Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, 12.8 million people worldwide need neurosurgery treatments. This is according to the Journal of Neurosurgery. It shows how important neurological surgery is for treating many nervous system conditions.
Neurosurgical procedures include many surgeries for the brain, spine, and spinal column. Looking into the most common neurosurgical procedures, we see how crucial they are. They greatly improve the lives of millions.
Key Takeaways
- Millions of people worldwide require neurosurgery treatments annually.
- Neurosurgery treats conditions related to the central and peripheral nervous system.
- Common neurosurgical procedures address various neurological conditions.
- Neurological surgery is crucial for treating brain, spine, and spinal column conditions.
- Understanding neurosurgical procedures can help patients make informed decisions.
The Field of Neurosurgery Explained
A neurosurgery specialist, dressed in a pristine white coat, stands before a detailed 3D brain model, intently studying the intricate neural pathways. The lighting is soft and directional, accentuating the focused expression on the specialist’s face and the subtle details of the brain model. The background is a clean, minimalist medical laboratory, with state-of-the-art equipment and instrumentation suggesting the advanced technology and precision required for neurosurgical procedures. The overall mood is one of quiet contemplation and professional expertise, reflecting the critical importance of the field of neurosurgery.
Neurosurgery is a specialized field that deals with complex conditions of the nervous system. It involves diagnosing and treating issues like brain tumors and spinal disorders. Neurosurgeons are experts in these areas, using advanced techniques to help patients.
Definition and Scope of Neurological Surgery
Neurological surgery, or neurosurgery, focuses on treating the nervous system. This includes the brain, spinal cord, and nerves. Neurosurgeons learn a lot about the nervous system and keep up with new surgical methods.
Neurosurgery covers many conditions, such as:
- Brain tumors and cysts
- Aneurysms and arteriovenous malformations (AVMs)
- Spinal disorders, including herniated discs and spinal stenosis
- Nerve compression syndromes, such as carpal tunnel syndrome
- Traumatic brain and spinal injuries
Evolution of Modern Neurosurgical Techniques
Modern neurosurgery has seen big changes thanks to new technology and techniques. Now, there are ways to do surgery that are less invasive and have better results. This means patients can recover faster and face fewer risks.
Some key advancements include:
- Minimally Invasive Surgery: Smaller incisions mean less damage and quicker healing.
- Endoscopic Surgery: Surgery through small openings, avoiding big cuts.
- Stereotactic Radiosurgery: A precise radiation therapy for brain tumors and abnormalities.
These new methods have made neurosurgery better and let doctors treat more conditions. As technology keeps improving, we can look forward to even better care for patients.
Common Neurosurgery: Procedure Statistics in the United States
A meticulously detailed medical infographic showcasing the most common neurosurgical procedures performed in the United States. The foreground features an array of anatomical diagrams and statistical charts, depicting the prevalence, success rates, and patient demographics for procedures like craniotomies, spinal fusions, and tumor resections. The middle ground presents a sleek, minimalist layout with clean typography and color-coded data visualizations. The background conveys a clinical atmosphere, with subtle medical equipment silhouettes and a muted palette of grays and blues, creating a sense of authoritative professionalism. The overall composition strikes a balance between informative clarity and visual sophistication, making it an ideal illustration for a comprehensive overview of neurosurgery trends and statistics.
In the United States, a lot of neurosurgical operations happen every year. These surgeries treat many brain and spine problems. They are key to healthcare, helping people with serious and long-lasting conditions.
Statistical Overview of Neurosurgical Operations
About 12.8 million people need neurosurgery treatments each year worldwide. A big part of these surgeries happen in the United States. The Journal of Neurosurgery says these operations include spinal surgeries, craniotomies, and shunt placements.
Some important stats on neurosurgery are:
- Spinal Surgeries: These are common. They treat problems like herniated discs and spinal stenosis.
- Craniotomies: These surgeries relieve brain pressure, remove tumors, or fix blood vessel issues.
- Shunt Placements: These are key for managing hydrocephalus, a fluid buildup in the brain.
Factors Influencing Procedure Frequency
Many things affect how often neurosurgery is done. These include:
- Demographic Changes: More older people and age-related conditions mean more need for surgery.
