Last Updated on December 2, 2025 by Bilal Hasdemir

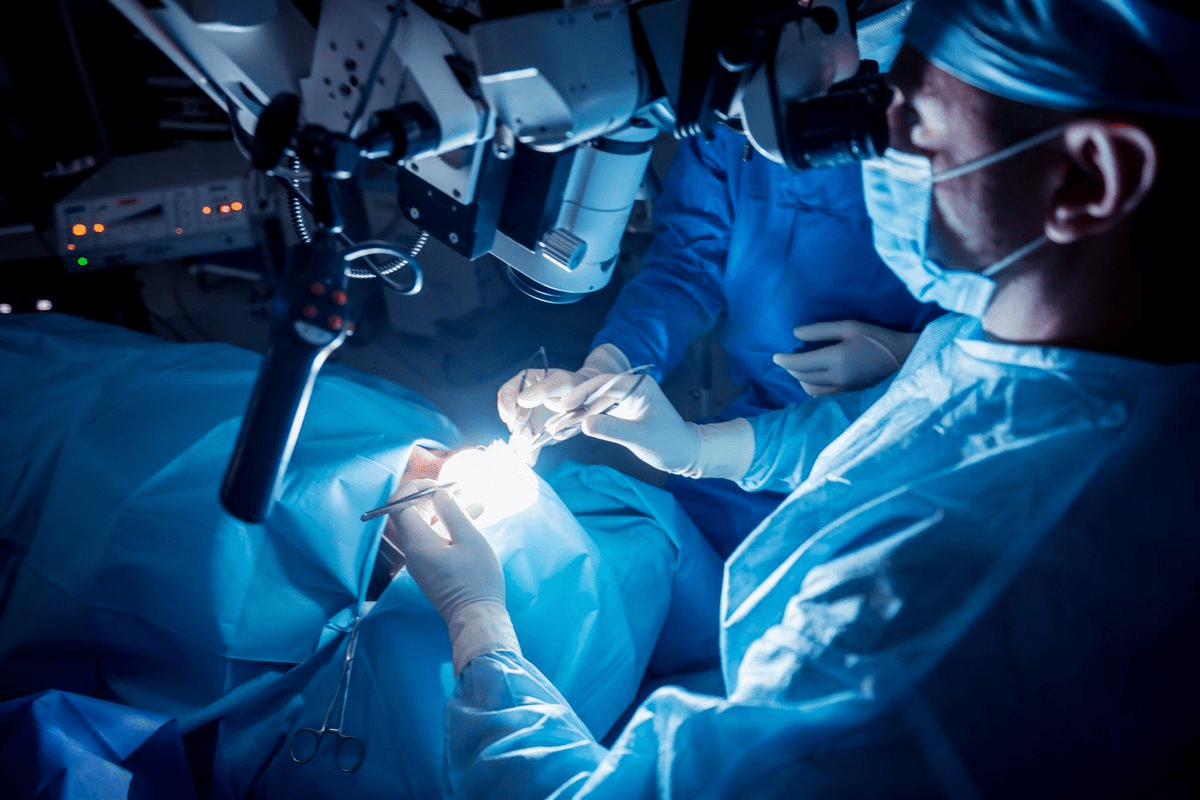
Awake craniotomy is a complex surgery where patients stay awake during parts of it. Surprisingly, studies show these patients often have shorter hospital stays and fewer complications than those who have traditional brain surgery.
Brain surgery can be scary, and recovery worries are common. At our institution, we focus on caring for our patients from start to finish. Our team works hard to give patients the best care, helping them through every step of their recovery.
Key Takeaways
- Awake craniotomy can result in shorter hospital stays.
- Fewer post-operative complications are observed in awake craniotomy patients.
- Personalized care is key for the best recovery.
- Our institution is committed to providing full support during surgery.
- Knowing the recovery time helps plan for post-operative care.
Understanding Awake Craniotomy

Awake craniotomy is a big step in brain surgery. It lets surgeons work while the patient is awake. This requires teamwork between the surgical team and the patient.
