Last Updated on November 25, 2025 by Ugurkan Demir
Spotting complete third-degree heart block on an ECG is key for quick medical help. This issue can make about 10% of heart attacks worse. It’s a serious heart rhythm problem.
At Liv Hospital, we stress knowing the important ECG signs of this condition. Quick spotting is vital for good patient care.
Knowing the main signs of 3rd degree heart block helps doctors give top-notch care. We aim for care that’s both focused on the patient and quick.
Key Takeaways
- Understanding the critical ECG findings of complete third-degree heart block is key.
- Quick spotting can greatly help patient results.
- Advanced cardiac care is vital for handling this issue.
- Liv Hospital offers full support for international patients.
- Quick action is essential for good care.
Understanding Complete Third Degree Heart Block
It’s key to understand complete third-degree heart block to help patients. We’ll look into what it is, how it works, and why it happens.
Definition and Pathophysiology
Complete third-degree heart block, or third-degree AV block, stops signals from the atria to the ventricles. This means the atria and ventricles beat on their own. It can greatly lower the heart’s ability to pump blood.
This problem comes from a big issue with the heart’s electrical system. Normally, the heart beats in sync. But with complete third-degree AV block, the ventricles have to find their own rhythm. This is called an escape rhythm.
Common Causes and Risk Factors
Many things can cause complete third-degree AV block. Aging and heart disease are common reasons. These can damage the heart’s electrical system.
Other reasons include:
- Damage to the heart’s electrical system during surgery
- Medicines that can mess with the heart’s rhythm
- Diseases like sarcoidosis or amyloidosis that harm the heart
- Inflammation of the heart, or myocarditis
Knowing these causes helps doctors catch and treat complete third-degree AV block early. This can stop serious problems.
Clinical Significance and Consequences
It’s key to understand the clinical importance of complete third-degree heart block. This condition deeply affects a patient’s heart function and overall health.
Hemodynamic Impact
Complete third-degree heart block makes it hard for the heart to pump enough blood. The hemodynamic impact can be big, causing:
- Less blood being pumped because of the heart’s rhythm problem
- Having to rely more on backup heart rhythms, which might not work as well
- Possible hemodynamic instability, which can get worse with activity or stress
The severity of these effects can differ from person to person. It depends on their heart health and how well their backup rhythm works.
Patient Presentation
People with complete third-degree heart block might show different symptoms, like:
- Dizziness or feeling like they might pass out
- Syncope or near-syncope
- Fatigue and shortness of breath
- Chest pain or discomfort
Healthcare providers need to spot these signs and link them to 3rd degree heart block ECG findings. This helps them give the right care on time.
Looking at 3rd degree heart block rhythm strips is key for diagnosing and managing this condition. By studying these strips, doctors can check if the backup rhythm is stable and spot any early signs of trouble.
In summary, the effects of complete third-degree heart block are big, affecting both heart function and symptoms. It’s vital for doctors to understand these impacts to manage the condition well and help patients get better.
Complete Third Degree Heart Block ECG Fundamentals
To understand complete third-degree heart block, knowing ECG basics is key. The electrocardiogram (ECG) shows the heart’s electrical activity. It helps diagnose by showing complete AV dissociation.
Normal Cardiac Conduction Review
Normal heart conduction is complex. It starts with the SA node sending electrical signals. These signals then go through the AV node to the ventricles, causing the heart to contract in sync.
Knowing normal cardiac conduction helps spot problems in complete third-degree heart block.
The normal pathway is:
- The SA node fires at 60-100 beats per minute (bpm).
- The impulse goes through the atrial tissue to the AV node.
- The AV node delays the impulse before it reaches the ventricles.
- The impulse then moves through the Bundle of His, bundle branches, and Purkinje fibers to activate the ventricles.
Pathophysiologic Changes in Complete AV Block
In complete third-degree heart block, the normal pathway is broken. This leads to complete AV dissociation. The atria and ventricles beat on their own.
The changes include:
- The SA node keeps firing, but the impulses are blocked at the AV node.