- Advancements in Surgical Techniques: New, less invasive surgeries and technology make more procedures possible and safer.
- Awareness and Diagnosis: Better diagnosis and public awareness lead to more cases needing surgery.
Knowing these stats and factors helps healthcare and policy makers. It helps them plan better and improve care. By looking at trends and what affects surgery rates, we can meet future needs and improve care quality.
Lumbar Discectomy: The Most Frequently Performed Neurosurgical Procedure
A highly detailed, photorealistic illustration of a lumbar discectomy surgical procedure. The scene depicts a human patient lying prone on an operating table, with the lower back exposed and the spinal column visible. In the foreground, a team of skilled neurosurgeons and medical staff are performing the delicate procedure, using precision instruments to carefully remove a damaged or herniated intervertebral disc from the lumbar region. The lighting is bright and clinical, casting crisp shadows that highlight the intricate details of the surgical instruments and the patient’s anatomy. The composition emphasizes the gravity and complexity of the procedure, conveying a sense of professionalism and technical expertise. The overall atmosphere is one of focused intensity, with the medical team working in seamless coordination to ensure the best possible outcome for the patient.
Lumbar discectomy is a top neurosurgical procedure. It helps those with herniated discs find relief. This surgery aims to ease pain and discomfort from a herniated disc in the lower back.
Understanding Herniated Discs and Their Symptoms
A herniated disc happens when the soft inner gel leaks out. This can irritate nerves, causing pain, numbness, and weakness in the back and legs. Symptoms depend on where and how bad the herniation is.
The Discectomy Procedure Step-by-Step
The lumbar discectomy procedure has several steps:
- Administering anesthesia to ensure patient comfort
- Making a small incision in the lower back to access the herniated disc
- Removing the herniated portion of the disc that is pressing on the nerve
- Closing the incision with sutures or staples
This minimally invasive method aims to cut down on recovery time and tissue damage.
Patient Selection and Success Rates
Not every patient with a herniated disc is right for lumbar discectomy. Doctors pick patients based on symptom severity, daily life impact, and failed conservative treatments. Research shows it works well for those who are chosen carefully.
We look at each patient’s situation to see if lumbar discectomy is the best option. We consider the surgical risks and benefits.
Spinal Surgeries: Leading the Neurosurgical Field
A detailed and lifelike surgical scene showing the intricate anatomy of the human spine during a complex operation. The image should depict the surgeon’s hands delicately manipulating the vertebrae, surrounded by state-of-the-art medical equipment and a sterile, well-lit operating theater. Subtle yet impactful lighting casts dramatic shadows, emphasizing the precision and intensity of the procedure. The overall atmosphere should convey a sense of focused professionalism and the critical importance of the neurosurgical task at hand.
Spinal surgeries, like spinal fusion and laminectomy, are very common. They help treat many spinal problems that cause a lot of pain and discomfort.
Spinal Fusion for Degenerative Conditions
Spinal fusion is a surgery that joins two or more vertebrae together. This helps stabilize the spine and reduce pain from degenerative conditions. These conditions include spondylolisthesis, degenerative disc disease, and spinal deformities.
We use the latest techniques and tools in spinal fusion to get better results. The surgery removes the damaged disc and replaces it with a bone graft. Then, rods, screws, or cages are used to stabilize it, helping the vertebrae to heal and fuse.
Benefits of Spinal Fusion:
- Significant pain reduction
- Improved spinal stability
- Enhanced quality of life
Laminectomy for Spinal Stenosis
Laminectomy is a surgery that relieves pressure on the spinal cord or nerves due to spinal stenosis. This condition narrows the spinal canal, causing pain, numbness, and weakness in the back and legs.
In a laminectomy, we remove part or all of the lamina to make more space for the nerves. This can greatly improve symptoms and mobility in patients with spinal stenosis.
Procedure | Condition Treated | Primary Benefit |
Spinal Fusion | Degenerative Conditions | Pain Reduction and Stability |
Laminectomy | Spinal Stenosis | Nerve Decompression |
Minimally Invasive Spine Surgery Advancements
Minimally invasive spine surgery has changed the field by reducing tissue damage and promoting faster recovery. Techniques like endoscopic discectomy and minimally invasive spinal fusion are becoming more popular.
