Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know some substances in blood, urine, or tissues can show cancer? These are called tumor markers”proteins or molecules made by cancer cells or produced by the body in response to cancer. Understanding the role of Common Tumor Markers in Cancer Diagnosis is vital for early detection and ongoing monitoring.PSA (prostate-specific antigen) is a key marker for prostate cancer. CEA (carcinoembryonic antigen) and CA-125 are linked to colorectal and ovarian cancers. By learning about the Common Tumor Markers in Cancer Diagnosis, patients and doctors can work together for earlier detection, better monitoring, and more effective treatment planning.
Key Takeaways
- Tumor markers are substances found in higher amounts in people with certain types of cancer.
- PSA, CEA, and CA-125 are three common cancer diagnostic markers.
- These markers help in diagnosing and monitoring cancer progression.
- Understanding tumor markers is essential for early cancer detection and treatment.
- Cancer biomarkers play a critical role in cancer diagnosis and management.
Understanding Tumor Markers in Cancer Detection
Tumor markers are key in finding and managing cancer. They show if cancer is present and how it’s growing. These markers are made by tumors or by the body’s reaction to them. They can be found in blood, urine, or tissues of people with some cancers.
Definition and Basic Concepts
Tumor markers are biological molecules made by cancer cells or the body’s reaction to them. They can be proteins, enzymes, hormones, or genetic material. If these markers are present in high amounts, it might mean cancer is there. They can also tell us about the cancer’s growth or how likely it is to come back.
We use tumor markers for many things. For example, they help in screening, diagnosing, predicting how the cancer will grow, and checking if treatment is working. Some markers help us see if a patient is getting better or if the cancer might come back.
Role in Modern Oncology
In today’s oncology, tumor markers are indispensable tools for doctors. They help find cancer early, which means we can test patients who might need more tests. They also help track how the disease is growing and how well it’s responding to treatment. This helps doctors make better choices for their patients.
We count on tumor markers to help decide on treatments, watch for cancer coming back, and screen for cancer in people at high risk. Thanks to tumor markers, we can treat cancer more effectively and personally.
The Science Behind Tumor Markers
Tumor markers are key in changing how we diagnose and treat cancer. They are substances found in higher amounts in the blood, urine, or tissues of cancer patients. Knowing where they come from and how they are classified helps us see their importance in fighting cancer.
Biological Origin of Tumor Markers
Tumor markers can come from cancer cells or the body’s reaction to them. Cancer cells make these markers because of their changed genes. This leads to proteins or molecules not found in normal cells or in much smaller amounts.
For example, some proteins are made too much or change in cancer cells. These proteins can show that cancer is present.
The body’s fight against cancer also creates tumor markers. Inflammation and immune responses caused by cancer cells release substances into the blood or other fluids. These substances can indicate cancer or help track how it’s growing.
Classification of Cancer Biomarkers
Cancer biomarkers, like tumor markers, are sorted by their structure and function. Proteomic biomarkers are proteins or peptides linked to cancer. These include enzymes, receptors, or proteins that are made too much or change in cancer cells.
Other biomarkers might be based on genetic material, like DNA or RNA, that changes in cancer cells. The way we sort tumor markers is not just about their chemical makeup. It’s also about how useful they are in the clinic.
Prognostic markers tell us about the disease’s likely outcome. Predictive markers help us guess how well a treatment will work. Knowing these types is key to using tumor markers well in medical care.
Common Tumor Markers in Cancer Diagnosis
Tumor markers are key in finding and tracking cancer. They are made by tumors or in response to them. Finding these markers helps doctors diagnose, monitor, and catch cancer’s return.
