We’re here to help you understand mild cutaneous vasculitis. It’s a condition where small blood vessels in the skin get inflamed. It can show up in different ways, from short-term to long-lasting. Knowing the signs early is key for quick treatment.
Vasculitis makes blood vessels swell and get irritated. This can make the blood vessel walls thicken. This can narrow the vessels and harm organs and tissues. Spotting symptoms early can greatly improve treatment results.
We’ll look at the main signs of this condition. We’ll give you the info you need to tell it apart from other skin problems. In this article, we’ll cover the main features of cutaneous vasculitis and what to watch for.

Cutaneous vasculitis, also known as vasculitis cutanea, is a condition that affects the blood vessels in the skin. It causes inflammation, leading to symptoms like skin lesions and purpura. In severe cases, it can cause ulcers.
Studies show that cutaneous vasculitis affects 38.6 people per million each year. About 45 percent of these cases involve small blood vessels. Anyone can get vasculitis, but some types are more common in certain age groups.
Cutaneous vasculitis is when the blood vessels in the skin get inflamed. It can range from mild to severe. It’s not very common, with an annual incidence of about 38.6 per million people.
“Vasculitis is a complex condition that can affect any organ, but when it affects the skin, it’s termed cutaneous vasculitis.”
Many things can trigger vasculitis, like infections and certain medications. Sometimes, the cause is unknown, making it hard to diagnose and treat.
There are several types of vasculitis that can affect the skin. Each type has its own characteristics. The main types include:
|
Type of Vasculitis |
Characteristics |
Common Symptoms |
|---|---|---|
|
Small Vessel Vasculitis |
Affects small blood vessels |
Palpable purpura, petechiae |
|
Medium Vessel Vasculitis |
Involves medium-sized vessels |
Ulceration, livedo reticularis |
|
Large Vessel Vasculitis |
Affects larger blood vessels |
Reduced pulses, limb claudication |
Knowing about these different types is key for proper diagnosis and treatment. Some types might get better on their own, but most need medicine to control inflammation and prevent flares.

Mild cutaneous vasculitis mainly affects the skin, causing blood vessel inflammation. This can lead to various skin symptoms. These include palpable purpura, petechiae, edematous papules, and plaques.
These symptoms often show up on the lower legs in a bilateral and symmetrical pattern. The skin is the largest and most visible organ. It’s easy to spot early signs of inflammation here. In some cases, skin symptoms may be the first sign of vasculitis, months before other organs are affected.
The characteristics of mild cutaneous vasculitis are key for diagnosis. It’s often marked by specific skin lesions like palpable purpura and petechiae. These lesions are easy to spot and have unique features that set them apart from other skin conditions.
Knowing these characteristics is vital for diagnosing mild cutaneous vasculitis and distinguishing it from other skin conditions.
The main difference between mild and severe cutaneous vasculitis is the extent of inflammation. Mild cases have limited skin symptoms, while severe cases can lead to serious complications. These include ulceration or hemorrhagic bullae.
“The severity of cutaneous vasculitis can vary significantly among patients, with some experiencing mild symptoms while others suffer from more severe manifestations.”
Understanding the differences between mild and severe presentations is key. It helps determine the right treatment and predict patient outcomes.
Vasculitis is a condition that causes inflammation in blood vessels. This inflammation can lead to different skin problems. It’s important to understand how it affects the skin.
Many things can cause vasculitis, like infections, medicines, and diseases. These things make the immune system attack the blood vessels by mistake.
