Last Updated on November 14, 2025 by
Congenital anomalies of the gastrointestinal tract are a big health issue worldwide. They affect thousands of children. We will look at the four main pediatric gastrointestinal anomalies that are hard to diagnose and treat.
These birth defects of the digestive tract include esophageal atresia/tracheoesophageal fistula, duodenal atresia, anorectal Common Congenital GI malformations, and Hirschsprung’s disease. Studies show these conditions often cause intestinal obstruction. Signs include feeding troubles, a swollen belly, and vomiting.

It’s important to understand these gut development defects. This helps in early detection and effective treatment. It also improves the lives of affected families.
The development of the gut is complex. Disruptions during this time can cause various birth defects. These defects can greatly affect a child’s life and their family’s well-being.
The gut’s development is a detailed process. It involves the formation of the foregut, midgut, and hindgut. The primitive gut forms into different parts, like the esophagus and small intestine.
Any issues during this time can lead to problems. For example, intestinal atresia or congenital abdominal issues can occur.
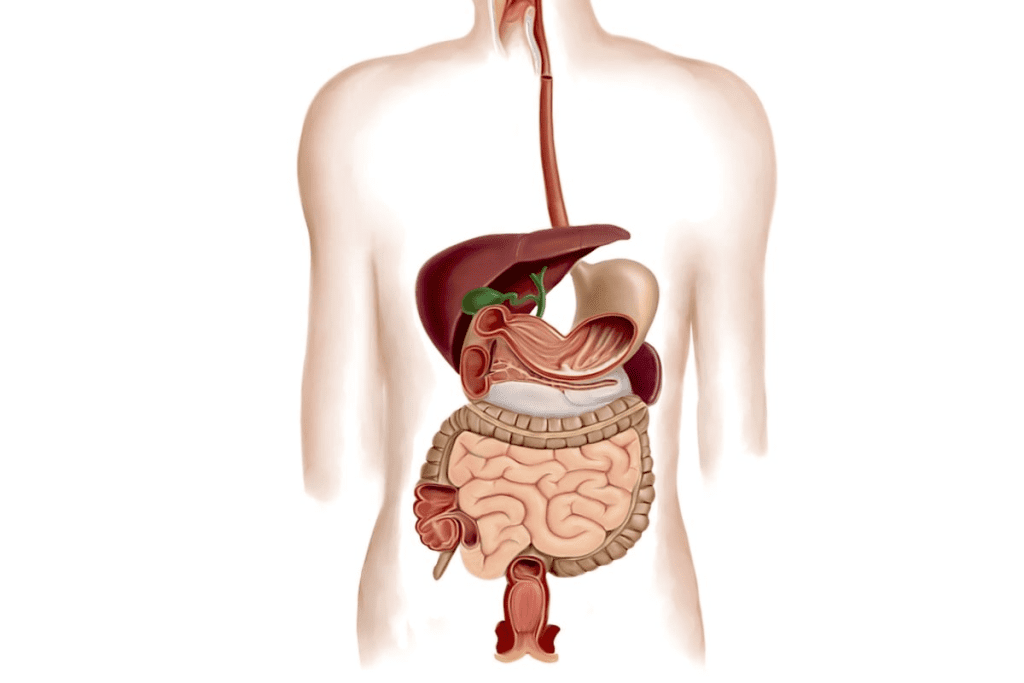
Congenital GI anomalies can be grouped by location and type. Types include esophageal atresia and intestinal malrotation. Knowing these classifications helps doctors plan the right pediatric surgical conditions.
In 2021, digestive birth defects affected 2.2 million kids. They caused over 47,000 deaths and 4.3 million DALYs. This shows how big of a health issue these conditions are worldwide.
It’s key to know about common congenital GI malformations for better healthcare planning. These malformations are a big cause of sickness and death in kids all over the world. We’ll look at how common they are, how many die from them, and how their numbers are changing.
