Last Updated on November 4, 2025 by mcelik

Discover conditions misdiagnosed as bursitis and how proper testing ensures accurate treatment. Did you know that nearly 30% of patients first thought to have bursitis are later found to have something else? This highlights the challenges involved in accurately diagnosing joint pain. It’s why a detailed differential diagnosis is so important.
Getting the right diagnosis is a big relief, mainly when dealing with severe joint pain. But, different conditions can have similar symptoms. This makes it hard to figure out what’s wrong. Misdiagnosed joint pain can lead to the wrong treatment and more suffering.
At our place, we stress the need for a careful check-up. We want to make sure we’re not mistaking bursitis for other conditions. This way, we can give our patients the right care they need.
Key Takeaways
- Nearly 30% of initial bursitis diagnoses are later found to be incorrect.
- Differential diagnosis is key to accurately diagnosing joint pain.
- Misdiagnosed joint pain can lead to inappropriate treatment.
- A thorough evaluation is needed to tell bursitis apart from other similar conditions.
- Getting the right diagnosis is essential for proper care and easing suffering.
Understanding Bursitis and Its Common Symptoms

Bursitis is a condition where the bursae, fluid-filled sacs, get inflamed. These sacs cushion bones, tendons, and muscles near joints. This inflammation leads to pain, mainly when moving the affected joint.
What Is Bursitis and How Does It Develop?
Bursitis happens when bursae get irritated or inflamed. This can be due to repetitive motion, direct trauma, or infection. Repetitive motion is a big cause, as it causes friction and irritation to the bursae. For example, throwing or lifting can cause bursitis in the shoulder or elbow.
Underlying conditions like rheumatoid arthritis or gout can also lead to bursitis. Sometimes, an infection can cause bursitis, which needs quick medical care.
Common Locations and Symptoms of Bursitis
Bursitis often affects joints that move a lot or get a lot of pressure. The most common spots are the shoulders, elbows, hips, and knees. Symptoms include pain when moving the joint, swelling, and limited mobility.
- Pain that gets worse with movement or pressure
- Swelling or redness around the joint
- Warmth or tenderness to the touch
- Limited range of motion
Typical Diagnostic Criteria for Bursitis
Diagnosing bursitis involves a physical exam, medical history, and sometimes imaging tests like X-rays or MRI. A healthcare provider will check for pain, swelling, and how well you can move. They might also do fluid aspiration to check for infection or other conditions.
To diagnose bursitis, they look at how bad the symptoms are, find any underlying causes, and rule out other conditions like tendonitis or arthritis.
The Challenge of Diagnosing Joint Pain Accurately
Finding the exact cause of joint pain can be tough. Many conditions share similar symptoms. This is shown in health reports, like those from the American College Health Association National College Health Assessment (ACHA-NCHA). They highlight the wide range of health issues students face.
Overlapping Symptoms in Joint Conditions
One big problem in diagnosing joint pain is that symptoms can look the same across different conditions. For example, bursitis, tendonitis, and arthritis all cause pain, swelling, and stiffness. Getting a correct diagnosis means knowing each condition well.
A study in the Journal of Orthopaedic & Sports Physical Therapy points out the challenge. It says diagnosing joint pain is hard because symptoms are not specific and the joint anatomy is complex. This shows we need a detailed way to diagnose.
| Condition | Common Symptoms | Distinguishing Features |
| Bursitis | Pain, swelling, limited mobility | Inflammation of the bursa, often related to repetitive motion |
| Tendonitis | Pain, swelling, tenderness | Inflammation of the tendon, often related to overuse or repetitive strain |
| Arthritis | Pain, stiffness, swelling, joint deformity | Inflammation of the joint, various types including osteoarthritis and rheumatoid arthritis |
Limitations of Clinical Examinations
Clinical exams are key in diagnosing joint pain, but they’re not perfect. They give important clues, but sometimes aren’t enough. Tests like imaging and lab work are often needed to confirm a diagnosis.