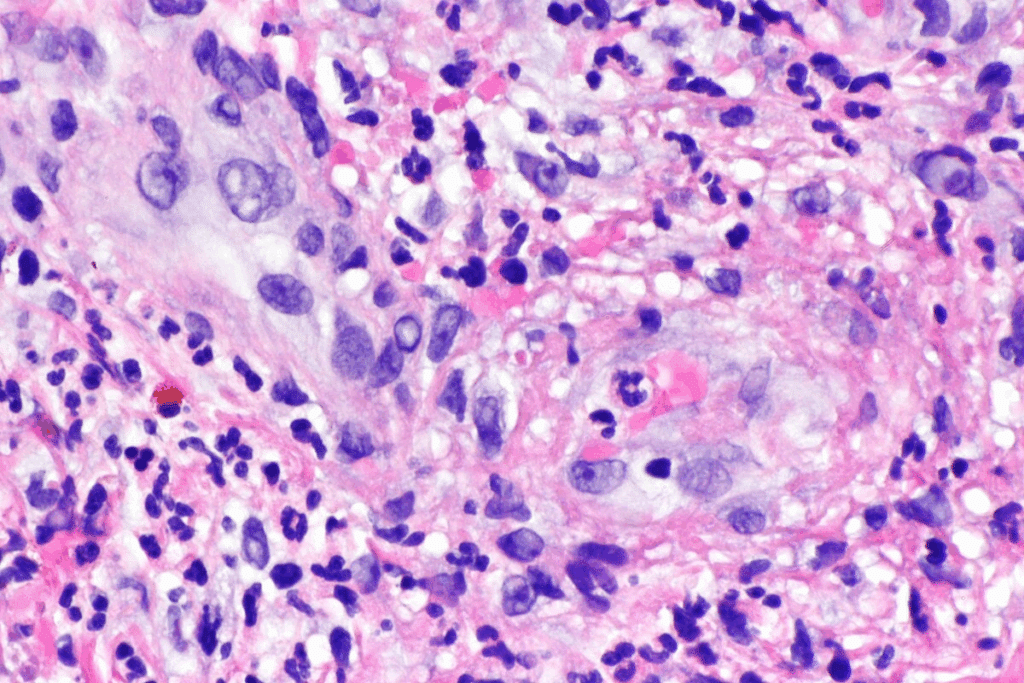
In vasculitis, immune cells get into the blood vessel walls. This damage causes the skin symptoms we see.
Medical Expert, a renowned rheumatologist, says, “Vasculitis can cause many skin symptoms, from mild spots to severe sores.”
“The key to managing vasculitis is understanding its pathophysiology and identifying the underlying triggers.”
Medical Expert, Vasculitis Expert
|
Trigger |
Percentage of Cases |
Common Manifestations |
|---|---|---|
|
Infections |
22% |
Petechial rash, purpura |
|
Medications |
20% |
Cutaneous vasculitis, skin ulcers |
|
Connective Tissue Diseases |
12% |
Petechiae, vasculitic rash |
The immune system is key in vasculitis. It sees the blood vessels as foreign and attacks them.
This attack causes inflammation and damage. Knowing how the immune system works helps us find better treatments.
By knowing the signs and understanding vasculitis, we can manage it better. This helps improve patient care.
It’s important to know about palpable purpura for diagnosing mild cutaneous vasculitis. These are small, raised purple spots usually on the lower legs.
Palpable purpura looks like non-blanching, purplish spots that feel raised. They happen because of inflammation in the small blood vessels of the skin. “The presence of palpable purpura is a hallmark of small-vessel vasculitis,” as noted in medical literature.
To spot palpable purpura, doctors do a detailed skin check. They look at the texture and color of the spots.
Palpable purpura often shows up on the lower legs, ankles, and buttocks. These spots are more likely to happen because of increased pressure. The spots’ location can help figure out what’s causing vasculitis.
It’s key to tell palpable purpura apart from other skin issues. Conditions like petechiae, capillaritis, and thrombocytopenic purpura can look similar. But, palpable purpura stands out because it’s raised and linked to vasculitis.
To tell palpable purpura apart, we look at the whole picture. This includes the patient’s symptoms and test results. A detailed check helps us correctly diagnose and treat cutaneous vasculitis.
Cutaneous vasculitis often shows up as petechiae, tiny spots from blood leakage under the skin. These small, pinpoint spots can pop up anywhere on the body. They are a big sign of the condition. We’ll look at how to spot petechiae, their patterns, and when they’re a worry.
Petechiae are small, red or purple spots from bleeding under the skin. They are flat and can show up in clusters or patterns. To spot petechiae, look for these signs: they don’t fade when pressed, are under 2 mm, and can be on any body part, like legs, arms, and trunk.
Petechiae can show up in different ways, but often on the lower legs. In cutaneous vasculitis, they might be all over or just in certain spots. Knowing where they are helps figure out how bad the condition is. We check the skin closely to see where and how many petechiae are.
Petechiae can be harmless in some cases, but in cutaneous vasculitis, they mean small vessel damage. If you see a lot of petechiae suddenly, and with symptoms like fever, joint pain, or tiredness, get medical help. We look at the whole picture to decide what to do next.
One of the key signs of mild cutaneous vasculitis is the presence of edematous papules and plaques on the skin. These lesions are characterized by their raised, swollen appearance and can vary in size.
Edematous papules and plaques associated with vasculitis skin disease often have a distinct appearance. They are typically erythematous (red) and can be tender to the touch. The texture is usually firm due to the edema (swelling) caused by inflammation.