These advancements let us do complex spinal procedures through smaller incisions. We use special instruments and imaging guidance. This leads to less postoperative pain and quicker recovery for patients.
Advantages of Minimally Invasive Spine Surgery:
- Smaller incisions
- Less tissue damage
- Faster recovery times
Craniotomy: Common Brain Surgery Procedure
a detailed and realistic medical illustration depicting a craniotomy procedure, the most common neurosurgical operation. in the foreground, a team of surgeons carefully operating on an open skull, using precision instruments to expose and access the brain. the middle ground shows an array of advanced medical equipment and monitors, providing critical data to the surgical team. the background depicts a sterile, well-lit operating theater, with bright lighting and a clean, clinical atmosphere. the overall scene conveys the gravity and complexity of the procedure, with a focus on the technical expertise and advanced technology involved in modern neurosurgery.
Craniotomy is a complex surgery where part of the skull is removed to access the brain. It’s key for treating serious conditions like brain tumors and aneurysms. We’ll look at why it’s done, the methods used, and how technology has made it better.
Indications for Craniotomy
Craniotomy is needed for several important reasons. It’s mainly used to remove brain tumors, fix aneurysms, and drain hematomas. It’s also used to ease pressure on the brain from trauma or swelling. Doctors decide on a craniotomy after detailed checks and scans.
The type of surgery depends on the brain issue. For example, the size and location of a tumor or an aneurysm affect the surgery plan.
Surgical Approach and Techniques
The surgery plan is made with great care to access the brain safely. Preoperative imaging helps pinpoint the best entry point. This ensures the surgery is effective and safe.
During surgery, we use advanced methods to navigate the brain. The bone flap is kept safe for later use. This is done under general anesthesia.
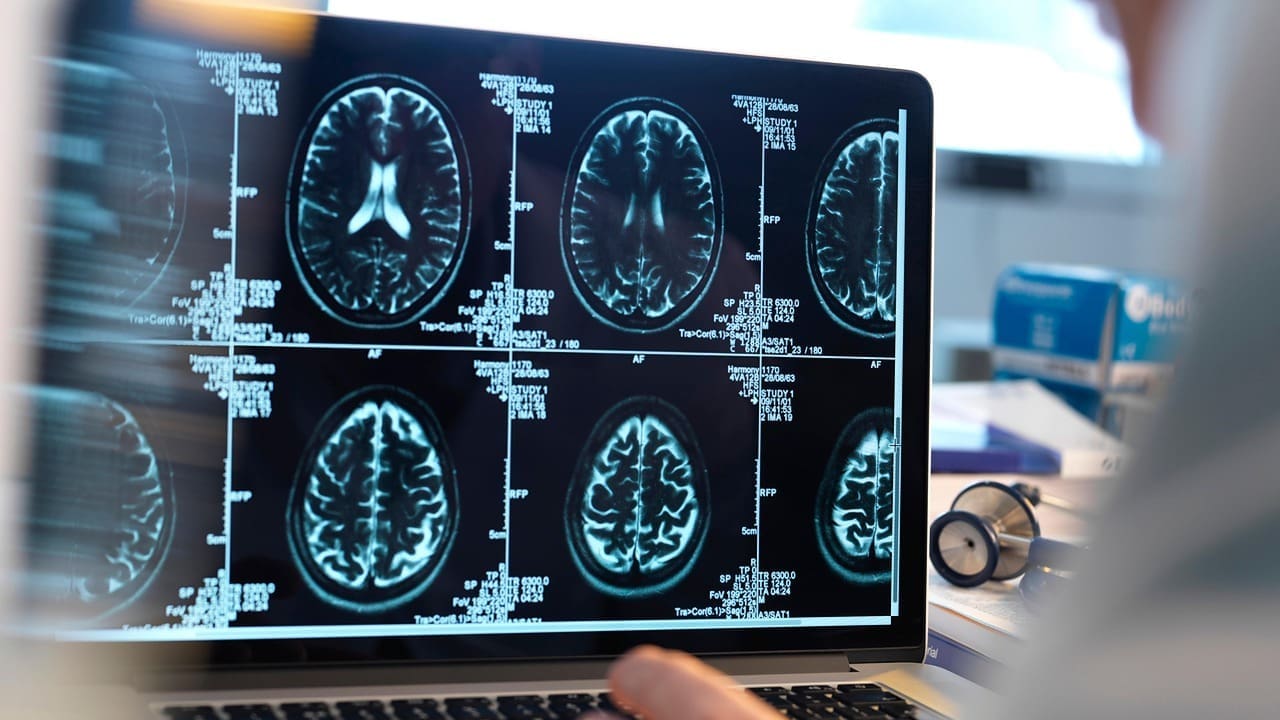
Technological Advancements in Cranial Surgery
New technologies have greatly improved craniotomy outcomes. Intraoperative MRI and navigation systems allow for real-time monitoring. This makes the surgery safer and more effective.