Overview of Widely Used Tumor Markers
Many tumor markers are used in cancer care. Here are some well-known ones:
- PSA (Prostate-Specific Antigen) for prostate cancer
- CEA (Carcinoembryonic Antigen) for colorectal cancer
- CA-125 for ovarian cancer
- AFP (Alpha-Fetoprotein) for liver cancer
- CA19-9 for pancreatic cancer
These markers help in different ways, like screening and tracking treatment.
| Tumor Marker | Associated Cancer | Primary Use |
| PSA | Prostate Cancer | Screening, Monitoring |
| CEA | Colorectal Cancer | Monitoring, Recurrence Detection |
| CA-125 | Ovarian Cancer | Monitoring, Diagnosis Support |
| AFP | Liver Cancer | Screening, Diagnosis |
| CA19-9 | Pancreatic Cancer | Monitoring, Diagnosis Support |
Selection Criteria for Clinical Use
Choosing tumor markers for use in clinics is based on several things. These include the cancer type, how well the marker works, and its usefulness in care. A good marker should be very sensitive and specific for the cancer it’s meant to find.
Here’s what we look at when picking tumor markers:
- Sensitivity: How well the marker finds people with the disease.
- Specificity: How well the marker finds people without the disease.
- Clinical Utility: How the marker affects patient care and results.
By looking at these points, doctors can use tumor markers well in cancer care.
PSA (Prostate-Specific Antigen): A Critical Prostate Cancer Marker
PSA is key in fighting prostate cancer. It’s a protein made by the prostate gland. High levels might mean cancer, but not always.
Clinical Significance and Reference Ranges
PSA helps find prostate cancer early. Normal levels are between 0 to 4 ng/mL. But, this can change based on the lab.
Knowing PSA ranges is very important. A man’s age, race, and more can affect what’s normal.
Limitations and Controversies
PSA testing has its downsides. It can cause worry and unnecessary tests if it’s wrong. It can also be high when there’s no cancer, like in prostatitis or BPH.
“The use of PSA testing for prostate cancer screening has been a subject of debate, with some arguing it leads to overdiagnosis and overtreatment.”
Recent Advances in PSA Testing
New methods aim to make PSA testing better. The PSA velocity and free PSA percentage help tell if it’s cancer or not.
These new ways have made PSA testing more useful. Scientists keep working to make it even better, maybe for each person’s needs.
CEA (Carcinoembryonic Antigen): Monitoring Colorectal Cancer
Carcinoembryonic antigen, or CEA, is a protein used to track colorectal cancer. It’s important in clinical practice. We’ll look at its discovery, role, and use in tracking cancer.
Discovery and Biological Function
CEA was founded in 1965 by Gold and Freedman. It’s found in embryonic cells and colon cancer cells. High levels of CEA are linked to many cancers, mainly colorectal cancer.
CEA is not specific to cancer. It can also rise in inflammatory bowel disease and some benign conditions. Yet, in colorectal cancer, it’s a key tool for tracking the disease and treatment success.
Clinical Applications in Colorectal Cancer
In clinical settings, CEA helps monitor colorectal cancer patients. Increasing CEA levels after surgery may mean the cancer has come back. Falling levels during treatment suggest the cancer is responding well. We combine CEA tests with imaging and clinical checks.
Guidelines support using CEA to watch for cancer return and treatment success. But, we must consider each patient’s situation when looking at CEA levels.
CEA in Other Malignancies
CEA is also linked to cancers like breast, lung, and pancreatic. Its role in these cancers is not as clear as in colorectal cancer. Yet, it can offer useful insights in some cases.
In summary, CEA is a key marker for colorectal cancer. It helps track the disease and how well treatments work. We keep improving how we use CEA to help patients.
CA-125: The Primary Ovarian Cancer Biomarker
The CA-125 tumor marker is key in checking on ovarian cancer patients. It’s a protein that often goes up in ovarian cancer. We use it to see how well treatment is working and if the cancer comes back. Let’s look at how we find it, what normal levels are, and the tricky parts of understanding its results.
Detection Methods and Normal Values
We find CA-125 levels in blood tests. These tests look for the CA-125 protein in your blood. The most common test is the electrochemiluminescence immunoassay (ECLIA). Normal levels are usually below 35 U/mL, but can change a bit between labs.