“A detailed history, physical exam, and tests are key to accurately diagnosing joint pain.”
— Journal of Clinical Rheumatology
The Importance of a Thorough Diagnostic Approach
Getting a correct diagnosis for joint pain needs a detailed approach. This includes a full medical history, physical exam, and tests like X-rays and MRIs. By using all these tools, doctors can make a precise diagnosis and plan the best treatment.
As we dive deeper into diagnosing joint pain, it’s clear we need a multi-step approach. This ensures we get the right diagnosis and treatment.
Conditions Misdiagnosed as Bursitis: An Overview
Getting the right diagnosis is key because many conditions are mistaken for bursitis. Bursitis is when the bursae, which cushion joints, get inflamed. It can look like other joint problems, making it hard to tell what’s wrong.
Why Misdiagnosis Occurs
Misdiagnosis happens because symptoms of bursitis and other joint issues are similar. Patients often have pain, swelling, and trouble moving. This makes it important to do detailed tests to figure out the real problem.
Common reasons for misdiagnosis include:
- Not doing a full check-up
- Not using imaging tests
- Similar symptoms with other conditions
Common Categories of Conditions Confused with Bursitis
Many conditions are often mistaken for bursitis. These include:
| Condition Category | Examples |
| Tendon-related conditions | Tendonitis, tendon ruptures |
| Arthritic conditions | Osteoarthritis, rheumatoid arthritis, gout |
| Joint structure injuries | Labral tears, meniscus tears, ligament sprains |
The table shows that many conditions are mistaken for bursitis. This highlights the need for a detailed diagnosis.
“The complexity of diagnosing joint pain accurately is a significant challenge in clinical practice, requiring a thorough understanding of the underlying causes.” –
A respected medical journal
The Impact of Misdiagnosis on Treatment Outcomes
Misdiagnosis can really hurt treatment results. If a condition is thought to be bursitis but isn’t, the wrong treatment might be given. This can lead to more pain and make things worse.
Health reports, like those from the ACHA-NCHA, show how important accurate diagnosis is. Knowing which conditions are often mistaken for bursitis helps us get better at diagnosing and treating them.
Tendon-Related Conditions Often Confused with Bursitis
Bursitis is often mixed up with tendon issues like tendonitis and tendon ruptures because their symptoms are similar. These injuries can make it hard to tell what’s wrong. We’ll look at the main differences between these conditions and bursitis, focusing on rotator cuff injuries and Achilles tendonitis.
Tendonitis vs. Bursitis: Key Differences
Tendonitis and bursitis both cause pain and swelling, but they affect different parts of the body. Tendonitis is when the tendons, which connect muscles to bones, get inflamed. Bursitis, on the other hand, is when the bursae, fluid-filled sacs that cushion joints, get inflamed.
To tell tendonitis from bursitis, look at where the pain is and how it feels. Tendonitis pain gets worse when you move or push against the tendon. Bursitis pain gets worse when you press on the bursa.
- Tendonitis pain is usually localized to the area where the tendon attaches to the bone.
- Bursitis pain is typically centered over the bursa, which can be near the joint but not directly on the tendon.
Rotator Cuff Injuries and Shoulder Bursitis Confusion
Rotator cuff injuries are often mistaken for shoulder bursitis because their symptoms are similar. Both can cause pain and make it hard to move your shoulder. But rotator cuff injuries damage the tendons and muscles around the shoulder, while bursitis affects the bursae in the shoulder area.
To figure out what’s wrong, you need a detailed check-up, including imaging studies like MRI or ultrasound. The treatment depends on the correct diagnosis.
Achilles Tendonitis vs. Retrocalcaneal Bursitis
Achilles tendonitis and retrocalcaneal bursitis both affect the ankle and can be confused. Achilles tendonitis is when the Achilles tendon gets inflamed. Retrocalcaneal bursitis is when the bursa between the Achilles tendon and the calcaneus bone gets inflamed.
The main difference is where the pain is and what makes it worse. Achilles tendonitis pain gets worse with activity and gets better with rest. Retrocalcaneal bursitis pain gets worse with pressure on the bursa.