- The ventricles have their own slower rhythm.
- This rhythm can start from the AV junction or the ventricles themselves.
Knowing these pathophysiologic changes is key to understanding ECG findings in complete third-degree heart block. It helps spot the 3rd degree av block ecg strip patterns.
Key Finding #1: Complete AV Dissociation
Complete AV dissociation is a key sign of third-degree heart block. It shows independent atrial and ventricular rhythms. This is a key feature to spot on an electrocardiogram (ECG).
Independent Atrial and Ventricular Rhythms
In complete AV dissociation, the atria and ventricles beat on their own. The P waves show atrial depolarization, while QRS complexes show ventricular depolarization. This happens because the electrical block stops impulses from moving from the atria to the ventricles.
So, the atria and ventricles have their own pacemakers. The atria are controlled by the sinoatrial (SA) node. The ventricles are controlled by another pacemaker, either junctional or ventricular.
Differentiating from Isorhythmic Dissociation
It’s important to tell complete AV dissociation apart from isorhythmic dissociation. In isorhythmic dissociation, the atrial and ventricular rates seem similar but aren’t really connected. The P waves and QRS complexes might look like they’re linked by chance, not by a true pathway.
To tell these apart, we need to carefully look at the ECG strip. In complete AV dissociation, there’s no steady PR interval. Also, P waves often “march through” the QRS complexes.
ECG Strip Analysis Techniques
To spot complete AV dissociation on an ECG strip, follow these steps:
- Find P waves and QRS complexes.
- Check if the PR intervals are the same.
- See if P waves “march through” QRS complexes.
- Compare the rates of the atria and ventricles.
By doing these steps and knowing what complete AV dissociation looks like, doctors can correctly diagnose third-degree heart block on an ECG.
Key Finding #2: P:QRS Ratio Discrepancy
When we look at an ECG for Complete Third Degree Heart Block, we notice a key thing. This is the P:QRS ratio discrepancy. It shows that the heart’s atrial and ventricular activities are not in sync. This leads to an imbalance in the number of P waves and QRS complexes.
More P Waves Than QRS Complexes
In Complete Third Degree Heart Block, the ECG shows more P waves than QRS complexes. This happens because the atrial rhythm keeps going, but the ventricles start at a slower pace. The extra P waves mean the atrial depolarization isn’t reaching the ventricles, a sign of complete AV block.
Regular P-P Intervals (60-100 bpm)
The atrial rate in Complete Third Degree Heart Block is usually normal, between 60-100 bpm. It also keeps regular P-P intervals. This regularity helps us tell it apart from other heart block types where the atrial rate might be irregular.
Identifying Hidden P Waves
Diagnosing Complete Third Degree Heart Block can be tricky because of hidden P waves. These P waves are buried in other ECG parts like QRS complexes or T waves. We need to carefully look at the ECG to spot these hidden waves, which is key for a correct diagnosis.
To better find P waves and check the P:QRS ratio discrepancy, looking at multiple leads helps. Sometimes, P waves are clearer in certain leads, which helps us diagnose better.
| ECG Feature | Characteristic | Clinical Significance |
| P:QRS Ratio | More P waves than QRS complexes | Indicates complete AV dissociation |
| Atrial Rate | Regular P-P intervals, 60-100 bpm | Suggests normal sinus node function |
| Hidden P Waves | P waves obscured by QRS or T waves | Requires careful ECG analysis for detection |
Key Finding #3: Escape Rhythm Characteristics
When we look at third-degree AV block, it’s key to spot escape rhythm characteristics. These rhythms help us figure out the best treatment. They show how the heart tries to keep a steady beat.
These rhythms start from different places, like the AV node or the ventricles. Knowing about these rhythms helps us understand the heart’s condition and how severe the block is.
Junctional Escape Rhythms
Junctional rhythms start from the AV junction. They beat between 40-60 times per minute. On an ECG, we see:
- Narrow QRS complexes, unless there’s a bundle branch block
- Absent or retrograde P waves
- A regular rhythm
These rhythms are usually more stable and faster than ventricular rhythms. They’re a better backup for the heart when it’s blocked.