Detection Techniques:
- Electrochemiluminescence immunoassay (ECLIA)
- Radioimmunoassay (RIA)
- Enzyme-linked immunosorbent assay (ELISA)
Interpretation Challenges in Clinical Settings
Understanding CA-125 levels can be tricky. It can go up in many non-cancer conditions like endometriosis, pregnancy, and pelvic inflammatory disease. So, we look at the whole picture of the patient when we check CA-125 levels.
Factors Affecting CA-125 Levels:
- Benign gynecological conditions
- Pregnancy
- Menstruation
- Pelvic inflammatory disease
CA-125 in Treatment Monitoring
CA-125 is great for watching how ovarian cancer responds to treatment. If CA-125 goes down, it means treatment is working well. But if it goes up, it might mean the cancer is coming back or not responding to treatment. We use CA-125 to help decide on treatment and see if it’s working.
Clinical Utility:
- Monitoring treatment response
- Detecting recurrence
- Assessing prognosis
Additional Significant Tumor Markers
There are many tumor markers beyond the well-known ones. These markers are key in finding and tracking cancer. They help doctors spot cancer early and check how well treatments are working.
AFP (Alpha-Fetoprotein) in Liver Cancer
Alpha-Fetoprotein (AFP) is a protein found in the blood of people with liver cancer and some germ cell tumors. AFP testing is very helpful for watching over people at risk for liver cancer. This includes those with chronic hepatitis B or C, or cirrhosis.
“High AFP levels can mean liver cancer is present,” doctors say. But not all liver cancers have high AFP, and not all high AFP means cancer. So, AFP is used with other tests to make sure of a diagnosis.
CA19-9 for Pancreatic Cancer Detection
CA19-9 is a sugar antigen used for pancreatic cancer. It’s not just for pancreatic cancer, but it’s useful for tracking the disease’s growth and treatment success.
CA19-9 levels change based on the tumor and the patient’s health. It’s important to look at these levels with other test results. Studies show CA19-9 can help predict how well a patient will do and guide treatment in pancreatic cancer.
HCG in Testicular and Gestational Tumors
Human Chorionic Gonadotropin (HCG) is a hormone seen in pregnancy, but it’s also in some tumors. This includes testicular cancer and gestational trophoblastic disease. HCG is key for diagnosing and tracking these conditions.
In testicular cancer, HCG is used with AFP to help diagnose and check treatment success. For gestational trophoblastic disease, HCG levels are vital for diagnosis, risk assessment, and treatment monitoring.
In summary, markers like AFP, CA19-9, and HCG are important in cancer diagnosis and care. Knowing their roles and limits helps doctors make better decisions for their patients.
