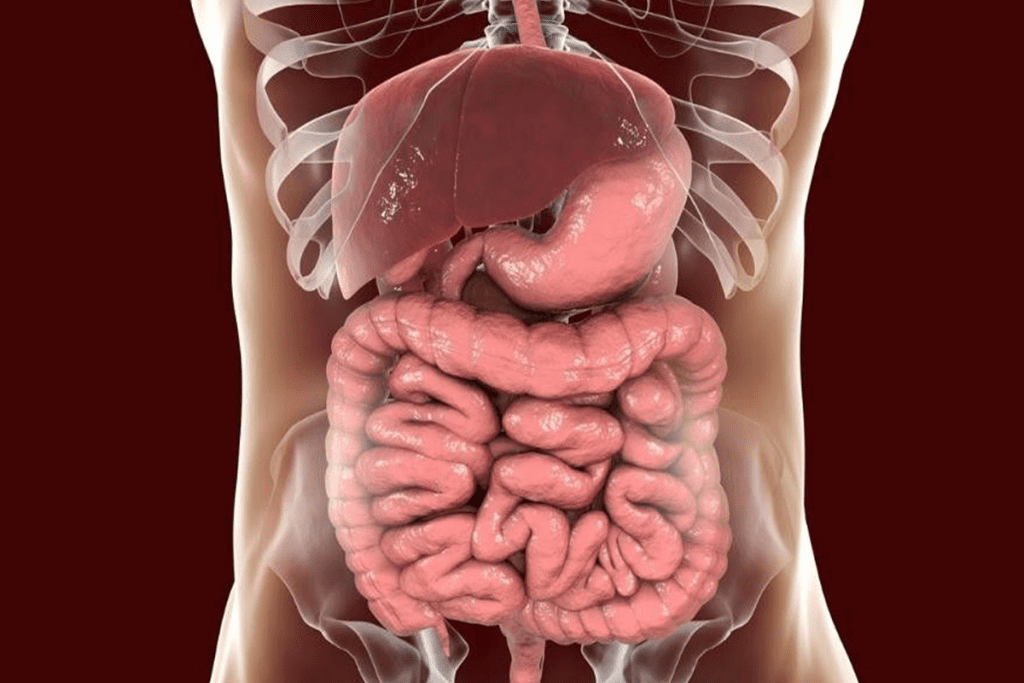
Congenital malformations of the gastrointestinal (GI) tract are big problems for babies worldwide. They happen when organs don’t form properly during pregnancy.

These structural or functional anomalies can cause serious health problems in babies. It’s important to know about the different congenital abnormalities of the GI tract. This helps us give the best care and support to babies.
Key Takeaways
- Congenital malformations of the GI tract are a leading cause of infant health issues.
- These abnormalities occur during fetal development.
- Understanding congenital abnormalities is key to the best care.
- The GI tract is a complex system prone to various congenital malformations.
- Timely intervention is key to managing these conditions.
Overview of Congenital Malformations in the Digestive System
It’s key for healthcare providers to understand congenital malformations in the digestive system. These disorders happen during fetal development. They greatly affect the health and well-being of infants.
Definition and Embryological Development
Congenital anomalies of the digestive system are structural defects at birth. They come from abnormal development in the womb. The formation of the gastrointestinal tract is complex, involving the foregut, midgut, and hindgut.
Disruptions in this process can cause various malformations. These can be due to genetics, environment, or both. The digestive system’s complex development makes it prone to many anomalies.
Global Prevalence and Mortality Statistics
Gastrointestinal anomalies make up 31.1% of all congenital anomalies in newborns. In 2021, there were 2206.79 thousand cases globally. This led to over 47,000 deaths.
The numbers vary worldwide. Factors like prenatal care, diagnostic tools, and surgical services play a role. Knowing these stats helps healthcare systems plan better and improve care for affected infants.
Common Risk Factors for Gastrointestinal Birth Defects
Understanding the risk factors for gastrointestinal birth defects is key. It helps in giving better prenatal care. Knowing these factors helps healthcare providers support families better.
Genetic Predispositions and Inheritance Patterns
Genetics plays a big role in these birth defects. Some genetic conditions can be passed down in families. This means a family history of these malformations can raise the risk.