Minimally invasive and endoscopic methods are also used. They help reduce damage and speed up recovery. These advances have made craniotomy safer and more effective for patients.
In summary, craniotomy is a crucial surgery that has seen major improvements with technology. Knowing its purpose, the methods used, and how tech helps is key to understanding its benefits and complexities.
Brain Tumor Resection: Types and Approaches
A highly detailed medical illustration showcasing various surgical techniques for removing brain tumors. The foreground displays a series of delicate incisions and precise removal of the tumor mass, while the middle ground depicts the exposed brain anatomy, with intricate blood vessels and neural pathways. The background features a sterile operating room setting with advanced medical equipment, such as a high-powered microscope and specialized surgical tools. The lighting is bright and evenly distributed, creating a sense of clinical precision, and the camera angle is positioned to provide a clear, unobstructed view of the surgical procedure. The overall mood is one of medical expertise and scientific rigor, conveying the complexity and importance of this neurosurgical procedure.
Neurosurgeons use advanced methods to remove brain tumors. This improves patients’ lives and outcomes. Removing brain tumors is a key surgery that needs careful planning. It’s based on the tumor’s type, where it is, and the patient’s health.
Common Brain Tumors Requiring Surgical Intervention
Brain tumors can be either benign or cancerous. Surgery is chosen based on the tumor’s size, location, and type. Common types needing surgery include:
- Meningiomas
- Glioma
- Acoustic neuromas
- Metastatic brain tumors
Each tumor type poses unique challenges for neurosurgeons. They must plan and execute the surgery carefully.
Surgical Techniques for Tumor Removal
Removing brain tumors involves different methods. These range from traditional surgery to newer, less invasive options. Several factors decide the surgical method:
- Tumor location and size
- How close it is to important brain parts
- The patient’s health and past medical history
Neurosurgeons use high-tech imaging and monitoring during surgery. This ensures safe and effective tumor removal.
Awake Craniotomy for Eloquent Area Tumors
For tumors in areas controlling important functions, an awake craniotomy is used. This lets the surgeon watch the patient’s brain function during surgery. It helps avoid damage to key brain areas.
The awake craniotomy’s benefits are:
- Lower risk of brain damage
- More accurate tumor removal
- Shorter recovery times
This advanced technique helps neurosurgeons achieve better results for patients with tumors in sensitive areas.
Cerebrovascular Neurosurgery: Aneurysm and AVM Treatment
A high-quality, detailed surgical scene depicting cerebrovascular neurosurgery, showcasing the intricate procedure of treating an aneurysm or arteriovenous malformation (AVM). Set in a well-lit operating room, with a skilled neurosurgeon and their team performing delicate manipulations on the patient’s exposed brain. Observe the precision of the instruments, the focus of the medical professionals, and the complex web of blood vessels and neural structures that require careful navigation. Convey a sense of critical importance and technical expertise, with a somber, concentrated atmosphere befitting the gravity of the situation. Realistic, photorealistic rendering with accurate anatomical details and subtle lighting to highlight the complexity of the procedure.
Advances in cerebrovascular neurosurgery have greatly improved treatment for aneurysms and AVMs. This field focuses on brain vascular disorders. We’ll look at treatments like surgery and endovascular methods.