Definition and Purpose
An awake craniotomy is a neurosurgical procedure where the patient stays awake during part of the surgery. The main goal is to let surgeons work on the brain while watching the patient’s brain functions live.
This method is great for surgeries on parts of the brain that control important things like speech and movement. By keeping the patient awake, surgeons can check these functions during the surgery. This helps avoid harming important brain areas.
When Is Awake Craniotomy Recommended
Awake craniotomy is often suggested for patients with brain tumors or epilepsy in key brain areas. The choice to do an awake craniotomy depends on the tumor’s size, location, and the patient’s health.
Doctors might also choose awake craniotomy for patients needing detailed brain mapping. This ensures they can save important brain functions.
Difference Between Awake and Traditional Craniotomy
The main difference between awake and traditional craniotomy is the patient’s state during surgery. In traditional craniotomy, the patient is asleep the whole time.
Awake craniotomy, on the other hand, has the patient awake for parts of the surgery. This allows for constant checks on brain functions. This change affects how the surgery is done and the patient’s recovery.
The Science Behind Awake Brain Surgery
The science of awake brain surgery is complex. It involves understanding the brain’s many parts. This surgery lets neurosurgeons work on the brain while the patient is awake. It’s key for surgeries near areas that control important functions like speech and movement.
How the Brain Functions During Surgery
During an awake craniotomy, the brain’s function is watched closely. This lets surgeons map out important brain areas. The brain’s work during surgery is a complex mix of systems.
Neurological mapping is vital. It helps surgeons keep vital brain functions safe. The patient’s awareness during surgery is key. It lets the team make quick adjustments to avoid harming brain functions.
Neurological Mapping
Neurological mapping is a detailed technique used in awake brain surgery. It involves stimulating brain parts and watching the patient’s reactions. This helps surgeons know exactly where to work, reducing risks.
The use of neurological mapping has made awake brain surgeries safer. It lets surgeons remove bad tissue while keeping the patient’s brain functions intact.
Brain Regions and Consciousness
The link between brain areas and consciousness is key in awake brain surgery. Different brain parts handle different functions. Knowing how these areas work together is essential for a successful surgery.
Keeping the patient awake during surgery helps neurosurgeons see how their actions affect the brain. This direct feedback is critical. It helps ensure the surgery goes well without harming the patient’s brain or body.
Preparing for an Awake Craniotomy
Getting ready for an awake craniotomy can make you feel less anxious and improve your results. We’ll walk you through what you need to do. This way, you’ll be well-prepared for the surgery.
Medical Evaluations
First, you’ll have medical checks to see how you’re doing and what’s wrong. These might include:
- Imaging Tests: MRI or CT scans to see your brain clearly.
- Neurological Assessments: Tests to check your brain function and find any issues.
- Blood Tests: To find out if there are any health problems that could affect surgery or recovery.
These tests help us understand your situation better. Then, we can plan your surgery.
Psychological Preparation
It’s also key to prepare your mind for the surgery. Here’s what we suggest:
- Counseling: To talk about any fears or worries you might have.
- Support Groups: Meeting others who have had similar surgeries can be really helpful.
- Relaxation Techniques: Like meditation or deep breathing to help you relax.
By getting your mind ready, you’ll find it easier to handle the surgery and recovery.
What to Expect Before Surgery
In the days before your surgery, you’ll likely:
Day Before Surgery | Day of Surgery |
Avoid eating or drinking after midnight | Arrive at the hospital as instructed by your healthcare team |
Review and sign consent forms | Prepare to undergo anesthesia and the surgical procedure |
By following these steps, you’ll make sure your surgery goes smoothly and successfully.
The Awake Craniotomy Procedure Step by Step
Awake craniotomy is a complex neurosurgical technique. It involves several stages, from the start of anesthesia to the patient’s role during the surgery. A skilled team and a detailed plan are needed for the best results.
Anesthesia Administration
The first step is giving anesthesia. Local anesthesia numbs the scalp, but the patient stays awake. This lets the team do tests during surgery. They watch the patient’s comfort and adjust the anesthesia as needed.