- Achilles tendonitis is more likely to cause pain during and after physical activity.
- Retrocalcaneal bursitis tends to cause pain when the bursa is compressed, such as when wearing tight shoes.
Tendon Ruptures Misdiagnosed as Bursitis
Tendon ruptures can be mistaken for bursitis, even if the symptoms are not severe at first. A tendon rupture is when the tendon tears, causing sudden, severe pain and weakness.
It’s important to tell the difference between a tendon rupture and bursitis because the treatment is different. A ruptured tendon might need surgery, while bursitis can be treated with rest, ice, and anti-inflammatory drugs.
We need to carefully check patients who might have bursitis to make sure they don’t have a tendon rupture. We use a combination of clinical exams and imaging studies as needed.
Arthritic Conditions That Mimic Bursitis Symptoms
Many arthritic conditions can look like bursitis, making diagnosis tricky. Bursitis is when the bursae get inflamed. It’s hard to tell apart from other arthritic conditions because of similar symptoms. We’ll look at how osteoarthritis, rheumatoid arthritis, gout, pseudogout, and polymyalgia rheumatica can seem like bursitis, making it hard to figure out what’s wrong.
Osteoarthritis and Its Bursitis-Like Presentation
Osteoarthritis (OA) is a joint disease that can feel like bursitis. It happens when cartilage wears down, causing bones to rub together and get inflamed. This can be mistaken for bursitis, mainly in the hip or knee. But, joint space narrowing and osteophytes on X-rays are signs of OA, not bursitis.
Rheumatoid Arthritis: Inflammatory Similarities
Rheumatoid arthritis (RA) is an autoimmune disease that can look like bursitis. It causes inflammation in joints, which can be mistaken for bursitis. RA often hits smaller joints, but can also affect bigger ones. The inflammation can feel like bursitis, so it’s important to tell them apart. Tests for rheumatoid factor and anti-CCP antibodies can help tell RA from bursitis.
Gout and Pseudogout: Crystalline Arthropathies
Gout and pseudogout are sudden, severe pain and swelling conditions. They can look like bursitis. Gout is caused by urate crystals, and pseudogout by calcium pyrophosphate dihydrate crystals. Finding these crystals in the fluid is key to diagnosing these conditions, not bursitis.
Polymyalgia Rheumatica vs. Multiple Bursitis Sites
Polymyalgia rheumatica (PMR) is an inflammatory condition that can feel like bursitis. It causes pain and stiffness in the shoulders and hips. PMR is marked by high inflammatory markers and responds well to steroids. Systemic symptoms and no bursae inflammation help tell PMR from bursitis.
In conclusion, many arthritic conditions can mimic bursitis symptoms. This makes it important to do a thorough check-up. Knowing the differences between these conditions helps doctors make the right diagnosis and treatment plan.
Joint Structure Injuries Mistaken for Bursitis
It’s easy to confuse bursitis with injuries like labral tears, meniscus tears, and ligament sprains. These injuries share symptoms like pain and limited movement. Knowing the differences is key to correct diagnosis and treatment.
Hip and Shoulder Labral Tears
Labral tears happen when the cartilage around a joint’s socket gets damaged. In the hip and shoulder, these tears can mimic bursitis symptoms. The labrum, a ring of cartilage, supports and stabilizes the joint. A tear can lead to pain and reduced mobility.
These tears can come from injury, repetitive actions, or structural issues. For example, a sudden twist or a fall might cause a tear. Sports like golf or tennis can also lead to tears over time.
Meniscus Tears in the Knee
Meniscus tears are often mistaken for bursitis. The meniscus is cartilage in the knee that cushions and stabilizes it. A tear can cause pain, swelling, and limited movement, similar to bursitis.
These tears can happen from injury or wear and tear. Athletes are at high risk due to the demands on their knees. It’s important to accurately diagnose meniscus tears to treat them properly.