Surgical Clipping of Cerebral Aneurysms
Surgical clipping is a key method for treating cerebral aneurysms. It involves craniotomy to reach the aneurysm. Then, a clip is placed to block blood flow to the aneurysm.
This method aims to stop the aneurysm from rupturing again. New clipping techniques use intraoperative angiography for better results.
Endovascular Coiling Procedures
Endovascular coiling is a less invasive option for aneurysm treatment. It uses a catheter to place coils in the aneurysm. This promotes clotting and blocks blood flow.
Advancements in coil technology have made this procedure safer and more effective.
AVM Resection and Embolization Techniques
AVM treatment often combines surgery and endovascular embolization. Embolization reduces blood flow to the AVM, making surgery safer. We use advanced imaging techniques to plan the best treatment.
Surgical removal of the AVM follows. The goal is to cure the condition.
In conclusion, cerebrovascular neurosurgery offers effective treatments for aneurysms and AVMs. Understanding these options helps patients make informed decisions about their care.
Shunt Placement for Hydrocephalus
Hydrocephalus often needs a shunt to drain extra cerebrospinal fluid from the brain. This condition can come from many causes, like being born with it, infections, or tumors.
Understanding Hydrocephalus Pathophysiology
Hydrocephalus happens when the brain makes too much cerebrospinal fluid and can’t get rid of it. This leads to fluid building up in the brain’s ventricles. If not treated, it can cause brain damage.
We find out if someone has hydrocephalus by looking at their symptoms, doing MRI or CT scans, and sometimes a lumbar puncture. Knowing why it happens helps us choose the right treatment.
Types of Shunt Systems and Selection
There are different shunt systems for different needs. The most used is the ventriculoperitoneal (VP) shunt. It moves CSF from the brain to the belly.
Shunt Type | Description | Indications |
Ventriculoperitoneal (VP) Shunt | Diverts CSF to the peritoneal cavity | Most common type, suitable for many hydrocephalus cases |
Ventriculoatrial (VA) Shunt | Diverts CSF to the right atrium of the heart | Used when peritoneal cavity is not suitable |
Lumboperitoneal (LP) Shunt | Diverts CSF from the lumbar subarachnoid space to the peritoneal cavity | Used for communicating hydrocephalus or pseudotumor cerebri |
Surgical Procedure and Long-term Management
To put in a shunt, a small cut is made in the scalp. Then, a hole is made in the skull, and the shunt is placed in the brain. The other end goes under the skin to the drainage site.
After surgery, regular check-ups are needed to make sure the shunt is working right. Patients and their families learn what to watch for if the shunt stops working or gets infected. They need to see a doctor right away.
It’s key to keep up with care and watch for any problems. This helps patients with hydrocephalus live better lives.
Neurosurgery for Trauma Cases
Neurosurgery is key in managing trauma cases. Specialists perform critical procedures under pressure. They address complex injuries from traumatic events, needing great skill and precision.
Emergency Decompressive Craniectomy
Emergency decompressive craniectomy is a lifesaving surgery. It relieves brain pressure from swelling or bleeding. By removing part of the skull, it lets the brain expand, lowering pressure.
This surgery is urgent when patients show signs of high brain pressure. These signs include decreased consciousness or neurological problems. The surgery is often done with other treatments to manage the patient’s condition.
Evacuation of Intracranial Hematomas
Intracranial hematomas are blood clots in the skull from head trauma. Removing these clots is crucial to reduce brain pressure. We use advanced imaging to find and remove the clots effectively.
Quickly removing these clots is vital. It prevents further brain damage from the clot’s pressure. Our aim is to restore brain function by relieving pressure and ensuring blood flow.
Skull Fracture Repair Techniques
Skull fractures are common in trauma cases. They range from simple to complex. Repairing these fractures is essential to protect the brain and prevent complications.
We use plates, screws, and other devices to fix fractures. In severe cases, cranioplasty may be needed to rebuild the skull.
Peripheral Nerve Surgery: Addressing Nerve Compression
Peripheral nerve surgery helps fix nerve problems by relieving pressure. This pressure can come from tissue or injury, causing pain, numbness, and weakness. We’ll look at how to treat these issues through surgery, focusing on carpal tunnel release, ulnar nerve decompression, and fixing nerve injuries.
