Last Updated on November 25, 2025 by Ugurkan Demir
Hypertension is a big risk for heart diseases, like coronary heart disease (CHD). We know how important it is to control high blood pressure for better heart health. People with high blood pressure are twice as likely to get CHD as those with normal blood pressure.
At Liv Hospital, we offer top-notch care, cutting-edge research, and focus on our patients. We understand how hypertension affects CHD. This knowledge helps us manage and lower the risk of this serious condition.
Hypertension and coronary heart disease (CHD) are big problems worldwide. They affect many people and cost a lot to treat. This is a big worry for health and the economy.
Over 1.28 billion people have hypertension globally. This is a big risk for heart problems and death. High blood pressure is a main cause of CHD.
Studies show that where hypertension is common, CHD also happens more. This shows we need to focus on treating hypertension to prevent CHD.
Hypertension and CHD cost a lot to treat. This includes hospital stays, medicines, and surgeries. Lost work and disability add to the cost.
| Region | Prevalence of Hypertension (%) | Incidence of CHD (per 1000) | Estimated Annual Cost (billion USD) |
| North America | 35 | 10 | 120 |
| Europe | 30 | 8 | 100 |
| Asia-Pacific | 25 | 6 | 80 |
The table shows how much hypertension and CHD cost in different places. It shows the huge financial burden on healthcare.
Managing hypertension well is key. It helps prevent CHD and saves money for healthcare. We need to prevent these problems and make sure people stick to their treatment.
Learn how coronary heart disease hypertension are connected and impact your health.
To understand how hypertension affects coronary heart disease, we need to know what hypertension is. It’s a condition where blood pressure is too high. We’ll look at its definitions, types, and risk factors. This will give us a full picture of hypertension.
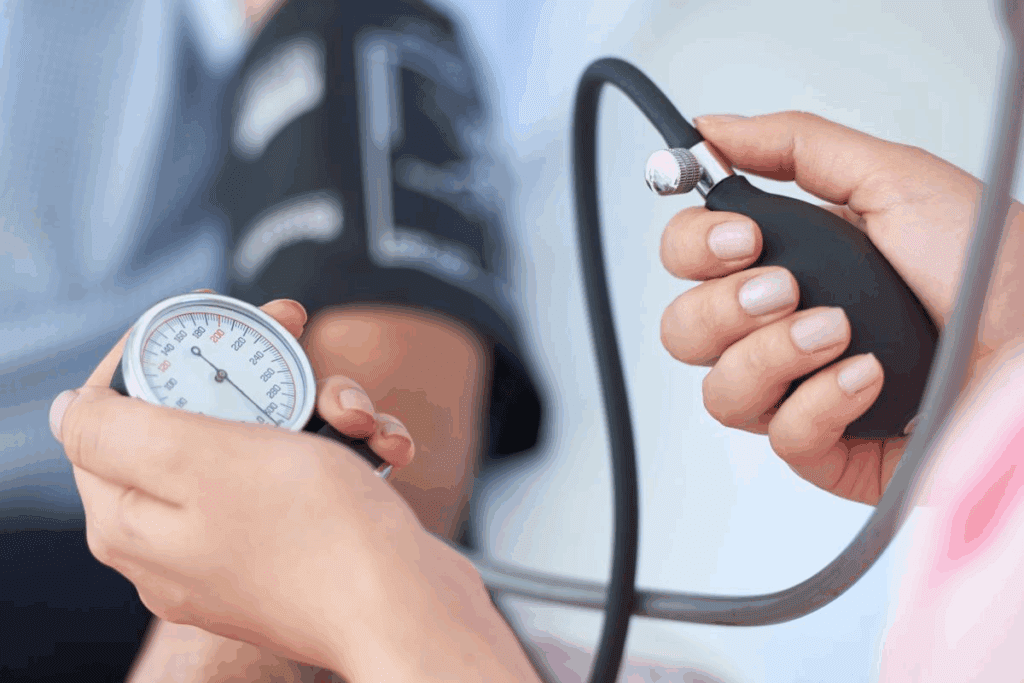
Blood pressure is measured in millimeters of mercury (mmHg). It’s shown as two numbers: systolic and diastolic blood pressure. Knowing these numbers is key to diagnosing and treating hypertension.
Normal blood pressure is less than 120/80 mmHg. Elevated blood pressure is a warning sign. It means you’re at higher risk for heart diseases.