Ligament Sprains and Their Symptoms
Ligament sprains happen when the ligaments around a joint are stretched or torn. Ligaments connect bones, providing joint stability. Sprains can cause pain, swelling, and bruising, symptoms that might look like bursitis.
Sprains can come from sudden injuries or repetitive strain. For instance, ankle sprains are common in sports that require quick direction changes. Correct diagnosis is vital to treat ligament sprains differently than bursitis.
| Condition | Common Symptoms | Typical Causes |
| Labral Tears | Pain, limited mobility, joint instability | Injury, repetitive motion, structural abnormalities |
| Meniscus Tears | Pain, swelling, limited mobility | Traumatic injury, wear and tear |
| Ligament Sprains | Pain, swelling, bruising | Sudden injury, repetitive strain |
Diagnosing these joint injuries right requires a thorough check-up. This includes a detailed medical history, physical exam, and imaging. Understanding each condition helps doctors create the right treatment plan.
Spine-Related Problems That Present Like Bursitis
Conditions like herniated discs and spinal stenosis can mimic bursitis symptoms. It’s key to check for spine issues when dealing with joint pain. This ensures accurate diagnosis and treatment.
Herniated Discs and Referred Pain
A herniated disc happens when the soft center leaks out. This can cause pain, numbness, or weakness in limbs, often mistaken for bursitis. The pain’s location depends on where the disc is herniated.
Key characteristics of herniated disc pain include:
- Radiating pain or numbness
- Symptoms worsen with movement or straining
- Possible weakness or tingling in the affected limb
Spinal Stenosis Effects on Extremities
Spinal stenosis narrows the spinal canal, pressing on nerves. This can cause pain, numbness, or weakness in limbs, similar to bursitis symptoms.
Spinal stenosis can affect limbs in different ways. Common symptoms include:
- Pain or cramping in the legs or arms
- Numbness or tingling sensations
- Weakness in the affected limbs
Sciatica and Hip Bursitis Confusion
Sciatica is pain along the sciatic nerve from the lower back to legs. It can be mistaken for hip bursitis. Sciatica pain usually goes below the knee, unlike bursitis.
To tell sciatica from hip bursitis, doctors look for specific signs. These include:
- Pain radiating below the knee
- Numbness or tingling in the leg
- Symptoms worsen with certain movements or positions
Facet Joint Syndrome vs. Trochanteric Bursitis
Facet joint syndrome is inflammation of the spine’s facet joints. It can cause pain in the lower back, hips, or thighs, leading to misdiagnosis as trochanteric bursitis.
Distinguishing features of facet joint syndrome include:
- Pain upon movement, like twisting or bending
- Tenderness over the affected facet joint
- Pain referred to the hip or thigh
Nerve Compression Syndromes vs. Bursitis
Nerve compression syndromes and bursitis share similar symptoms, making diagnosis tricky. These conditions cause pain, numbness, and tingling due to nerve compression. Knowing the differences is key for correct diagnosis and treatment.
Carpal Tunnel Syndrome and Wrist Bursitis
Carpal tunnel syndrome affects the wrist by compressing the median nerve. It leads to numbness, tingling, and pain in the hand and wrist. Wrist bursitis causes pain and swelling, but numbness and tingling point to carpal tunnel syndrome. A medical expert notes,
“The key to differentiating between carpal tunnel syndrome and wrist bursitis lies in the presence of neurological symptoms.”
Cubital Tunnel Syndrome and Elbow Bursitis
Cubital tunnel syndrome compresses the ulnar nerve at the elbow. It causes pain, numbness, and tingling in the arm and hand. Elbow bursitis may cause pain and swelling, but cubital tunnel syndrome is marked by neurological symptoms. Accurate diagnosis is key for the right treatment.
Tarsal Tunnel Syndrome and Ankle Bursitis
Tarsal tunnel syndrome affects the ankle and foot by compressing the posterior tibial nerve. It leads to pain, numbness, and tingling in the foot. Ankle bursitis may cause similar symptoms, but tarsal tunnel syndrome is recognized by its neurological signs. Careful examination is needed to tell them apart.