Genetic mutations can affect the gut’s development. For example, certain mutations can cause intestinal atresia. Knowing this can help in early detection and treatment.
Environmental Exposures During Pregnancy
Exposure to harmful substances during pregnancy is another risk factor. Chemicals, pollutants, and infections can increase the risk of congenital malformations. Pregnant women should avoid harmful substances.

Smoking and drinking alcohol during pregnancy also pose risks. Smoking can lead to congenital anomalies in the gut. The CDC stresses avoiding harmful substances to prevent birth defects.
Maternal Health Conditions and Medications
Maternal health issues and medications can also affect the risk. Conditions like diabetes and obesity can increase the risk of congenital anomalies. Managing these conditions is important during pregnancy.
Some medications, like anticonvulsants and antibiotics, can also pose risks. Pregnant women should talk to their doctor before taking any medication.
Esophageal Atresia and Tracheoesophageal Fistula
Understanding esophageal atresia and tracheoesophageal fistula is key to managing these complex conditions. Esophageal atresia happens when the esophagus doesn’t connect to the stomach. It often comes with a tracheoesophageal fistula, an abnormal link between the esophagus and the trachea.
Pathophysiology and Classification
Esophageal atresia and tracheoesophageal fistula are birth defects caused by issues in early development. They are classified based on the atresia and fistula and their location. The most common type is esophageal atresia with a distal tracheoesophageal fistula.
Classification Types:
- Type A: Esophageal atresia without tracheoesophageal fistula
- Type B: Esophageal atresia with proximal tracheoesophageal fistula
- Type C: Esophageal atresia with distal tracheoesophageal fistula (most common)
- Type D: Esophageal atresia with both proximal and distal tracheoesophageal fistula
- Type E: Tracheoesophageal fistula without esophageal atresia (H-type)
Clinical Presentation and Diagnostic Approach
Newborns with esophageal atresia often drool a lot, spit up, and have trouble breathing. Doctors usually diagnose it before birth or soon after. A nasogastric tube can’t reach the stomach, and X-rays confirm the issue.
Diagnostic Tools:
- X-ray with nasogastric tube
- Contrast studies (cautiously used)
- Endoscopy
Surgical Management and Postoperative Complications
Surgery is the main treatment for these conditions. The goal is to close the fistula and connect the esophagus. After surgery, babies might face issues like leaks, strictures, and GERD.
Postoperative Care:
- Monitoring for complications
- Nutritional support
- Long-term follow-up for possible late issues
We stress the need for a team effort in treating these complex birth defects. This ensures the best care for affected babies.
Anorectal Malformations: Types and Presentations
Anorectal malformations are complex birth defects affecting the rectum and anus. They can range from mild to severe. Often, they come with other birth defects, making treatment very important.
Anatomical Variations and Classification Systems
Anorectal malformations include many types, from simple to complex. A key system for classifying these is the Krickenbeck classification. It helps doctors choose the right treatment.
“The Krickenbeck classification helps us understand the different types of anorectal malformations,” say pediatric surgeons. It groups malformations by fistula type and location.
Associated Anomalies and VACTERL Association
Many anorectal malformations come with other birth defects, part of the VACTERL association. VACTERL means Vertebral, Anal, Cardiac, Tracheo-Esophageal, Renal, and Limb anomalies. Knowing about these other defects is key to treating anorectal malformations well.
Dealing with VACTERL association means a team of specialists is needed.
Staged Surgical Repair and Functional Outcomes
Surgery for anorectal malformations is often done in stages. It starts with a colostomy, then the main repair, and ends with closing the colostomy. The aim is to help patients control their bowel movements and have normal function.
“The main goal in treating anorectal malformations is to help patients control their bowel and avoid long-term problems,” say pediatric surgery experts.
It’s vital to keep up with patients over time and offer support. This helps meet their unique needs.
Hirschsprung Disease: Congenital Megacolon
Hirschsprung disease is a condition where ganglion cells are missing in the lower colon and rectum. It’s a problem that people are born with.