Ventricular Escape Rhythms
Ventricular rhythms start from the ventricles. They beat slower, from 20-40 times per minute. On an ECG, we see:
- Wide QRS complexes
- Dissociation from atrial activity
- Often, a slower rate compared to junctional rhythms
These rhythms are a more basic backup. They often mean the heart’s conduction system is very sick, which can be serious.
Third Degree AV Block with Junctional Escape Rhythm
When third-degree AV block has a junctional rhythm, the ECG shows:
- Complete AV dissociation
- A regular ventricular rate around 40-60 bpm
- Narrow QRS complexes unless there’s a conduction delay
This situation is often more stable than ventricular rhythms. But, it’s important to watch the patient closely and might need pacing.
Knowing about escape rhythms is key for managing third-degree AV block. By looking at these rhythms on an ECG, doctors can learn a lot. This helps them make the best decisions for their patients.
Key Finding #4: QRS Complex Morphology Analysis
When diagnosing complete third-degree heart block, looking at the QRS complex is key. The width and shape of these complexes on an electrocardiogram (ECG) tell us a lot. They show us the level of the block and where the escape rhythm starts.
Narrow QRS Complexes
Narrow QRS complexes are less than 120 milliseconds wide. This means the ventricles are activated through the normal His-Purkinje system. It usually points to a junctional escape rhythm, which happens when the block is closer to the AV node.
Wide QRS Complexes
Wide QRS complexes, wider than 120 milliseconds, show a ventricular escape rhythm. This happens when the block is further down, below the AV node. The ventricles are activated slowly and abnormally. Wide QRS complexes often mean a worse prognosis because of the risk of ventricular dysfunction and asystole.
3rd Degree Block ECG Strip Pattern Recognition
To spot third-degree AV block on an ECG, look for AV dissociation and analyze the QRS complex. The table below shows the main differences between narrow and wide QRS complexes in third-degree heart block:
| Characteristic | Narrow QRS Complexes | Wide QRS Complexes |
| QRS Duration | < 120 ms | ≥ 120 ms |
| Escape Rhythm Origin | Junctional | Ventricular |
| Level of Block | AV Node (proximal) | Below AV Node (distal) |
| Prognosis | Generally better | Generally poorer |
By studying the QRS complex morphology, doctors can understand the heart’s condition better. This helps them make the right decisions for patient care.
Key Finding #5: Transitional ECG Changes
Third-degree heart block shows clear ECG changes that doctors need to spot. These signs show how the heart’s condition is getting worse. They help doctors understand what’s happening inside the heart.
Progression from First and Second Degree Blocks
Third-degree heart block often starts with first or second-degree AV block. It’s important to watch these changes because they can mean the heart’s problems are getting worse. For example, someone with first-degree AV block might move to second-degree and then to complete heart block.
“The move from first or second-degree AV block to complete AV block is common,” say
cardiology experts. They stress the need for regular ECGs to track disease progress.
ST-T Wave Abnormalities
ST-T wave changes also happen, showing how the heart reacts to the block. These can include ST-segment changes, T-wave inversion, or other repolarization issues. It’s key to study these changes to see how they affect the heart’s function.
- ST-segment elevation or depression
- T-wave inversion
- Repolarization abnormalities
3rd Degree Heart Block ECG Findings Over Time
As time goes on, ECG signs in third-degree heart block can change. These changes show how the heart’s conduction system is adapting. Doctors need to watch closely for any signs of trouble or worsening heart function.
Knowing about the ECG changes in complete third-degree heart block helps doctors care for patients better. It helps them decide when to use treatments like pacing.
Key Finding #6: Stability Assessment of Escape Rhythms
When we look at third-degree heart block, checking the stability of escape rhythms is key. It helps us decide the best treatment and understand the patient’s future.