Carpal Tunnel Release Procedure
Carpal tunnel syndrome happens when the median nerve gets squeezed at the wrist. The surgery to fix this involves cutting the transverse carpal ligament. This lets the median nerve breathe and relieves pressure. The surgery can be done in two ways: open or endoscopic. The endoscopic method is better because it uses smaller cuts and might heal faster.
Benefits of Carpal Tunnel Release:
- Significant pain relief
- Improved hand function
- Minimally invasive options available
Ulnar Nerve Decompression at the Elbow
Ulnar nerve compression at the elbow is called cubital tunnel syndrome. It can make your hand numb, tingle, and weak. The surgery to fix this involves cutting the nerve free from tight spots around the elbow. There are a few ways to do this, like simple cuts, removing part of the bone, or moving the nerve.
Surgical Technique | Description | Advantages |
Simple Decompression | Releasing compressive structures | Less invasive, quicker recovery |
Medial Epicondylectomy | Removing part of the medial epicondyle | Reduces nerve irritation |
Ulnar Nerve Transposition | Relocating the ulnar nerve | Effective for severe compression |
Surgical Management of Traumatic Nerve Injuries
Traumatic nerve injuries need quick and often surgical treatment to fix nerve function. Doctors might repair the nerve, use a graft, or transfer the nerve. The choice depends on the injury’s type and how bad it is.
We’ve talked about the different parts of peripheral nerve surgery. It’s key in treating nerve compression problems. Knowing the surgical options helps both patients and doctors make the best choice for treatment.
Minimally Invasive Neurosurgery: Growing Trends
Minimally invasive neurosurgery is changing how we treat complex brain conditions. New technologies like endoscopic surgery and Laser Interstitial Thermal Therapy (LITT) are becoming more common. They offer patients less invasive options with fewer risks.
Endoscopic Techniques in Cranial and Spinal Surgery
Endoscopic techniques have made neurosurgery better. They allow for minimally invasive procedures that cause less damage and help patients recover faster. In brain surgery, endoscopy helps surgeons be more precise. In spinal surgery, it treats problems like herniated discs with less harm to other tissues.
A recent study found that “Endoscopic surgery is a valuable tool in neurosurgery. It reduces pain and shortens hospital stays,” (Source: Journal of Neurosurgery). This shows a trend in neurosurgery towards less invasive methods. The goal is to get the best results with less discomfort and quicker recovery.
Laser Interstitial Thermal Therapy (LITT)
LITT is a new technique in neurosurgery. It uses laser energy to kill targeted tissue, like brain tumors, while keeping healthy tissue safe. It’s great for tumors in hard-to-reach brain areas, where traditional surgery is risky.
- LITT allows for real-time temperature control, making it safer and more precise.
- It can be done under MRI, helping target the tumor accurately.
- LITT leads to shorter recovery times than traditional surgery.
Benefits and Limitations of Minimally Invasive Approaches
Minimally invasive neurosurgery has many benefits. It causes less harm to patients, less pain after surgery, and faster recovery. But, there are also challenges. Surgeons need to learn new skills, and the equipment is specialized. Sometimes, it’s hard to see or reach certain areas.
As neurosurgery advances, minimally invasive techniques will be more important. Knowing their benefits and limits helps us better care for our patients. We can offer them the best treatment options available.
Age-Related Factors in Neurosurgical Procedures
Age is very important in neurosurgery. It changes how we approach and treat patients, from kids to seniors. Knowing how age impacts these procedures is key.
Pediatric Neurosurgery: Common Procedures
Pediatric neurosurgery deals with many issues in children. These include:
- Craniosynostosis repair: Surgery to fix early skull bone fusion.
- Hydrocephalus treatment: Using shunts or endoscopic third ventriculostomy to manage fluid buildup.
- Spinal deformity correction: Surgery for scoliosis or spina bifida.
These surgeries need special care because of the child’s growing body and brain.
Geriatric Considerations in Neurosurgery
Older patients face special challenges in neurosurgery. These include:
- Comorbidity management: Managing conditions like high blood pressure and diabetes.