Pathogenesis and Genetic Basis
This disease causes a blockage because of missing ganglion cells. It happens when neural crest cells don’t migrate right during fetal development. Genetic factors are key, with many genes linked to the disease.
The genetics of Hirschsprung disease are complex. It involves many genes and environmental factors. The RET proto-oncogene is often linked to it, mainly in families.
Clinical Features and Diagnostic Methods
Newborns with Hirschsprung disease may have a swollen belly and trouble passing meconium. Doctors use a few ways to diagnose it. These include looking at the baby, imaging tests, and a rectal biopsy, which is the most accurate test.
It’s important to catch this disease early to avoid serious problems like enterocolitis. Tests help doctors tell it apart from other blockages.
Surgical Approaches and Long-term Bowel Function
Surgery is used to remove the bad part and fix the bowel. There are different surgeries, like the Swenson, Duhamel, and Soave procedures. The right one depends on the patient and the doctor.
Thanks to better surgery, most people do well long-term. Some might have trouble with constipation or incontinence. Regular check-ups are important to handle any ongoing issues and help with the transition to adult care.
Congenital Diaphragmatic Hernia
Congenital diaphragmatic hernia is a serious birth defect that affects lung growth and function. It’s important to understand the congenital diaphragmatic hernia and its embryological basis. This helps us grasp the anatomical issues it causes.
This condition happens when the diaphragm doesn’t form right. This lets organs from the belly move into the chest. This can cause pulmonary hypoplasia, which is a big factor in how well a baby will do.
Embryological Basis and Anatomical Types
The diaphragm forms in a complex way during development. If this process fails, a congenital diaphragmatic hernia can occur. The most common type is the Bochdalek hernia, which usually happens on the left side.
The embryological basis of congenital diaphragmatic hernia is linked to the pleuroperitoneal canal not closing fully during fetal development. Knowing this is key to diagnosing and treating the condition.
Pulmonary Hypoplasia and Physiological Consequences
Pulmonary hypoplasia in congenital diaphragmatic hernia means the lungs don’t develop fully. This leads to breathing problems and other issues. The presence of abdominal organs in the chest can also stop the lungs from growing properly.
The effects of pulmonary hypoplasia include high blood pressure in the lungs and trouble breathing. These problems can greatly affect a baby’s chances of survival.
Management Strategies and Survival Outcomes
Handling congenital diaphragmatic hernia requires a team effort. This includes prenatal checks, care for newborns, and surgery. New ways of managing the condition have led to better survival rates. The focus is on getting the baby ready for surgery and caring for them after.
Surgery usually involves moving the herniated organs back and fixing the diaphragm. Thanks to better care and surgery methods, more babies with congenital diaphragmatic hernia are surviving.
Gastroschisis: Abdominal Wall Defect
Gastroschisis is a condition where the intestines stick out through a hole in the belly. It’s becoming more common and is very hard to treat. Doctors must act fast to help the baby.
Causes and Rising Incidence
The reasons for gastroschisis are not fully understood. It’s thought to be caused by genetics and the environment. Babies born to young mothers are at higher risk. More and more babies are being born with this condition.
A leading researcher says, “The growing number of gastroschisis cases is worrying. We need to find out why and how to stop it.”
“Understanding the underlying factors contributing to this rise is critical for developing effective strategies to manage and potentially reduce the incidence of gastroschisis.”
Prenatal Detection and Monitoring
Doctors use ultrasound to find gastroschisis before birth. This helps plan care after the baby is born. It’s important to watch the baby’s health and any problems.
Surgical Repair and Complications
Fixing gastroschisis involves putting the intestines back inside and closing the hole. The method used depends on the size of the hole and the intestines’ health. Intestinal dysfunction can cause problems like trouble eating and staying in the hospital longer.
The choice of surgery depends on the situation. “The main goal is to fix the intestines and help the baby heal. This improves their long-term health.”
Omphalocele: Herniation into the Umbilical Cord
Omphalocele is a birth defect where the intestines or other organs bulge into the umbilical cord. This happens when the intestines don’t go back into the belly during fetal development. As a result, the organs stay outside, covered by a sac that connects to the umbilical cord.