Meralgia Paresthetica vs. Trochanteric Bursitis
Meralgia paresthetica compresses the lateral femoral cutaneous nerve, causing numbness, tingling, and pain in the thigh. Trochanteric bursitis can cause hip pain, but meralgia paresthetica is known for its unique neurological symptoms. Understanding these differences is vital for correct diagnosis and treatment.
Serious Conditions That Require Immediate Attention
Serious conditions can look like bursitis, making it key to get a correct diagnosis. When you feel joint pain, figuring out the real cause is vital for the right treatment. We’ll talk about serious issues that might be mistaken for bursitis and need quick medical help.
Joint Infections (Septic Arthritis)
Joint infections, or septic arthritis, happen when germs get into the joint. This can cause a lot of pain, swelling, and make it hard to move. If not treated, it can damage the joint forever and even be life-threatening. Quick diagnosis and treatment are key to avoid serious problems.
Fractures and Stress Fractures
Fractures and stress fractures can feel like bursitis with pain and swelling. But, they need different treatments. Fractures are breaks in the bone, and stress fractures are tiny cracks from too much stress. It’s important to get a clear diagnosis through imaging to tell them apart from bursitis.
| Condition | Common Symptoms | Diagnostic Approach |
| Fractures | Pain, swelling, limited mobility | X-rays, CT scans |
| Stress Fractures | Pain, swelling, tenderness | X-rays, MRI, bone scan |
Tumors and Malignancies
Sometimes, tumors or cancers can cause joint pain and swelling, like bursitis. Though rare, it’s important to think of these when diagnosing, if the patient has other symptoms or a cancer history. A detailed check, including imaging and biopsy, is needed to accurately diagnose these conditions.
Vascular Conditions Mimicking Joint Inflammation
Some vascular issues, like deep vein thrombosis (DVT) or vascular malformations, can also cause joint pain and swelling. These need quick diagnosis and treatment to avoid serious issues. Being careful and using the right imaging studies are important for spotting vascular problems that look like joint inflammation.
Diagnostic Tools to Differentiate Bursitis from Other Conditions
It can be hard to tell if someone has bursitis without the right tools. We use many diagnostic tools to find out if it’s bursitis or something else. These tools help make sure patients get the right treatment.
Physical Examination Techniques
A detailed physical exam is the first step in finding bursitis. We look for signs like swelling, redness, and warmth. We also check how much the joint can move.
Checking the patient’s history is also important. We look for things like repetitive motion or direct trauma. This helps us figure out what might have caused the bursitis.
Imaging Studies: X-rays, MRI, Ultrasound
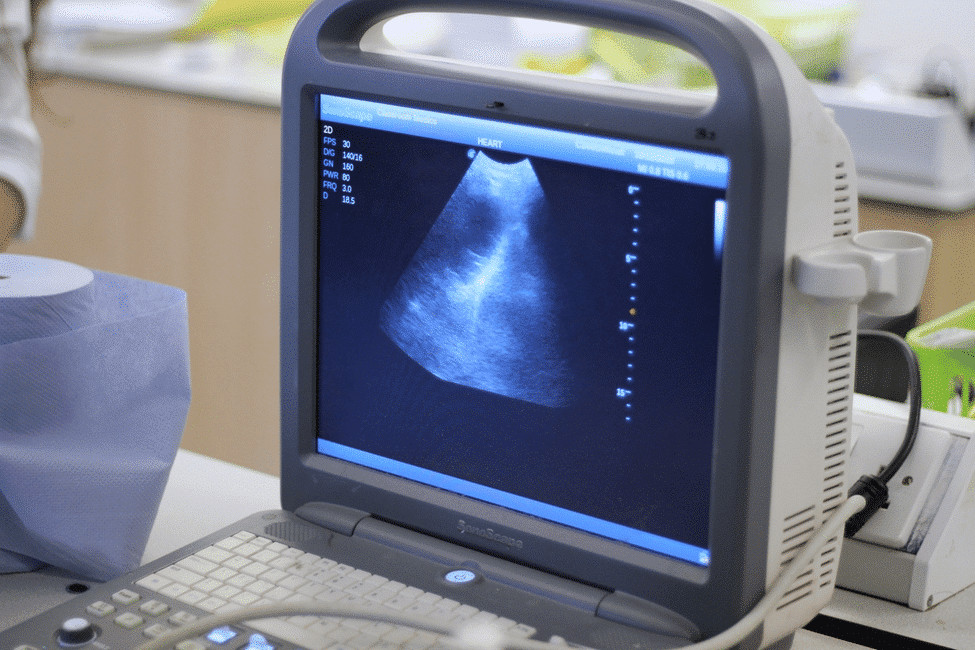
Imaging studies are key in confirming bursitis. X-rays help rule out bone problems like fractures or osteoarthritis. MRI shows soft tissues like bursae, tendons, and ligaments, helping spot inflammation or fluid.