- Polypharmacy: Watching how many medicines they take to avoid bad reactions.
- Cognitive and functional status: Checking how well they think and function before surgery.
By focusing on these areas, we can help older patients do better after surgery.
Age-Specific Surgical Risks and Outcomes
Risks and results change with age. Here’s a table showing some key differences:
Age Group | Common Risks | Outcome Considerations |
Pediatric | Anesthesia risks, developmental impacts | Long-term follow-up, growth and development monitoring |
Adult | Surgical site infection, neurological deficits | Return to baseline function, pain management |
Geriatric | Comorbidity exacerbation, cognitive decline | Rehabilitation needs, potential for extended recovery |
Knowing these age-specific factors helps us tailor care for each patient. This way, we can improve their outcomes.
Risks and Complications of Neurosurgical Procedures
Neurosurgical procedures are lifesaving but come with risks. These risks include general surgical risks and procedure-specific complications. Neurosurgeons manage these risks carefully.
General Surgical Risks in Neurosurgery
General risks in neurosurgery include infection, bleeding, and reactions to anesthesia. We reduce these risks through preoperative screening and sterile techniques. Postoperative care is also crucial.
For example, antibiotics prevent surgical site infections. Managing bleeding risks is also key. We use hemostatic agents and precise surgical techniques to minimize bleeding.
Procedure-Specific Complications
Each neurosurgical procedure has its own risks. Craniotomies can lead to cerebral edema or brain injury. Spinal surgeries may cause nerve damage or instability.
Procedure | Common Complications | Mitigation Strategies |
Craniotomy | Cerebral edema, infection | Corticosteroids, meticulous wound closure |
Spinal Fusion | Nerve damage, hardware failure | Intraoperative neuromonitoring, robust hardware |
Lumbar Discectomy | Recurrent herniation, nerve root injury | Minimally invasive techniques, careful patient selection |
Risk Mitigation Strategies and Patient Selection
Reducing risks starts with choosing the right patients. We assess their health, condition severity, and surgery benefits. Advanced diagnostics help us understand risks better.
“The key to successful neurosurgery lies not just in the technical skill of the surgeon, but in the judicious selection of patients and the careful management of risks.” –
A renowned neurosurgeon
We use minimally invasive techniques and intraoperative monitoring. Enhanced recovery after surgery (ERAS) protocols also help. These strategies lower complication risks and improve outcomes.
In conclusion, neurosurgical procedures have inherent risks. Understanding these risks and using effective strategies can improve patient outcomes. As neurosurgeons, we aim to provide the best care, balancing surgery benefits and risks.
Recovery and Rehabilitation After Neurosurgery
Neurosurgery needs careful care after the surgery. This includes recovery and rehab to get the best results. The recovery time changes based on the surgery type.
Typical Recovery Timelines by Procedure Type
Each neurosurgery has its own recovery time. For example, lumbar discectomy patients usually recover faster than those who had a craniotomy. We’ll explain the typical recovery times for different surgeries to help patients know what to expect.
Lumbar Discectomy: Most people can go back to normal in 2-6 weeks. But, it can take up to 3 months to fully recover.
Craniotomy: Craniotomy recovery can take 6-12 weeks. Some might need even more time to get back to normal.
Physical Therapy and Rehabilitation Programs
Physical therapy is key in rehab after neurosurgery. Custom rehab plans help patients get stronger and move better. We team up with physical therapists to make plans that fit each patient’s needs.
- Early mobilization to prevent complications
- Strengthening exercises to improve muscle tone
- Flexibility and range-of-motion exercises to enhance mobility
Long-term Outcomes and Quality of Life Measures
It’s important to check how patients do long-term after surgery. We look at pain, function, and how happy patients are. This helps us see if the surgery was a success.
Quality of life measures look at physical, emotional, and social health. These help us see how surgery affects patients’ lives. They guide us in making treatment plans better.
By focusing on full recovery and rehab, we can make patients’ lives better. This improves their quality of life.
Choosing a Neurosurgery Specialist: Important Considerations
Choosing a neurosurgery specialist is a big decision. It involves looking at qualifications, hospital resources, and how well the surgeon communicates with patients. It’s key to pick a specialist who is skilled, experienced, and works in a modern hospital.