Regular vs. Irregular Escape Rhythms
Escape rhythms in third-degree heart block can be regular or irregular. A regular escape rhythm means a steady ventricular rate. This could mean a stable pacemaker is working well.
An irregular escape rhythm shows changes in the ventricular rate. This might mean the condition is unstable or there are multiple pacemakers.
To tell if a rhythm is regular or irregular, we look at the ECG strip. Regular rhythms have the same R-R intervals. Irregular rhythms have changing intervals.
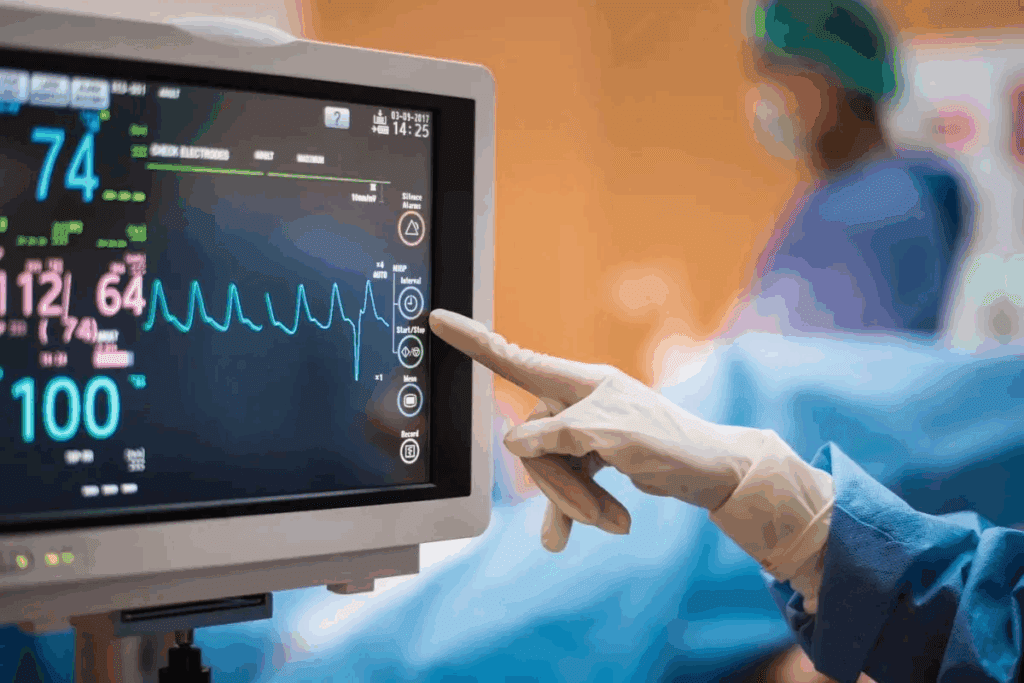
Escape Rhythm Rate Trends
The rate of the escape rhythm tells us a lot about the heart. A junctional escape rhythm is usually between 40-60 bpm. A ventricular escape rhythm is slower, between 20-40 bpm.
Watching how the rhythm rate changes over time helps us understand the patient’s condition. If the rate goes down, it might mean the heart is getting worse. But if it stays the same or goes up, it could be a good sign.
| Escape Rhythm Type | Typical Rate Range (bpm) | Implications |
| Junctional Escape Rhythm | 40-60 | Generally more stable, higher pacemaker site |
| Ventricular Escape Rhythm | 20-40 | Often less stable, lower pacemaker site |
3rd Degree Heart Block Rhythm Strips Interpretation
When we interpret rhythm strips in third-degree heart block, we need to look closely at both atrial and ventricular activities. We look for signs of AV dissociation, the presence of P waves, and the characteristics of the QRS complexes.
Understanding these details helps us see if the escape rhythm is stable. For example, a consistent rhythm with a narrow QRS complex might mean a junctional escape rhythm. This is usually more stable than a ventricular rhythm with a wide QRS complex.
Emergency Management and Intervention
Complete third-degree heart block needs quick and effective action to avoid serious problems. We will cover the key steps in managing this condition. This includes temporary pacing, using medicine, and thinking about permanent pacemakers.