Distinguishing Features from Gastroschisis
Omphalocele is often mixed up with gastroschisis, another birth defect. But they are different. In gastroschisis, the intestines stick out through a hole near the belly button. In an omphalocele, the intestines bulge into the umbilical cord, and they’re covered by a membrane.
Key distinguishing features include the location of the defect and the presence of a covering membrane in an omphalocele. Knowing these differences is key to correct diagnosis and treatment.
Associated Chromosomal and Cardiac Abnormalities
Omphalocele often comes with other birth defects, like genetic issues and heart problems. It might mean there’s a genetic syndrome, like Beckwith-Wiedemann syndrome or Trisomy 18. Heart issues are common, so a pediatric cardiologist needs to check the heart.
A comprehensive assessment is essential to spot any linked problems early. This includes genetic tests and heart scans to check how well the heart is working.
Treatment Approaches and Staged Repair
Treating an omphalocele means surgery, which might be done in parts. First, the baby is stabilized, and the bulging organs are protected. The surgery aims to put the organs back in the belly and fix the hole.
In big cases, staged repair is needed. This means covering the hole first, then slowly moving the organs back into the belly. The goal is to fix the belly wall well and help it grow normally.
Intestinal Atresia and Stenosis
It’s important to understand intestinal atresia and stenosis for managing birth defects in the gut. Atresia means a complete blockage, while stenosis is a partial narrowing. These issues can greatly affect a person’s quality.
Duodenal, Jejunal, and Ileal Variants
These conditions can happen in different parts of the small intestine. Duodenal atresia often comes with other birth defects, like Down syndrome. Jejunal and ileal atresias might happen due to blood issues during pregnancy.
Knowing the type of atresia helps doctors choose the right surgery.
Clinical Presentation and Diagnostic Imaging
The symptoms of these conditions depend on where and how bad the blockage is. Signs include vomiting, a big belly, and trouble passing the first stool. Diagnostic imaging is key to confirming the diagnosis, with X-rays and ultrasound being common tools.
Ultrasound during pregnancy might spot these issues early, helping with care after birth.
Surgical Correction and Nutritional Management
Surgical correction is the main treatment for these issues. Surgery aims to fix the blockage and get the intestine working right. The surgery method depends on the blockage’s type and location.
Nutritional management is vital after surgery. Patients might start with IV nutrition, then move to eating through the gut as it heals.
Keeping up with follow-up visits is important to watch for any problems and make sure the patient is getting enough nutrients.
Malrotation and Midgut Volvulus
Intestinal malrotation, complicated by midgut volvulus, is a surgical emergency. It happens when the intestine doesn’t rotate right during fetal development. This increases the risk of volvulus, where the intestine twists around its mesenteric attachment.
Normal and Abnormal Intestinal Rotation
Normal intestinal rotation is a complex process during fetal development. The intestine rotates and fixes in place. Abnormal intestinal rotation, or malrotation, occurs when this process is disrupted. This leads to a higher risk of complications like midgut volvulus.
It’s important to understand both normal and abnormal rotation to diagnose and manage malrotation. An upper GI series can help spot the abnormal intestinal position.
Acute Presentation and Bilious Vomiting
Patients with malrotation and midgut volvulus often show up with bilious vomiting, abdominal pain, and signs of intestinal obstruction or ischemia. It’s key to recognize these symptoms quickly for timely treatment.
Bilious vomiting is a warning sign that needs immediate action. It usually starts with imaging to check the intestine’s anatomy and health.
Emergency Management and Ladd’s Procedure
Managing midgut volvulus is urgent and needs quick surgery. Ladd’s procedure is the usual surgery. It involves detorsion of the volvulus, cutting any abnormal peritoneal bands (Ladd’s bands), and widening the mesenteric base to stop future twisting.
- Ladd’s procedure is done to fix the obstruction from the volvulus.
- The surgery includes detorsion of the twisted intestine.
- Dividing Ladd’s bands is key to avoiding future problems.
Quick emergency management with Ladd’s procedure can greatly improve outcomes for patients with malrotation and midgut volvulus.
Multidisciplinary Management of Gastrointestinal Congenital Malformations
Managing gastrointestinal congenital malformations needs a team effort. Healthcare experts from different fields work together for the best care.