Hypertension is divided into categories based on blood pressure levels. These categories help doctors understand the severity and plan treatment. Here’s a table showing the different types of hypertension:
| Blood Pressure Category | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) |
| Normal | Less than 120 | Less than 80 |
| Elevated | 120-129 | Less than 80 |
| Stage 1 Hypertension | 130-139 | 80-89 |
| Stage 2 Hypertension | 140 or higher | 90 or higher |
Several factors can lead to hypertension. These include age, family history, obesity, lack of exercise, smoking, and too much alcohol. Knowing these risk factors is important for prevention and early treatment.
Understanding risk factors and types of hypertension is key to managing it. This helps prevent it from turning into more serious heart diseases. We’ll keep exploring how hypertension affects heart disease in the next sections.
To understand Coronary Heart Disease, we must explore its pathophysiology. This includes the anatomy of coronary arteries and the development of atherosclerosis. CHD occurs when the coronary arteries, which supply blood to the heart, become narrowed or blocked. This is due to atherosclerosis, leading to various symptoms.
The coronary arteries are key for delivering oxygen and nutrients to the heart. The left main coronary artery and the right coronary artery branch off from the aorta. These arteries split into smaller ones that cover the heart’s surface. Knowing the anatomy of these arteries helps us understand how CHD develops.
Atherosclerosis is the main cause of CHD. It involves the buildup of plaque, made of fat, cholesterol, and other substances, in the arterial walls. This buildup can narrow or block the arteries, reducing blood flow to the heart. The process is complex and involves inflammation, endothelial dysfunction, and smooth muscle cell proliferation.
The symptoms of CHD can vary greatly. They range from no symptoms at all to acute coronary syndromes. Common symptoms include angina pectoris, which is chest pain or discomfort due to temporary heart muscle ischemia. More severe symptoms include myocardial infarction (heart attack) and sudden cardiac death.
Understanding these aspects of CHD is key for diagnosing and managing the disease. The relationship between hypertension and CHD makes things more complex. Hypertension can speed up the progression of atherosclerosis.
The relationship between hypertension and coronary artery disease (CAD) is complex. High blood pressure causes damage to blood vessels. This damage leads to the growth of plaque in arteries, which is a major cause of CHD.
Endothelial dysfunction is a key step in the development of atherosclerosis. High blood pressure harms the endothelium. This harm makes it hard for the endothelium to control blood flow and prevent blood clots.
This damage also leads to more inflammation in the blood vessels. This inflammation attracts harmful cells and starts the formation of plaques.
Hypertension causes the blood vessels to change shape. The walls of the arteries get thicker, and the space inside gets smaller. This is due to the growth of smooth muscle cells and the buildup of connective tissue.
These changes make the arteries less flexible. This increase in blood pressure speeds up the growth of CHD.
Oxidative stress and inflammation are key players in both hypertension and CHD. High blood pressure puts more stress on blood vessels. This stress leads to the production of harmful free radicals.
These free radicals cause more inflammation and damage to the endothelium. This creates a cycle that worsens the disease.
The neurohormonal system, like the RAAS, is important in the connection between hypertension and CHD. RAAS activation causes blood vessels to constrict and hold onto sodium. This increases blood pressure and leads to heart remodeling.
This activation also boosts oxidative stress and inflammation. These factors speed up the growth of CHD.
In summary, the link between hypertension and CHD involves many complex mechanisms. Understanding these is key to finding ways to prevent and treat high blood pressure and CAD.
Epidemiological studies have been key in understanding hypertension’s impact on CHD. They look at large groups over time. This gives us important evidence about the link between high blood pressure and CHD.
Knowing the risk is vital for preventing and managing CHD. It helps us find who’s at higher risk. Then, we can tailor plans to lower that risk.
The Framingham Heart Study started in 1948. It’s a top study on heart diseases, including CHD. It found that high blood pressure greatly increases CHD risk.
Studies, like the Framingham Heart Study, show a big finding. Hypertension doubles the risk of CHD. High blood pressure harms the heart and blood vessels, leading to more CHD risk.
This is why managing high blood pressure is so important. It helps prevent CHD.
Other big studies also link hypertension to CHD. For example, controlling high blood pressure lowers CHD risk. This shows how early detection and treatment are key.
Together, these studies build a strong case. They show managing hypertension is essential in preventing CHD.
Coronary artery disease in people with high blood pressure shows unique signs. These signs need special care. We will look at how CAD shows up in people with hypertension, and the challenges in treating them.
People with high blood pressure face a higher risk of heart attacks and unstable angina. Their heart disease is often worse, making treatment harder. It’s key to control blood pressure and use antiplatelet drugs in these cases.
Stable angina in those with high blood pressure can be tricky to spot. They might feel pain even when they’re not very active. To manage this, doctors focus on lowering blood pressure, prescribe certain drugs, and suggest lifestyle changes.