The development of these lesions is a result of the inflammatory process affecting the blood vessels. As vasculitis wounds progress, they can become more pronounced and potentially lead to further complications if not properly managed.
We observe that the progression of edematous papules and plaques can be influenced by various factors, including the underlying cause of the vasculitis and the effectiveness of the treatment plan.
Patients with edematous papules and plaques due to cutaneous vasculitis may experience additional symptoms. These can include pain or discomfort in the affected areas, itching, and in some cases, systemic symptoms if the vasculitis is part of a more widespread condition.
|
Symptom |
Frequency |
Clinical Significance |
|---|---|---|
|
Pain/Discomfort |
Common |
Indicates active inflammation |
|
Itching |
Occasional |
May suggest allergic or immune-mediated component |
|
Systemic Symptoms |
Less Common |
Could indicate systemic involvement |
Understanding the characteristics and implications of edematous papules and plaques is key for diagnosing and managing vasculitis skin disease effectively.
One of the key signs of cutaneous vasculitis is its pattern. It often shows up in both sides of the body in a symmetrical way. This is more common in mild cases, mainly affecting the lower legs.
The lower legs are where cutaneous vasculitis is most seen. This pattern is a big clue for doctors. It points to a problem that affects the whole body, not just one spot.
Research shows that the lower legs are more likely to get these lesions. This is because of gravity, higher venous pressure, and less oxygen in the skin.
|
Characteristics |
Description |
|---|---|
|
Bilateral Involvement |
Affects both sides of the body equally |
|
Symmetrical Distribution |
Lesions are mirrored on both sides |
|
Lower Extremity Predominance |
Most commonly affects the legs |
The symmetrical pattern of lesions is important. It shows that the problem is not just in the skin. It’s a sign of a bigger issue.
Recognizing bilateral and symmetrical patterns is key. It helps doctors diagnose mild cutaneous vasculitis. It also helps them understand how to treat it.
In short, the symmetrical patterns in mild cutaneous vasculitis are important. They help doctors figure out what’s going on and how to treat it.
The fifth key sign of cutaneous vasculitis involves possible complications that need quick attention. Understanding and spotting these complications early can greatly improve patient outcomes.
One serious complication of cutaneous vasculitis is ulcer formation. These ulcers happen when inflammation and blood vessel damage cause tissue death. Prompt wound care and management are key to avoid infection and aid healing.
Ulcers can be very painful and greatly affect a patient’s life quality. It’s important to watch these ulcers closely and adjust treatments as needed.
Hemorrhagic bullae, or blood-filled blisters, are another complication of cutaneous vasculitis. These bullae form when blood leaks into the skin due to damaged vessels. The presence of hemorrhagic bullae shows a more serious disease.
Handling hemorrhagic bullae requires careful thought to avoid more damage and infection. Treatment might include draining the bullae and treating the underlying cause.
It’s vital to spot the warning signs of cutaneous vasculitis getting worse. These signs include bigger ulcers, new lesions, and systemic symptoms like fever or fatigue. Early detection of these signs allows for timely intervention, which can prevent long-term harm.
Patients should tell their healthcare provider about any new or worsening symptoms. Regular check-ups are essential for tracking disease progression and adjusting treatments as necessary.
It’s important to know what causes cutaneous vasculitis. This helps doctors diagnose and treat it better. Many things can lead to this condition, like infections, medicines, and diseases that affect connective tissue.
Infections are a big reason for cutaneous vasculitis, making up about 22% of cases. Bacteria, viruses, and fungi can start the inflammation. For example, hepatitis B and C are linked to vasculitis. Treating the infection is key to managing symptoms.
Medicines also cause cutaneous vasculitis, in about 20% of cases. Some drugs can trigger an immune response that leads to vasculitis. Common offenders include antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and anticonvulsants. Stopping the bad medicine is a big step in treating drug-induced vasculitis.
Diseases that affect connective tissue are also a risk, making up about 12% of cases. Conditions like rheumatoid arthritis, systemic lupus erythematosus, and Sjögren’s syndrome can lead to vasculitis. Treating the underlying disease is key to managing vasculitis symptoms.
Some cases of cutaneous vasculitis have no known cause, called idiopathic. Even with thorough checks, the exact cause is not found. Researchers are working hard to find out more about these cases.
Here’s a quick list of common causes and risk factors for cutaneous vasculitis:
Knowing these causes helps doctors treat cutaneous vasculitis better. By finding and treating the root cause, we can make treatment plans that work better for patients.