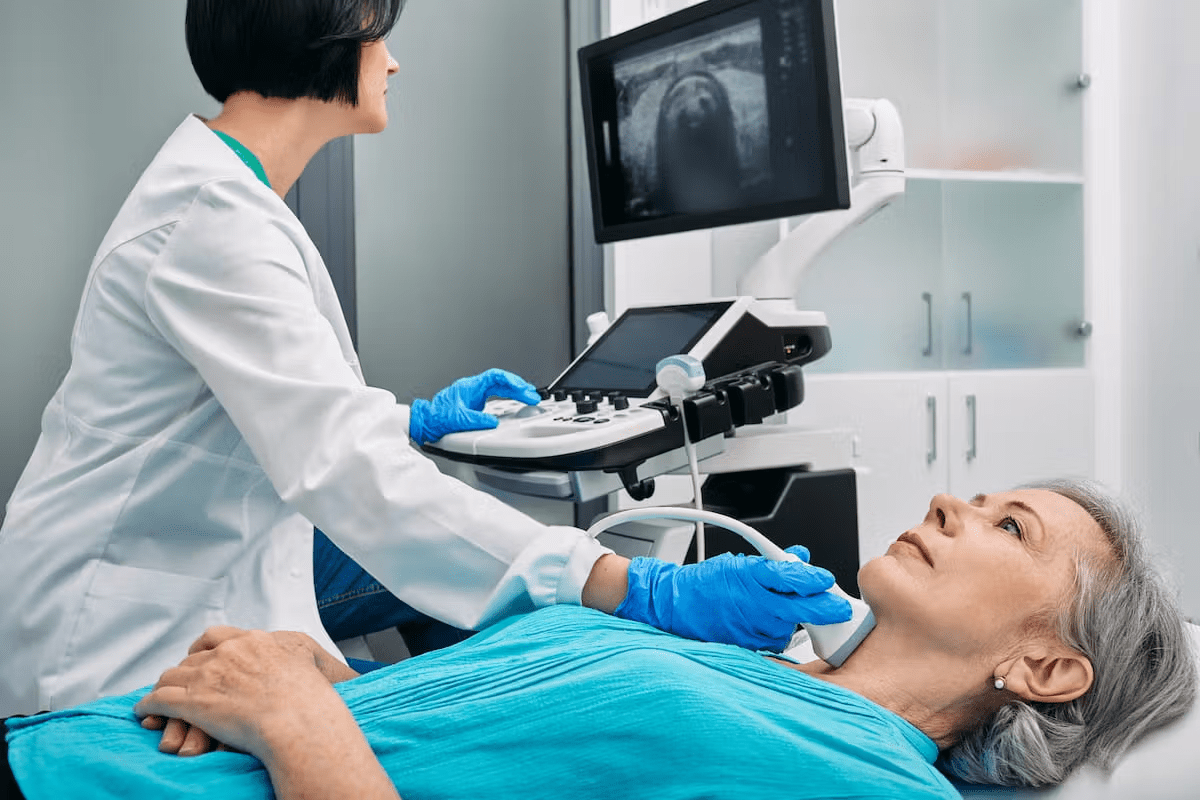
Tumor Marker Testing Methodologies
Finding tumor markers is a detailed process with different methods. Each method has its own benefits and drawbacks. These markers can be found in blood and tissues, helping doctors diagnose and track cancer.
Blood-Based Detection Techniques
Testing for tumor markers in blood is common because it’s easy and affordable. Here are some ways to do it:
- Immunoassays: Use antibodies to spot specific markers in blood.
- Molecular Tests: Look for cancer genes with PCR.
- Protein Biomarker Detection: Find and measure protein markers with mass spectrometry.
These tests are key for tracking cancer and seeing how well treatments work. For example, PSA testing for prostate cancer and CA-125 testing for ovarian cancer are well-known.
Tissue Sample Analysis
Looking at tissue samples from biopsies or surgeries helps find tumor markers. This method gives clear signs of cancer and insights into its nature.
- Immunohistochemistry (IHC): Uses antibodies to find proteins in tissues, spotting markers.
- Fluorescence In Situ Hybridization (FISH): Sees genetic changes in tissues.
- Molecular Pathology: Checks tissues for genetic changes to guide treatments.
Tissue analysis is great for diagnosing and understanding cancer types. It also helps find new treatments.
By mixing blood tests with tissue analysis, doctors get a full picture of a patient’s cancer. This helps create treatment plans that fit each person’s needs.
Interpreting Tumor Marker Results
Understanding tumor marker results is complex. It involves knowing reference ranges and other key factors. When we look at these results, we must think about several things that can change the test’s accuracy.
Understanding Reference Ranges
Reference ranges for tumor markers are based on what’s normal in healthy people. These ranges help us see if a marker is too high, which might mean cancer or another issue. It’s important to know that these ranges can differ between labs because of how they test and handle samples.
For example, the normal range for Prostate-Specific Antigen (PSA) is usually up to 4 ng/mL. But, this can vary a bit between labs. Knowing these ranges helps us understand test results better and make good decisions about what to do next.
| Tumor Marker | Typical Reference Range |
| PSA | 0-4 ng/mL |
| CEA | 0-5 ng/mL |
| CA-125 | 0-35 U/mL |
Factors Affecting Test Results
Many things can change tumor marker test results, making them hard to understand. We have to think about lab differences, patient health, and other possible errors when we look at these results.