Hypertension greatly increases the risk of heart failure in CAD patients. High blood pressure can cause the heart to thicken and fail. Spotting and treating high blood pressure early is vital to avoid heart failure.
Hypertensive patients with CAD are more likely to have irregular heartbeats. These irregularities can be dangerous. They also face a higher risk of sudden death, making it important to assess their risk and manage it well.
In summary, CAD in hypertensive patients is complex. Understanding these complexities is key to better treatment and outcomes for these high-risk patients.
Diagnosing coronary artery disease in patients with high blood pressure is complex. We use many tools to check for heart disease risk and presence. This is important for these patients.
Non-invasive tests are key for checking patients with high blood pressure at risk of heart disease. Echocardiography shows how the heart works and looks. It spots signs of heart disease and possible heart blockages.
Stress testing is another important test. It checks how the heart does under stress. A study in the Journal of the American College of Cardiology found it’s very good at finding heart disease in patients with high blood pressure.
“The use of non-invasive imaging techniques, such as stress echocardiography, has revolutionized the diagnosis of coronary artery disease in hypertensive patients.”
— Journal of Hypertension
When tests show a high risk or clear signs of heart disease, coronary angiography is needed. This test shows detailed pictures of the heart’s arteries. It helps find blockages or problems.
Coronary angiography is great for those at high risk or with unclear test results. It helps decide on treatments, like opening blocked arteries.
It’s vital to sort out the risk of heart disease in patients with high blood pressure. We use tools like the Framingham Risk Score to guess the chance of heart problems in the next 10 years. This score looks at age, blood pressure, and cholesterol levels.
By looking at all these factors, we can find who needs more help. This might include changing lifestyle or taking medicine.
Managing patients with high blood pressure and heart disease needs a detailed plan. This plan includes controlling blood pressure, using medicine, making lifestyle changes, and sometimes doing heart surgeries. We will look at each part of this plan.
Guidelines say to keep blood pressure under 140/90 mmHg for most people with high blood pressure and heart disease. Keeping this goal is key to lowering heart attack and stroke risks.
It’s important to check blood pressure often and adjust treatment as needed for each patient.
Medicine is a big part of treating high blood pressure and heart disease. Medicines like ACE inhibitors, beta-blockers, and diuretics help control blood pressure.
Choosing the right medicine depends on the patient’s health and any other health issues they might have.
Changing how we live is also key in managing high blood pressure and heart disease. Eating less salt and more fruits, vegetables, and whole grains can help lower blood pressure.
Exercising regularly, quitting smoking, and keeping a healthy weight are also important lifestyle changes.
For those with serious heart disease, heart surgeries like CABG or PCI might be needed. These surgeries help improve blood flow to the heart. This can make symptoms better and improve life quality.
In summary, managing high blood pressure and heart disease requires a full plan. This plan includes controlling blood pressure, using medicine, making lifestyle changes, and sometimes doing heart surgeries when needed.
We’ve looked into how high blood pressure affects heart disease. High blood pressure can make heart disease worse. It’s a complex issue with many factors involved.
New ways to manage blood pressure and treat heart disease have helped a lot. Keeping blood pressure in check is key. This can be done through lifestyle changes and medicine.
New tools and treatments are on the horizon. These will help manage heart disease better. We’re excited about these advancements for better heart health.
High blood pressure is a big risk for coronary heart disease. It can harm the arteries, making them more likely to get clogged. This increases the chance of a heart attack.
High blood pressure can damage the inner lining of the arteries. This damage can lead to atherosclerosis. It makes the arteries more prone to blockages.
People with high blood pressure and coronary artery disease may have heart attacks or chest pain. They might also experience heart failure or irregular heartbeats. High blood pressure can change how their disease is treated.
Studies like the Framingham Heart Study show that high blood pressure doubles the risk of heart disease. Other studies also confirm this risk.
Guidelines suggest keeping blood pressure under 140/90 mmHg for heart disease patients. Treatment plans may include medicines, lifestyle changes, or procedures to lower blood pressure.
Eating well, exercising regularly, managing stress, and quitting smoking can help. These changes can control blood pressure and heart disease.
Doctors use tests like electrocardiograms and echocardiograms to diagnose heart disease in those with high blood pressure. They may also use more invasive tests like angiography.
High blood pressure can make heart disease harder to manage. It increases the risk of complications. A good plan includes controlling blood pressure and using medicines and lifestyle changes.
While heart disease and high blood pressure are linked, heart disease doesn’t directly cause high blood pressure. But, having one condition can raise the risk of getting the other.
Risk tools help find patients at high risk of heart disease. They guide doctors in making treatment plans. This ensures those at highest risk get the best care.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!