Many skin conditions look like cutaneous vasculitis, making it important to diagnose correctly. We need to look at other skin problems that show similar signs, like petechial rash and vasculitis-like symptoms.
Thrombocytopenic purpura happens when you have too few platelets, causing purpura or petechiae. It’s different from cutaneous vasculitis because it has low platelets and doesn’t have much inflammation in blood vessel walls.
Capillaritis, or pigmented purpuric dermatosis, affects capillaries and shows petechiae and pigmentation. It’s different from vasculitis because it doesn’t affect big blood vessels and doesn’t have systemic symptoms.
It’s important to tell capillaritis apart from vasculitis because their treatments and outcomes are different. Vasculitis affects bigger vessels, which capillaritis does not.
Other conditions that look like cutaneous vasculitis include:
These conditions can show similar skin signs, so a detailed diagnosis is key.
|
Condition |
Key Features |
Differentiating Factors |
|---|---|---|
|
Cutaneous Vasculitis |
Palpable purpura, petechiae, inflammation of blood vessels |
Involvement of larger blood vessels, systemic symptoms |
|
Thrombocytopenic Purpura |
Purpura, petechiae, low platelet count |
Thrombocytopenia, absence of significant vessel inflammation |
|
Capillaritis |
Petechiae, pigmentation, capillary involvement |
Lack of larger vessel involvement, absence of systemic symptoms |
In conclusion, it’s vital to correctly diagnose cutaneous vasculitis from other skin conditions with similar symptoms. A detailed check-up, including your medical history, physical exam, and tests, is needed for the right diagnosis and treatment.
Knowing when to get medical help for vasculitis skin issues is key. Look out for certain symptoms that mean you should see a doctor right away.
Watch for a rash that doesn’t go away when pressed, painful spots, ulcers, or purple marks on your legs. Also, any sudden skin color changes with fever or joint pain are serious signs.
Some symptoms to keep an eye out for include:
These signs might mean you have vasculitis and petechiae. A doctor needs to check you to find out why and how to treat it.
Your doctor will do a physical check-up and ask about your health history. They might also do blood tests or a skin biopsy to confirm vasculitis.
It’s important to tell the difference between capillaritis vs vasculitis to get the right treatment. Your doctor will look at your symptoms and test results to decide the best treatment for you.
When you see your doctor, be ready to talk about your symptoms, health history, and any medicines you’re taking. They might also ask about recent illnesses or infections.
A detailed check-up and diagnosis will help your doctor create a treatment plan just for you. This ensures you get the best care for your condition.
Knowing the signs of mild cutaneous vasculitis is key for early treatment. Recognizing symptoms like palpable purpura and petechiae helps patients get help fast. This can prevent serious problems.
Getting a diagnosis and starting treatment early makes a big difference. Looking at pictures and images of vasculitis helps doctors find the right treatment. This way, patients can get better faster.
If symptoms don’t go away or get worse, it’s important to see a doctor. With the right care, people with cutaneous vasculitis can live better lives. They can enjoy a higher quality of life.
Working with doctors and learning about the condition is important. This helps patients manage their care well. It also lowers the chance of serious long-term problems.
Mild cutaneous vasculitis is a skin condition. It causes inflammation in small blood vessels. This leads to various skin symptoms.
Signs include palpable purpura and petechiae. You might also see edematous papules and plaques. These often appear on the lower legs.
Doctors use a clinical evaluation and medical history. Sometimes, a biopsy is needed. This helps assess inflammation and damage.
It can be caused by infections, medications, or connective tissue diseases. Sometimes, it happens without a known cause.
Mild cases have milder symptoms and fewer complications. Severe cases can cause more damage and affect the whole body.
Complications include ulcers and hemorrhagic bullae. These signs need quick medical attention.
Yes, treatment depends on the cause and severity. It may include medications to reduce inflammation and manage symptoms.
See a doctor if symptoms worsen, you notice signs of infection, or have concerns about your condition.
Prognosis varies based on the cause, severity, and treatment response. Early detection and proper management can improve outcomes.
Follow your treatment plan and monitor symptoms. Making lifestyle changes can help prevent complications and improve your quality of life.
Capillaritis affects capillaries. Vasculitis, on the other hand, involves inflammation of blood vessels, including capillaries, venules, and arterioles.
Yes, specific lesions include palpable purpura, petechiae, and edematous papules and plaques. These are characteristic of the condition.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9532537/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!