The Awakening Process
After the surgery’s first part, the patient is slowly woken up. This is done carefully to keep the patient comfortable and able to do tests. Waking up is key to checking the patient’s brain function.
Patient Participation During Surgery
During the awake part, the patient does tasks to check their brain function. They might move limbs, speak, or do simple tests. Patient participation is very important for the team to protect key brain areas.
Completion and Immediate Post-Op
After the tests, the patient gets more anesthesia for comfort. The team then closes the incision. The patient goes to the PACU for care after surgery. In the PACU, the team watches the patient’s recovery, managing pain and checking their brain function.
Immediate Recovery: The First 24-48 Hours
Right after an awake craniotomy, a team works together to manage pain and watch the brain. This time is key to keep the patient safe and comfortable.
Intensive Care Monitoring
Patients stay in the ICU for 24 to 48 hours after surgery. ICU staff watch vital signs, brain function, and possible problems. They act fast if something goes wrong.
- They keep an eye on blood pressure, heart rate, and oxygen levels.
- They check the brain often to see if it’s working right.
- They look for signs of bleeding or swelling.
Pain Management
Managing pain is very important right after surgery. We use medicine, position changes, and relaxation to help. Our aim is to reduce pain without risking the patient’s safety.
- We give pain medicine when needed.
- We use other methods like deep breathing to help with pain.
- We check how much pain the patient feels often to adjust treatment.
Initial Neurological Assessments
Neurological checks are done often to see how the patient is doing. These checks look at brain function, muscle strength, and how the patient feels things.
Important parts of these checks include:
- How awake and aware the patient is.
- How strong and coordinated the muscles are.
- How the patient feels things and their reflexes.
By watching the brain closely, we can spot and fix any problems quickly. This helps the patient recover better.
Hospital Recovery Period: Days 3-7
The hospital recovery period is key for patients after an awake craniotomy. Days 3-7 see a big change in care. Patients move from close monitoring to starting their rehabilitation and getting stable.
Physical Therapy Initiation
Physical therapy is key in recovery. It helps patients get stronger, move better, and function better. The therapy starts in the hospital and is made just for each patient.
Therapists help patients with exercises that fit their needs. This could be walking, improving balance, or getting better at small movements.
Physical Therapy Goals | Typical Exercises | Expected Outcomes |
Improve Mobility | Walking, transferring, stretching | Increased independence |
Enhance Strength | Resistance training, balance exercises | Better overall physical function |
Regain Fine Motor Skills | Dexterity exercises, hand therapy | Improved ability to perform daily tasks |
Medication Management
Managing medications is very important during this time. Patients take medicines for pain, to prevent seizures, and for other needs. The healthcare team watches how the medicines work and changes them as needed.
Key aspects of medication management include:
- Monitoring for side effects and interactions
- Adjusting dosages based on patient response
- Educating patients and caregivers on medication administration
As patients get better, the focus is on getting them ready to go home. By days 3-7, many have made big progress. This is thanks to the detailed care they get in the hospital.
Discharge Criteria After Craniotomy
Getting discharged after a craniotomy is a big step in recovery. It’s important to check if the patient is stable and can take care of themselves. This ensures a safe and successful recovery at home.
Neurological Stability Requirements
Before leaving the hospital, patients need to show they are neurologically stable. This means their condition is not getting worse. They should have:
- Stable vital signs
- Minimal or no signs of neurological deficits
- Adequate pain management
Doctors will check the patient’s brain function, motor skills, and senses often. This helps keep track of their recovery.
Self-Care Capabilities
Patients must also show they can do basic self-care tasks. This includes:
- Bathing and personal hygiene
- Dressing and grooming
- Feeding themselves
They should also be able to handle their medicines and follow doctor’s orders.
Home Environment Preparation
Getting the home ready for recovery is key. This means:
- Ensuring a safe and comfortable living space
- Having necessary medical equipment at home
- Arranging for support from family or caregivers
We suggest patients and their families talk to doctors to get the home ready before leaving the hospital.