- Laboratory Variability: Different labs use different tests, which can cause different results.
- Patient Conditions: Some health issues, like liver disease, can change marker levels.
- Specimen Handling: How samples are collected, stored, and sent can also affect results.
When to Retest and Follow Up
Retesting and follow-up are very important in tumor marker testing. We suggest retesting if the first results are abnormal or if symptoms don’t go away even with normal results. When to retest depends on the marker and the situation.
For example, with PSA tests for prostate cancer, we often recommend retesting a few weeks later. This helps confirm the results and rule out false positives.
By knowing reference ranges, considering how test results can be affected, and knowing when to retest, we can understand tumor marker results well. This helps us give our patients the best care possible.
Clinical Applications of Tumor Markers
We use tumor markers in many ways to fight cancer. They help us find and treat cancer better. These markers are used for screening, diagnosis confirmation, treatment monitoring, and spotting recurrence.
Screening and Early Detection
Tumor markers are key in finding cancer early. For example, the PSA test helps find prostate cancer. It catches the disease when it’s easier to treat.
CA-125 is another marker for ovarian cancer. It’s not a sure sign, but high levels mean more tests are needed.
Diagnosis Confirmation
Tumor markers also help confirm cancer diagnoses. Alpha-fetoprotein (AFP) in adults can mean liver cancer or germ cell tumors. AFP tests, along with imaging and doctor’s checks, help diagnose and plan treatment.
Human chorionic gonadotropin (hCG) is used for testicular cancer and gestational trophoblastic disease. It shows if these conditions are present and how they’re responding to treatment.
Treatment Monitoring and Recurrence Detection
Tumor markers are also key in checking how well treatment is working. If a marker’s levels go down, it’s a good sign. But if they stay the same or go up, treatment might not be working.
They also help find cancer that comes back. Watching marker levels can catch recurrence early. For example, rising CEA levels in colorectal cancer patients mean it might be coming back, so more tests and treatments are needed.
In short, tumor markers are very important in cancer care. They help us screen, diagnose, treat, and follow up. Their use greatly improves how we manage cancer, helping patients get better.
Limitations and Challenges of Tumor Marker Testing
Tumor marker testing has its benefits but also faces several challenges. We use these tests to help diagnose, monitor, and treat cancer. It’s important to know their limitations to make smart choices.
False Positives and Negatives
One big issue with tumor marker testing is getting false positives and negatives. A false positive can cause unnecessary worry and extra tests. A false negative might make us think everything is okay when it’s not.
Several things can lead to these false results:
- Laboratory errors
- Different testing methods
- Non-cancer conditions that change marker levels
Non-Cancer Conditions Affecting Marker Levels
Non-cancer conditions can also change tumor marker levels. For example:
- Inflammatory diseases can raise some markers
- Problems with the liver or kidneys can affect marker levels
- Benign tumors or cysts can also raise markers
It’s key to understand these factors for accurate results. We need to look at the whole clinical picture, including medical history and other tests, to make good decisions.
Knowing the limits of tumor marker testing helps us use them better in cancer care. It’s vital to stay informed and work with healthcare providers to understand test results.
Emerging Tumor Markers and Research Directions
The world of cancer diagnosis is changing fast. New tumor markers are being found. These markers help us understand cancer better and improve treatment.
Genetic and Molecular Markers
Genetic and molecular markers are key areas in cancer research. They are specific genetic changes or gene expressions linked to certain cancers. For example, BRCA1 and BRCA2 mutations are linked to breast and ovarian cancers.
These markers help find cancer early. They also help doctors tailor treatments to each patient’s genetic makeup.
Liquid Biopsy Technologies
Liquid biopsy technologies are changing oncology. They let doctors check for cancer without surgery. Instead, they look at DNA or cells in blood or fluids.
This method lets doctors track cancer and how well treatments work. It could lead to better patient care.