Ultrasound is great for looking at bursitis. It lets us see the bursa moving in real-time. This helps us find fluid and check the surrounding tissues.
Laboratory Tests and Fluid Analysis
Sometimes, we need lab tests to tell bursitis apart from other conditions. Joint fluid analysis is very helpful. It involves taking a sample from the bursa or joint to check for infection or other issues.
Blood tests also give us important info. They check for inflammation markers like ESR or CRP. These tests help us see if there’s inflammation that’s not just from bursitis.
By using physical exams, imaging, and lab tests together, we can accurately diagnose bursitis. Then, we can create a treatment plan that fits the patient’s needs.
Treatment Implications of Misdiagnosis
Misdiagnosing bursitis can lead to the wrong treatment. This can make things worse for the patient. Patients may suffer longer and their condition could get more complicated.
When Bursitis Treatments Won’t Help Other Conditions
Treatments for bursitis, like corticosteroid injections or physical therapy, might not work for other conditions. For example, if a patient has a tendon rupture or a joint infection, these treatments could be ineffective or even harmful.
Common conditions misdiagnosed as bursitis include tendonitis, osteoarthritis, and nerve compression syndromes. Each of these conditions needs a different treatment, showing how important it is to get the diagnosis right.
Potential Complications from Incorrect Treatment
Incorrect treatment due to misdiagnosis can cause many problems. For instance, using corticosteroid injections for a joint infection could make the infection worse. This is because it delays the right antibiotic treatment.
| Condition | Inappropriate Bursitis Treatment | Potential Complication |
| Joint Infection | Corticosteroid Injection | Worsening of Infection |
| Tendon Rupture | Physical Therapy | Delayed Surgical Intervention |
| Nerve Compression Syndrome | Corticosteroid Injection | Temporary Relief, Delayed Proper Treatment |
The Importance of Reassessment When Symptoms Persist
If symptoms don’t get better with bursitis treatment, it’s time to recheck the diagnosis. This means looking at the patient’s symptoms again, possibly doing more tests, and thinking about other possible diagnoses.
Reassessment is key to making sure patients get the right care. It helps doctors change their diagnosis and treatment plan, which can lead to better results for the patient.
Tailoring Treatment to the Correct Diagnosis
Once the right diagnosis is made, treatment can be made to fit the specific condition. This might include different treatments like medicine, physical therapy, or surgery, depending on the condition.
By focusing on accurate diagnosis and the right treatment, we can help patients get better faster. This also reduces the chance of problems caused by misdiagnosis.
When to Seek a Second Opinion or Specialist Referral
Getting a second opinion or specialist referral can help clarify complex joint conditions. If the first diagnosis is unclear or treatments don’t work, it’s a smart move. It leads to a correct diagnosis and a treatment plan that works.