Discharge Criteria | Description | Importance |
Neurological Stability | Stable vital signs, minimal neurological deficits | High |
Self-Care Capabilities | Ability to perform daily tasks, manage medications | High |
Home Environment Preparation | Safe living space, necessary medical equipment, support system | High |
Early Home Recovery: Weeks 1-2
After an awake craniotomy, home recovery is key. It’s important to manage activities, wound care, and challenges during the first two weeks. This ensures a smooth healing process.
Activity Restrictions
Following activity restrictions is vital. Avoid heavy lifting (more than 5 pounds), bending, or straining. These actions can raise intracranial pressure.
Driving and operating heavy machinery should be avoided until your doctor says it’s okay. Start with short walks and increase distance as you get stronger.
Wound Care and Healing
Proper wound care is essential. Keep the wound dry and clean, as instructed by your surgical team. Watch for signs of infection like redness, swelling, or discharge. Report these to your healthcare provider right away.
Common Challenges During Initial Home Recovery
Patients may face fatigue, headaches, or mild cognitive issues during recovery. Rest and relaxation are important. Having a support system, like family or caregivers, helps with daily tasks and emotional support.
By following these guidelines, patients can better navigate the early stages of recovery. This sets them up for a successful recovery overall.
Mid-Term Recovery: Weeks 3-6
Weeks 3-6 after an awake craniotomy are critical for recovery. Patients make big strides during this time. It’s a key phase for long-term success.
Increasing Physical Activities
Physical activities increase in the mid-term recovery phase. Patients start with gentle exercises and then do more as they get stronger. This helps them regain strength and function.
It’s important for patients to listen to their bodies and not push too hard. The healthcare team will guide them on the right activities based on their progress and needs.
Cognitive Rehabilitation
Cognitive rehabilitation is vital in the mid-term recovery. Patients take cognitive tests to check their brain function. Then, a special program is made to help them improve.
This program helps with memory, attention, and solving problems. Patients should be active in their rehabilitation to get the best results.
Return to Daily Routines
As patients get better, they can start doing daily tasks again. This includes cooking, cleaning, and socializing, which help them feel independent and improve their life quality.
But, patients should pace themselves and not rush back too fast. The healthcare team will help them know when and how to return to their daily activities.
Long-Term Recovery: Months 2-6
Months 2 to 6 after an awake craniotomy are key for recovery. During this time, patients see neurological improvement and gain more independence. They make big strides in their health and skills.
Neurological Improvement Timeline
The pace of neurological improvement differs for everyone. It depends on the surgery’s extent and the patient’s health. Most patients see better brain function over months. This includes better thinking, movement, and speech.
Potential for Return to Work
Many patients wonder when they can go back to work. The time frame depends on the job, recovery speed, and any lasting brain issues. Some might return to work in a few months, while others need more time or changes in their job.
Ongoing Therapy Needs
Ongoing therapy needs are vital for long-term recovery. Patients might need physical, occupational, or speech therapy. The type and amount of therapy depend on each person’s progress and challenges.
Regular check-ups with doctors are key during this recovery phase. They help track progress, solve problems, and adjust treatment plans. Working with healthcare teams helps patients reach their best recovery and improve their life quality.
Factors Affecting Craniotomy Recovery Time
Knowing what affects craniotomy recovery is key for patients and their families. The recovery journey is shaped by many factors. Each one plays a big role in how well a person recovers.
Age and Overall Health
A patient’s age and overall health are very important. Younger people with fewer health problems usually heal faster. Pre-existing medical conditions, like diabetes or heart disease, can make recovery harder.
Tumor Location and Size
The location and size of the tumor being removed also matter a lot. Tumors in sensitive brain areas may need more careful surgery. This can make recovery longer. Also, bigger tumors mean more complex surgery, leading to longer recovery times.
Surgical Complications
Surgical complications, like infections or bleeding, can really slow down recovery. These issues might need extra treatments, making recovery longer. It’s important for doctors to watch closely for any complications.
Pre-existing Conditions
Pre-existing conditions, like neurological disorders, can also affect recovery. People with these conditions might need special care plans to help them heal.
