensure the remaining parts are healthy for reconnection.
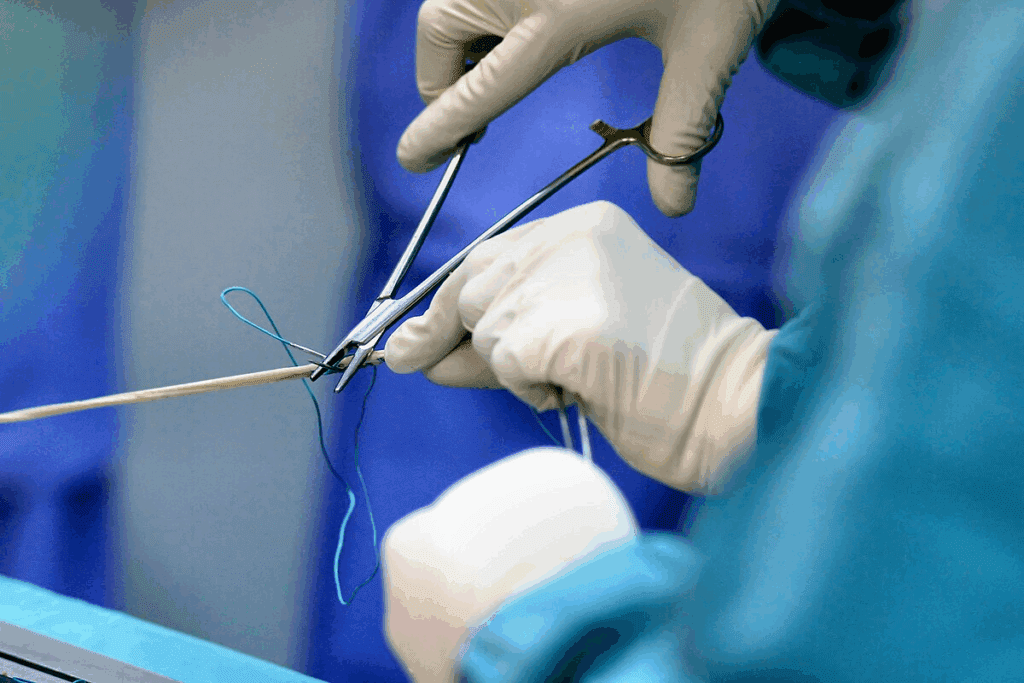
Anastomosis (Reconnection) Techniques
Next, the surgeon reconnects the remaining parts. This is done through various techniques, like hand-sewn or stapled anastomosis. The choice depends on the location and the surgeon’s preference.
Closure and Wound Care
The final step is closing the incision. For open surgery, this involves suturing or stapling. For minimally invasive procedures, small incisions are closed with sutures or staples. Proper wound care is key to prevent infection and promote healing.
Understanding colorectal surgery steps shows the complexity and care involved. Following the surgeon’s instructions for preparation and care is vital for a smooth recovery.
Post-Operative Care and Recovery
The post-operative care phase is very important. It needs careful attention and following medical advice. Recovery after colorectal surgery includes watching over the patient, managing pain, adjusting diet, and slowly getting back to normal activities.
Immediate Recovery Period
Right after surgery, patients are watched closely in the recovery room. They stay there until they are stable enough to move to a regular hospital room.
Hospital Stay Duration
The time spent in the hospital varies. It depends on the surgery type and the patient’s health. Usually, patients stay a few days to ensure they recover well and to handle any complications.
Monitoring Vital Signs
Heart rate, blood pressure, and oxygen levels are always checked. This helps spot any problems or distress quickly.
Pain Management Strategies
Managing pain well is key for a smooth recovery. This can involve epidural anesthesia, PCA, and oral pain meds.
Dietary Progression
Diet changes start with clear liquids and move to solid foods as the digestive system heals.
Clear Liquids to Solid Foods
First, patients get clear liquids to rehydrate and gently start the digestive system. As they get better, they start eating more solid foods.
| Dietary Stage | Foods Included | Duration |
| Clear Liquids | Broth, water, clear juice | 1-2 days |
| Liquid Diet | Soups, nutritional supplements | 2-3 days |
| Soft Foods | Mashed potatoes, cooked vegetables | 3-5 days |
| Regular Diet | Normal foods, gradually introduced | After 5 days |
Activity Restrictions and Gradual Return
Patients should avoid heavy lifting, bending, and hard activities at first. As they get better, they can start doing normal things again, with their doctor’s advice.