Temporary Pacing Indications
Temporary pacing is often needed for complete third-degree heart block, mainly when patients are unstable. It’s used when there’s symptomatic bradycardia, hemodynamic compromise, or when medicine doesn’t work. It helps keep the heart rate stable until a more lasting solution is found.
Pharmacologic Interventions
Medicine is a key part of treating complete third-degree heart block. Atropine is often the first choice to raise the heart rate, but it doesn’t work for everyone. Other drugs, like isoproterenol, help support the heart rate and blood pressure. But these are temporary fixes until pacing can be set up.
Permanent Pacemaker Considerations
For patients with complete third-degree heart block, a permanent pacemaker is often needed. The choice to get a permanent pacemaker depends on symptoms, heart disease, and if the heart is unstable. We look at the patient’s health, chance of getting better, and future risks when deciding on a permanent pacemaker.
In summary, managing complete third-degree heart block in emergencies needs a mix of temporary pacing, medicine, and thinking about permanent pacemakers. Understanding these steps helps healthcare providers manage this complex condition well and improve patient results.
Conclusion
It’s vital to spot the ECG signs of complete third-degree heart block early. This helps in quick action and better care for patients. We’ve looked at six key ECG signs for diagnosing this condition.
These signs include complete AV dissociation and a P:QRS ratio mismatch. We also discussed escape rhythm features, QRS complex shapes, and changes in ECG patterns. Lastly, we talked about how stable the escape rhythms are.
Healthcare workers need to know these ECG signs well. This knowledge helps them give the best care to patients with third-degree AV block. By recognizing these patterns, doctors can start the right treatments fast.
These treatments might include temporary pacing or medicines. This can greatly improve a patient’s health.
Getting this condition right means knowing how to read ECGs well. We stress the need for ongoing learning in ECG reading. This ensures doctors can handle this serious condition well.
FAQ
What is complete third-degree heart block?
Complete third-degree heart block, also known as third-degree AV block, is a condition. It stops electrical impulses from the atria from reaching the ventricles. This disrupts the normal heart rhythm.
What are the ECG findings characteristic of complete third-degree heart block?
The main ECG findings include complete AV dissociation and a P:QRS ratio discrepancy. There’s also analysis of QRS complex morphology and assessment of escape rhythms. Transitional ECG changes are also significant.
How is complete AV dissociation diagnosed on an ECG?
Complete AV dissociation is diagnosed when the atrial and ventricular rhythms are independent. There’s no association between P waves and QRS complexes.
What is the significance of a P:QRS ratio discrepancy in third-degree AV block?
A P:QRS ratio discrepancy shows that atrial impulses are not reaching the ventricles. This confirms complete third-degree heart block.
What are the characteristics of escape rhythms in third-degree AV block?
Escape rhythms can be junctional or ventricular. Junctional rhythms have a narrow QRS complex and a rate of 40-60 bpm. Ventricular rhythms have a wide QRS complex and a rate of 20-40 bpm.
How is the stability of escape rhythms assessed on an ECG?
The stability of escape rhythms is assessed by looking at rhythm regularity. Regular rhythms suggest stability, while irregular rhythms may indicate instability.
What are the emergency management strategies for complete third-degree heart block?
Emergency management includes temporary pacing and pharmacologic interventions like atropine or isoproterenol. Permanent pacemaker implantation may also be considered.
What is the role of temporary pacing in managing complete third-degree heart block?
Temporary pacing helps stabilize the heart rhythm. It maintains adequate cardiac output until a permanent pacemaker is implanted or the cause is addressed.
How do you differentiate between third-degree AV block and other types of heart block on an ECG?
Third-degree AV block is identified by complete AV dissociation, a P:QRS ratio discrepancy, and specific escape rhythm characteristics. These features distinguish it from other heart block types.
References
- Chaudhry, R. (2022). Physiology, Cardiovascular. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493197/