Understanding these factors helps patients and their families prepare for recovery. They know what to expect and how to care for them better.
Potential Complications and Their Impact on Recovery
Recovering from an awake craniotomy means facing possible complications. This surgery is advanced and usually safe. But knowing about these risks is key for patients and their families.
Infection and Wound Healing Issues
Infection is a big worry after surgery, like an awake craniotomy. Signs of infection include redness, swelling, more pain, or a fever. If you see these signs, get medical help fast.
Keeping the wound clean and dry is vital. Follow your doctor’s advice for dressing changes and go to all follow-up visits. Sometimes, antibiotics are given to stop or treat infection.
Neurological Deficits
Neurological problems can happen because of the surgery or complications. These might be weakness, numbness, trouble speaking, or changes in thinking. Rehabilitation is key to help with these issues. It includes physical, occupational, and speech therapy.
We help patients find and deal with these problems early. We make a special plan for each person to help them get better and improve their life.
Seizures and Medication Management
Seizures can be a problem after craniotomy, if the surgery is near areas that can cause seizures. Anticonvulsant medications are used to stop seizures. Managing these medicines is very important during recovery.
We watch for seizures and adjust the medicine as needed. This keeps the medicine working right and stops seizures from happening.
Psychological Challenges
Going through an awake craniotomy and recovering can be tough on the mind. Patients might feel anxious, depressed, or have mood swings. Help from mental health experts is a big part of getting better. They give patients ways to deal with these feelings.
We tell patients to get help when they need it. We also offer resources for counseling and therapy to help with mental challenges during recovery.
Recovery Comparison: Awake vs. Traditional Craniotomy
It’s important to know how awake and traditional craniotomy recovery differ. This knowledge helps both patients and healthcare providers. The recovery process for each procedure has big differences that affect patient results.
Hospital Stay Duration Differences
One big difference is how long patients stay in the hospital. Awake craniotomy patients usually stay less time than those under general anesthesia. This is because they need less ICU monitoring after surgery.
Shorter hospital stays can lower the risk of infections and other problems. This might lead to better health outcomes for patients.
Neurological Outcome Comparisons
How well the brain works after surgery is key. Awake craniotomy might lead to more favorable neurological outcomes. This is because the patient can give feedback during surgery. This helps doctors avoid damaging important brain areas.
A study in a top neurosurgery journal showed awake craniotomy patients had fewer brain problems after surgery. This is compared to those who had traditional craniotomy.
Quality of Life During Recovery
Quality of life during recovery is also important. Patients who have awake craniotomy often feel less pain and discomfort after surgery. This can make their early recovery better.
“The ability to participate in their care and recover more quickly was a significant advantage for patients undergoing awake craniotomy,” noted a leading neurosurgeon.
Also, awake craniotomy patients need less sedation and breathing help after surgery. This means they can get back to normal faster. They might also face fewer long-term brain and mental health issues.
Patient Experiences and Recovery Stories
Patient stories after awake craniotomy offer insights into recovery. They show the challenges and the strength of those who face them.
Case Studies of Successful Recoveries
Many case studies show how people can recover well after awake craniotomy. For example, a patient might have surgery to remove a tumor near a key language area. Being awake, the team can map brain functions live, saving important skills.
Real-life Example: A 35-year-old patient quickly got back to normal after surgery. Being awake during the surgery helped the doctors make precise moves, leading to a good result.
“I was amazed at how quickly I recovered. The support of the medical team was incredible.” –
A patient after awake craniotomy
Challenges Faced by Real Patients
Recovery is not easy for everyone. Patients deal with pain, temporary brain issues, and emotional struggles after surgery.
Common Challenges:
- Cognitive fatigue
- Emotional fluctuations
- Physical limitations
Knowing these challenges helps doctors and caregivers support patients better.
Lessons Learned from Patient Journeys
Patients’ stories teach us a lot. They show the value of care tailored to each person, the need for support, and the importance of educating patients.