Prenatal Diagnosis and Counseling
Prenatal diagnosis is key in managing these malformations. Ultrasound and MRI help spot them before birth. Counseling helps families prepare and understand their options.
Early detection allows for better planning and care after birth. Counseling covers the diagnosis, what to expect, and possible surgeries.
Neonatal Intensive Care Considerations
Newborns with these malformations need special care. They often need surgery and support to manage complications.
Our neonatal unit offers advanced care, like breathing help and nutrition. A team creates a care plan for each baby.
Long-term Follow-up and Transition to Adult Care
Long-term care is essential for these patients. It helps catch any issues early and supports them. We help them move to adult care smoothly.
We teach patients and families about their condition and care. We also connect them with adult care providers for ongoing support.
Our team approach improves care for these patients. We support them from birth to adulthood.
Conclusion: Advances in Care and Future Directions
Medical care has made big strides for those with gastrointestinal congenital malformations. We’ve seen major improvements in diagnosing and treating these complex issues. This has greatly improved the lives of those affected.
Research and new surgical methods keep getting better. As we learn more about these conditions, so will our treatment plans. This opens up new paths for caring for these malformations.
The future of treating congenital malformations depends on innovation and teamwork in healthcare. By expanding on current care, we can make patient outcomes even better. This will help support those dealing with these conditions fully.
FAQ
What are congenital malformations of the gastrointestinal tract?
These are birth defects in the digestive system. They happen during fetal development. They can cause serious health problems in babies.
What is the definition of congenital anomalies?
Congenital anomalies are defects that happen before birth. They can affect how a body part works or its structure.
What are the common risk factors associated with gastrointestinal birth defects?
Risk factors include genetics, exposure to certain things during pregnancy, and the mother’s health.
What is esophageal atresia and tracheoesophageal fistula?
These are birth defects of the esophagus and trachea. They need quick diagnosis and treatment to avoid problems.
What are anorectal malformations?
These are birth defects of the anus and rectum. They come in different types and often go with other defects.
What is Hirschsprung disease?
It’s a condition where the colon lacks nerve cells. This leads to bowel problems.
What is a congenital diaphragmatic hernia?
It’s a hole in the diaphragm. This lets organs from the belly move into the chest. It can harm lung development.
What is gastroschisis?
It’s a defect in the belly wall. This lets the intestines stick out. It needs surgery to fix.
What is an omphalocele?
It’s when the intestines or other organs stick out through the umbilical cord. It needs treatment and often more than one surgery.
What are intestinal atresia and stenosis?
These are defects in the small intestine. They cause blockages or narrowing. Surgery is needed to fix them.
What are malrotation and midgut volvulus?
These are defects in how the intestines twist. They can cause sudden problems. They need quick treatment.
How are gastrointestinal congenital malformations managed?
They are managed by a team. This includes prenatal care, neonatal care, surgery, and follow-up.
What is the significance of prenatal diagnosis in gastrointestinal congenital malformations?
Early detection helps plan care. It lets doctors give advice and prepare for after birth.
What are the long-term outcomes for individuals with gastrointestinal congenital malformations?
Outcomes vary by condition and care. But with better care, many people can live full lives.
References
- Centers for Disease Control and Prevention. (2023). Preventing birth defects. Retrieved fromhttps://www.cdc.gov/ncbddd/birthdefects/prevention.html
- World Health Organization. (2020). Congenital anomalies: Key facts. Retrieved fromhttps://www.who.int/news-room/fact-sheets/detail/congenital-anomalies.
- Chimah, O. U., & Ukwuoma, U. (2022). Congenital malformations: Prevalence and characteristics in newborns. Journal of Pediatric Surgery, 2(1), Article 47.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9059225/
- Khan, S., et al. (2023). Prevalence and pattern of gastro-intestinal tract congenital anomalies: A 30-year hospital based study. International Journal of Life Sciences and Pharma Research, 12(2), 1568-1571.http://ijlbpr.com/uploadfiles/280vol12issue2pp1568-1571.20230527102733.pdf


