Using new tumor markers and liquid biopsy tech could change how we fight cancer. As research grows, these tools will be more important in fighting cancer.
Guidelines for Tumor Marker Use in Clinical Practice
Clinical guidelines for tumor marker use are key for proper patient care. They help doctors make smart choices about using these markers. This includes diagnosis, tracking treatment, and follow-up care.
Professional Organization Recommendations
Groups like the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) offer advice on tumor markers. They create guidelines based on the latest research and expert opinions.
- ASCO Guidelines: ASCO has guidelines for breast cancer tumor markers. They stress picking the right markers for each patient.
- NCCN Recommendations: NCCN has detailed guidelines for many cancers. They cover using tumor markers for diagnosis and tracking.
Best Practices for Clinicians
Doctors need to know the best ways to use tumor markers. This includes knowing their limits and possible mistakes.
- Use tumor markers wisely, considering the patient’s situation and history.
- Be mindful of false positives and negatives.
- Know how tumor markers help track treatment success and find recurrence.
By following these guidelines and best practices, doctors can better use tumor markers. This helps improve patient results.
Conclusion
Tumor markers are key in finding and managing cancer. Important markers like PSA, CEA, and CA-125 help doctors a lot. They aid in spotting, tracking, and treating different cancers.
These markers have many uses in fighting cancer. They help in early detection, tracking treatment, and finding cancer that comes back. Knowing how they work is vital for taking care of patients.
The future of cancer diagnosis looks bright. New markers and genetic tech will shape how we find and treat cancer. Liquid biopsies, for example, could make testing for cancer easier and less invasive. As we learn more, cancer care will keep getting better.
FAQ
What are tumor markers, and how are they used in cancer diagnosis?
Tumor markers are substances found in higher amounts in people with certain cancers. They help us screen, diagnose, and monitor treatment.
What is the biological origin of tumor markers?
Tumor markers come from cancer cells or the body’s response to cancer. They are classified by structure and function.
What are some common tumor markers used in cancer diagnosis?
Common markers include PSA for prostate cancer, CEA for colorectal cancer, and CA-125 for ovarian cancer.
How is PSA used in prostate cancer diagnosis and monitoring?
PSA is key for prostate cancer. It helps assess risk, monitor treatment, and detect recurrence.
What are the limitations of tumor marker testing?
Testing can lead to false positives and negatives. Non-cancer conditions can also affect levels, making interpretation tricky.
How are tumor marker results interpreted?
Results need to be understood with reference ranges in mind. Factors that can affect results and when to retest are also important.
What are some emerging tumor markers and research directions?
New areas include genetic and molecular markers. Liquid biopsy technologies also show promise for better diagnosis and treatment.
How are tumor markers used in clinical practice?
We use them for screening, diagnosis, monitoring, and detecting recurrence. Guidelines and best practices help ensure effective use.
Can tumor markers detect cancer at an early stage?
Some markers can help detect cancer early. But their effectiveness depends on the cancer type and marker.
Are there any non-cancerous conditions that can affect tumor marker levels?
Yes, non-cancerous conditions can raise marker levels. It’s important to consider these when interpreting results.
How often should tumor marker tests be performed?
Testing frequency varies by cancer type, treatment, and patient factors. Clinical recommendations guide this.
References
- Duffy, M. J. (2012). Tumor Markers in Clinical Practice: A Review Focusing on Common Solid Cancers. International Journal of Molecular Sciences, 13(12), 14797“14834.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5586699/ - Zhou, Y., et al. (2024). Tumor Biomarkers for Diagnosis, Prognosis and Targeted Therapy. Signal Transduction and Targeted Therapy.
https://www.nature.com/articles/s41392-024-01823-2 - He, C.-Z., Zhang, K.-H., Li, Q., Liu, X.-H., & Hong, Y. (2013). Combined use of AFP, CEA, CA125 and CA19-9 improves the sensitivity for the diagnosis of gastric cancer. BMC Gastroenterology, 13, 87.
https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-13-87