Qualifications, Experience, and Expertise
A neurosurgery specialist’s qualifications are key to their care quality. We look for those who are board-certified and have had thorough training. Their experience matters too, showing they can handle complex cases.
Key Qualifications to Look For:
- Board certification in neurosurgery
- Completion of a neurosurgery residency program
- Additional fellowship training in a subspecialty (if relevant)
- Active involvement in neurosurgical research or education
It’s also important to check if the specialist has experience in your specific needs. For example, some specialize in spinal surgery or brain tumors. Having the right experience can greatly improve your results.
Hospital Resources and Technological Capabilities
The hospital where your specialist works is crucial. We look for hospitals with the latest neurosurgical technology. This technology helps make surgeries safer and more precise.
Technological Capability | Description | Benefit |
Intraoperative MRI | Allows for real-time imaging during surgery | Enhanced precision and safety |
Neuro-navigation Systems | Provides detailed navigation through the brain or spine | Improved accuracy in complex procedures |
Advanced Monitoring Systems | Monitors vital signs and neurological function in real-time | Better management of potential complications |
Patient-Surgeon Communication and Relationship
Good communication between patient and surgeon is essential. We look for specialists who explain things clearly. A strong relationship built on trust and understanding makes recovery better.
“A good neurosurgeon doesn’t just operate on the brain or spine; they also operate on the patient’s concerns and fears.” This shows how important empathy and clear communication are in neurosurgery.
When choosing a neurosurgery specialist, think about their communication style. Look for someone who listens and answers your questions.
Conclusion: The Future of Neurosurgical Procedures
Neurosurgical procedures are always getting better, thanks to new techniques and technology. The future looks bright for neurosurgery, with procedures like lumbar discectomy and spinal fusion getting more precise.
New methods like minimally invasive and endoscopic procedures are making a big difference. They help patients heal faster and with less pain. Also, technology like laser interstitial thermal therapy is opening up new ways to treat tough neurological problems.
We can look forward to even better treatments for brain tumors and spinal issues. Keeping up with the latest in neurosurgery helps both patients and doctors. This way, everyone can get the best care possible.
FAQ
What is the most common type of neurosurgery?
Lumbar discectomy is a common neurosurgery. It treats herniated discs and relieves back pain and nerve compression.
What is neurosurgery and what conditions does it treat?
Neurosurgery treats the brain and spine. It addresses spinal stenosis, brain tumors, aneurysms, and traumatic injuries.
What is a craniotomy procedure?
A craniotomy removes part of the skull to access the brain. It treats life-threatening conditions like brain tumors and aneurysms.
What is the difference between spinal fusion and laminectomy?
Spinal fusion joins vertebrae to stabilize the spine. It treats degenerative conditions. Laminectomy removes vertebra parts to relieve pressure on nerves.
What are the risks associated with neurosurgical procedures?
Neurosurgery risks include infection, bleeding, and anesthesia reactions. Each procedure has its own risks, making careful planning crucial.
What is minimally invasive neurosurgery?
Minimally invasive neurosurgery uses advanced techniques for smaller incisions. It aims to reduce recovery time and scarring.
How do I choose a neurosurgery specialist?
Choose a specialist based on their qualifications and experience. Consider the hospital’s resources and the importance of good communication.
What is the recovery process like after neurosurgery?
Recovery times vary by procedure. Some need physical therapy, while others require ongoing care.
What are the benefits of shunt placement for hydrocephalus?
Shunt placement relieves brain pressure from hydrocephalus. It improves symptoms and quality of life, needing ongoing management.
What is the role of neurosurgery in trauma cases?
Neurosurgery treats traumatic brain and spinal injuries. Emergency procedures like decompressive craniectomy save lives and prevent damage.
What are the age-related factors that influence neurosurgical procedures?
Age affects neurosurgical outcomes. Pediatric and geriatric patients need specialized care, highlighting the need for tailored treatment.
What is awake craniotomy and when is it used?
Awake craniotomy removes brain tumors in critical areas. The patient is awake to help preserve brain function.
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/neurosurgery