Long-term Recovery Timeline
Recovery time varies, but it usually takes weeks to fully recover from colorectal surgery. Regular check-ups with the surgeon are important to track healing and solve any issues.
Potential Complications and Risks
It’s important for patients to know about the risks of colorectal surgery. This helps them make better choices.
Common Complications
Like any big surgery, colorectal surgery has risks. Some common problems include:
Infection
Infection is a big risk after surgery. Signs of infection are fever, redness, swelling, and more pain at the site.
Bleeding
Bleeding can happen during or after surgery. Excessive bleeding might need blood transfusions or more surgery.
Anastomotic Leak
An anastomotic leak is when the intestine reconnects breaks down. This can cause serious infection and might need more surgery.
Warning Signs to Monitor
It’s key to watch for warning signs of complications. These include:
- Severe abdominal pain
- Fever or chills
- Redness or swelling at the surgical site
- Increased bleeding or discharge
- Nausea or vomiting
When to Contact Your Surgeon
If you see these symptoms, call your surgeon right away:
- Severe pain not helped by medicine
- Signs of infection
- Excessive bleeding
- Difficulty urinating or severe constipation
Long-term Side Effects
Some people might face long-term side effects after surgery. These can include:
- Bowel habit changes
- Bladder or sexual dysfunction
- Adhesions or scar tissue
Knowing about these risks helps patients prepare and know when to get medical help.
Conclusion
Understanding colorectal surgery is key for those facing surgery for colon or rectum issues. This article has given a detailed look at the procedures, from start to finish.
A summary of colorectal surgery shows the different methods used. These include open, laparoscopic, and robotic-assisted surgery. Each has its own benefits and drawbacks. The right choice depends on the patient’s health and the surgeon’s skills.
In conclusion, colorectal surgery is a complex process. It needs careful preparation, precise surgery, and good care after surgery. Knowing about colorectal surgery helps patients understand their treatment and recovery better. This leads to better results.
An overview of colorectal surgery procedures highlights the need for a team effort. Skilled surgeons, nurses, and healthcare professionals work together. As technology improves, so will surgery and care, making recovery better for patients.
FAQ
What is colorectal surgery?
Colorectal surgery is when doctors operate on the colon, rectum, or anus. They do this to treat diseases like cancer, inflammatory bowel disease, and diverticulitis.
How is colorectal surgery performed?
Doctors use different methods for colorectal surgery. These include open surgery, laparoscopic surgery, and robotic-assisted surgery. The choice depends on the patient’s health and the surgeon’s skills.
What are the different types of colorectal surgery procedures?
There are several types of colorectal surgery. These include colectomy, rectal resection, and colostomy. Each procedure has its own purpose and benefits.
What is the bowel preparation process for colorectal surgery?
Before surgery, patients follow a bowel prep process. This involves changing their diet and using laxatives and enemas. It helps clean the bowel and lowers the risk of complications.
How long does it take to recover from colorectal surgery?
Recovery time varies. It depends on the surgery type, the patient’s health, and how complex the procedure is. Generally, it takes weeks to months to fully recover.
What are the possible complications of colorectal surgery?
Complications can include infection, bleeding, and bowel obstruction. There can also be long-term effects like bowel dysfunction. Proper care after surgery is key to avoid these issues.
What is the difference between laparoscopic and open colorectal surgery?
Laparoscopic surgery uses small incisions and a camera for less pain and quicker recovery. Open surgery, on the other hand, involves a larger incision and takes longer to recover from.
What is robotic-assisted colorectal surgery?
Robotic-assisted surgery uses advanced robotic systems for more precise control. It’s beneficial for complex procedures and may reduce recovery time.
How is pain managed after colorectal surgery?
Pain management includes medication and epidural anesthesia. These methods help reduce discomfort and aid in a smooth recovery.
What dietary restrictions are necessary after colorectal surgery?
Patients start with clear liquids and gradually move to solid foods. The surgeon or healthcare team provides specific dietary advice to ensure a smooth recovery.
When should I contact my surgeon after colorectal surgery?
Contact your surgeon if you have severe pain, bleeding, or signs of infection. Also, reach out if you have any concerns about your recovery.
References
The Lancet. Evidence-Based Medical Insight. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(02)09290-5/fulltext