Congenital GI malformations are rare but serious. For example, anal atresia and stenosis happen in about 2.1 cases per 10,000 live births in Europe. Gastroschisis is getting more common, with 4.5 per 10,000 live births now. Omphalocele rates vary from 0.6“4.8 per 10,000.
Death from congenital GI malformations is a big worry. These issues cause a lot of sickness and death in babies. They also lead to a lot of disability-adjusted life years (DALYs). This affects families and healthcare systems a lot, showing we need better ways to manage and prevent these problems.
Recent studies show changes in how often certain GI malformations happen. For example, gastroschisis is becoming more common in some places. Knowing these changes helps us find out why and how to stop them. We must keep watching these trends to help improve healthcare.
Esophageal atresia and tracheoesophageal fistula are birth defects that affect the stomach’s ability to digest food in newborns. These issues arise from problems during fetal development. They can lead to serious problems with eating, breathing, and overall health.
Esophageal atresia happens when the esophagus doesn’t form correctly. Sometimes, it connects to the trachea, causing more problems. Knowing the different types is key for doctors to plan the best treatment.
These issues start in the womb when the esophagus and trachea don’t separate properly. Disruptions in this process can lead to various forms of esophageal atresia and tracheoesophageal fistula. Early detection and care are very important.
Newborns with these conditions often show symptoms right after birth. They might drool a lot, spit up, and have trouble breathing if there’s a fistula. It’s important to notice these signs early to get help fast.
First, doctors use a tube to help the baby’s stomach. This helps prevent vomiting and keeps the baby stable. Then, they can plan for surgery.
Doctors use several ways to diagnose these conditions. They look for signs, take X-rays, and do special tests. An X-ray can show if the tube is stuck in the esophagus. Tests with contrast can find fistulas.
Surgery is the main treatment for these conditions. The goal is to fix the esophagus and remove the fistula. The type of surgery depends on the specific problem and the baby’s health.
After surgery, babies might face issues like leaks, strictures, and acid reflux. They need ongoing care to manage these problems and get better.
Duodenal atresia is a birth defect that blocks the duodenum, the first part of the small intestine. It needs early treatment. This blockage stops the normal flow of food through the intestine.
The cause of duodenal atresia is linked to how the small intestine forms in the womb. Normally, the duodenum starts to form and open up early in pregnancy. But, in duodenal atresia, this process goes wrong, causing a blockage.
Key factors in the cause include genetics and the environment. These can affect how the duodenum develops.
Children with Down syndrome are more likely to have duodenal atresia. This shows why genetic tests are important.
Also, duodenal atresia is linked to the VACTERL association. This group includes problems like spinal issues, anal problems, heart issues, and limb problems.
Children with duodenal atresia often have vomiting and a swollen belly right after birth. A key sign is the “double bubble” on X-rays. This shows two air-filled parts (the stomach and the duodenum) with no air in the rest of the intestine.
To fix duodenal atresia, doctors perform surgery. They might do a duodeno-duodenostomy or a duodeno-jejunostomy.
Postoperative care is very important. It helps the baby recover and makes sure they get the right food.
Anorectal malformations are congenital defects that affect the anus and rectum. They need quick diagnosis and treatment to avoid long-term issues.
Anorectal malformations are classified by the level of the defect and any other anomalies. The Krickenbeck classification is a key system used. It sorts these malformations by the type of fistula.
These malformations vary from simple to complex. Knowing these variations helps doctors choose the right surgery.
Many babies with anorectal malformations also have urogenital issues. These can include kidney problems, bladder issues, and genital malformations. It’s important to check for these conditions.
Diagnosing anorectal malformations involves clinical exams, imaging, and sometimes endoscopy. X-rays and ultrasound help see the defect’s level and any other issues.
A distal loopogram helps show the rectum’s anatomy and any fistulas.
Surgery for anorectal malformations is often done in stages. The first step might be a colostomy to manage waste. Then, a more detailed repair is done later.
The posterior sagittal anorectoplasty (PSARP) is a common repair method. It aims to make the anus and rectum work properly.
Every patient is different. The surgery plan must fit the patient’s unique needs and conditions.