Red Flags That Suggest a Condition Other Than Bursitis
Certain symptoms and signs might mean it’s not just bursitis. These include:
- Severe pain or swelling that doesn’t improve with rest or treatment
- Systemic symptoms such as fever, weight loss, or fatigue
- Recent trauma or injury to the affected joint
- Neurological symptoms like numbness, tingling, or weakness
- Multiple joint involvement or migratory pain
Spotting these red flags can guide the decision to seek more evaluation.
Types of Specialists for Different Joint Conditions
Depending on the suspected condition, different specialists are needed. For example:
| Condition | Specialist |
| Rheumatoid Arthritis | Rheumatologist |
| Tendon Injuries | Orthopedic Surgeon or Sports Medicine Specialist |
| Nerve Compression Syndromes | Neurologist or Neurosurgeon |
Choosing the right specialist can greatly improve diagnosis and treatment.
Questions to Ask Your Healthcare Provider
Patients should ask their healthcare providers important questions. For example:
- What are the possible causes of my symptoms?
- What diagnostic tests are recommended and why?
- What are the possible risks and benefits of the proposed treatment?
- Are there other treatment options available?
These questions help patients take an active role in their care.
Advocating for a Complete Evaluation
Patients should advocate for themselves by seeking a second opinion or specialist referral when needed. A thorough evaluation can lead to a correct diagnosis and a treatment plan that really works.
Conclusion: Ensuring Accurate Diagnosis for Proper Treatment
Getting a correct diagnosis is key for effective treatment, like in bursitis cases. We’ve looked into how to diagnose bursitis and the challenges of not doing it right. Symptoms can be similar, and exams might not catch everything.
It’s important to consider many possible causes when diagnosing. This way, doctors can give the right treatment. Knowing the differences between bursitis and other conditions helps doctors make better choices. This leads to better care and fewer complications.
To accurately diagnose bursitis, doctors use physical exams, imaging, and lab tests. A thorough approach ensures patients get the right treatment. This shows why doctors need to keep learning and why getting a second opinion is sometimes wise.
FAQ
What is bursitis and how is it diagnosed?
Bursitis is when a bursa, a fluid-filled sac, gets inflamed. It cushions joints and reduces friction. Doctors usually diagnose it by examining you, looking at your medical history, and sometimes using ultrasound or MRI.
What are the common symptoms of bursitis?
Symptoms include pain, swelling, and trouble moving the affected area. The pain can be sharp or last a long time. It often gets worse when you move or press on it.
Why is bursitis often misdiagnosed?
It’s often mistaken for other conditions because its symptoms are similar. This includes tendonitis, osteoarthritis, and nerve issues. Getting a correct diagnosis needs a detailed check-up.
What conditions are commonly misdiagnosed as bursitis?
Tendonitis, osteoarthritis, rheumatoid arthritis, gout, and other injuries are often mistaken for bursitis. This is because their symptoms can be similar.
How can tendonitis be distinguished from bursitis?
Tendonitis is inflammation of the tendons, while bursitis is of the bursae. Doctors can tell them apart by examining you and using imaging studies to see inflammation or swelling.
What role do imaging studies play in diagnosing bursitis?
Studies like X-rays, MRI, and ultrasound help spot bursitis. They show the bursa, tendons, and other structures. They can also find inflammation or other issues.
Can gout be misdiagnosed as bursitis?
Yes, gout can be mistaken for bursitis because it causes sudden, severe pain and swelling. But gout has urate crystals in the joint, which can be seen through fluid analysis.
When should I seek a second opinion for suspected bursitis?
Get a second opinion if your symptoms don’t get better or get worse. Also, if you have severe pain, fever, or trauma, or if you’re not sure about your diagnosis.
What are the treatment implications of misdiagnosing bursitis?
The wrong treatment can cause more problems or slow down healing. It’s important to get the right diagnosis for the right treatment.
How can I advocate for a more detailed evaluation?
Ask your doctor about other possible conditions and request detailed tests. If needed, ask for a specialist’s opinion.
Reference
- Common Superficial Bursitis. (2017, February 15). American Family Physician, 95(4), 224‑231. Retrieved from https://www.aafp.org/pubs/afp/issues/2017/0215/p224.html