Hirschsprung’s disease is a serious issue with the gut. It happens when there are no nerve cells in the lower colon and rectum.
This condition affects how the gut works. The absence of ganglion cells in the lower bowel causes a blockage. This is because the bowel can’t relax and move stool. It leads to severe constipation or blockage.
The cause of Hirschsprung’s disease is linked to the abnormal migration of neural crest cells. Normally, these cells move to the gut and become the ganglion cells. But in Hirschsprung’s, they don’t move right, causing a lack of these cells in the lower bowel.
“The failure of neural crest cells to migrate to the distal bowel results in the characteristic aganglionosis seen in Hirschsprung’s disease.”
Hirschsprung’s disease has a genetic component. Several genes are involved, with RET being the most common. Other genes like EDNRB and GDNF also play a part. The way it’s passed down can be complex, with both dominant and recessive patterns.
The symptoms of Hirschsprung’s disease change with age. Newborns often have trouble passing meconium and may get bloated and vomit. Older kids might have long-term constipation, bloating, and a poor appetite.
Diagnosing Hirschsprung’s disease requires a few steps. Contrast enemas can spot the transition zone. But the only sure way is a rectal biopsy. This shows if there are ganglion cells or not.
To prevent congenital gastrointestinal anomalies, we need to know the risk factors. By understanding these, we can create strategies to lower their occurrence.
Maternal health is key in preventing these anomalies. Maternal smoking and lower socioeconomic status increase the risk. Good prenatal care and health education for expectant mothers can help reduce these risks.
Genetic counselling is vital for families with a history of these anomalies. It helps them understand their risks. Studies show that genetic counselling can greatly help manage pregnancies at risk for congenital anomalies.
Thanks to better ultrasound technology, we can detect these anomalies early. Early detection leads to better management and planning for surgery after birth. Regular prenatal check-ups are essential for early detection.
By tackling the risk factors of congenital gastrointestinal anomalies, we can lower their occurrence. This improves the outcomes for children affected by these conditions.
Recent studies show a drop in global cases and deaths from congenital GI issues. Between 1990 and 2021, cases fell by 8.15%, and deaths by 35.35%. This shows how better prenatal checks, new surgery methods, and improved care after surgery have helped.
We’ve looked at different GI problems in kids, like esophageal atresia and Hirschsprung’s disease. Knowing how these issues start, how they show up, and how to treat them is key. We need to keep studying and improving care to help more kids.
Looking ahead, we must focus on preventing these issues. This includes taking care of the mom and genetic testing for families at risk. With better prenatal care and surgery, we can make a big difference in the lives of kids with GI problems.
The main anomalies are esophageal atresia/tracheoesophageal fistula, duodenal atresia, anorectal malformations, and Hirschsprung’s disease.
Esophageal atresia means the esophagus didn’t fully develop. It might have a tracheoesophageal fistula, a bad connection between the esophagus and trachea.
The “double bubble” sign is seen in duodenal atresia. It shows two air-filled structures, the stomach and duodenum, showing duodenum blockage.
Anorectal malformations are sorted by where the rectal pouch is and its connection to the muscles. Different systems help guide treatment.
Hirschsprung’s disease is when the distal colon lacks ganglion cells, causing blockage. It’s diagnosed with a rectal biopsy.
Risk factors include maternal health, genetics, and environment. Genetic counselling is key for high-risk families.
Yes, some can be seen before birth with an ultrasound. This helps with planning for after birth.
Genetic counselling helps families understand risks and what it means. It aids in making informed choices.
Advances include better surgery, improved prenatal diagnosis, and postnatal care. This leads to better outcomes for kids.
GI malformations greatly affect global health, causing illness, death, and disability. More research and care are needed.
Down syndrome is linked to duodenal atresia. Children with Down syndrome are more likely to have it.
Symptoms include trouble feeding, regurgitation, and breathing issues. These often lead to early treatment.
Surgery for anorectal malformations involves several steps. First, a temporary fix is done, then a final repair and reconstruction.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!