Key Takeaways:
- The importance of a multidisciplinary care team
- The role of patient participation in surgical success
- The need for tailored rehabilitation programs
Looking at these experiences helps us improve care for those having awake craniotomy.
Support Resources During Craniotomy Recovery
Support resources are key in helping patients recover from a craniotomy. They offer care that covers medical, emotional, and practical needs. This support is vital as patients go through their recovery journey.
Medical Follow-up Schedule
A good medical follow-up plan is important. It helps track the patient’s recovery and quickly tackles any issues. Follow-up visits are usually set up soon after surgery, with the number of visits decreasing as the patient gets better.
At these visits, doctors check on the patient’s brain health, wound healing, and overall health. They also guide on managing medicines, exercise, and other post-surgery care.
Follow-up Appointment | Typical Timing | Purpose |
First Follow-up | 1-2 weeks post-op | Assess wound healing, neurological status |
Second Follow-up | 4-6 weeks post-op | Evaluate recovery progress, adjust medications |
Third Follow-up | 3-6 months post-op | Assess long-term recovery, address concerns |
Support Groups and Counseling
Support groups and counseling are essential for emotional and mental recovery. They offer a space for patients to share their stories, get support from others, and learn how to manage their condition.
“Support groups were invaluable during my recovery. Hearing others’ stories and sharing my own helped me feel less isolated and more empowered to manage my condition.”
A patient recovering from craniotomy
Home Care Services
Home care services are often needed to ensure patients get the care they need at home. These services can include nursing, physical therapy, and help with daily tasks.
When picking a home care provider, look for their experience with craniotomy patients. Choose a provider that creates personalized care plans for each patient’s needs.
Financial and Insurance Considerations
Dealing with the financial side of craniotomy recovery can be tough. Patients and their families need to know what their insurance covers and what they might have to pay for themselves.
Working with the healthcare team’s financial advisors is a good idea. They can help understand the costs of the procedure, hospital stay, and follow-up care.
Conclusion
Recovering from an awake craniotomy is a complex process. It needs careful postoperative care and support. We’ve looked at the recovery stages, from the first 24-48 hours to long-term improvements.
Knowing what affects recovery, like age and health, is key. Also, understanding possible complications helps manage expectations and improve outcomes.
Support resources, like medical follow-up and support groups, are vital. They help with a smooth recovery. With the right care plan, patients can improve their quality of life.
Remember, every patient’s journey is unique. Recovery from awake craniotomy needs patience, dedication, and the right support. Tailored postoperative care and resources can make a big difference.
FAQ
What is the typical recovery time for awake craniotomy?
Recovery time for awake craniotomy varies. Most patients recover in a few weeks to months. Age, health, and surgery complexity affect recovery time.
How long do I need to stay in the hospital after an awake craniotomy?
Hospital stay after awake craniotomy is a few days to a week. It depends on your condition and the surgeon’s assessment.
What are the benefits of awake craniotomy compared to traditional craniotomy?
Awake craniotomy reduces damage to brain areas. It leads to less swelling, pain, and shorter hospital stays.
Will I be awake during the entire surgery?
You’ll be sedated at first, then awake for the key part. After that, you’ll be sedated again. Being awake time varies by procedure.
How is pain managed during and after awake craniotomy?
Pain is managed with local anesthesia and sedation during surgery. After, medications help. Treatment plans adjust based on your needs.
Can I drive myself home after being discharged?
No, driving yourself home is not advised. Arrange for someone to drive you.
What are the common challenges during the initial home recovery?
Challenges include managing pain, fatigue, and activity restrictions. Cognitive fogginess or emotional changes are common too.
How long does it take to return to normal activities after awake craniotomy?
Returning to normal activities takes weeks to months. It varies by individual.
Are there any long-term effects of awake craniotomy?
Some may face long-term effects like neurological deficits or cognitive changes. Effects depend on surgery complexity and health.
What kind of follow-up care is needed after awake craniotomy?
Follow-up care includes regular check-ups and monitoring for deficits. Rehabilitation therapy may be needed to regain functions.
Can I undergo physical therapy after awake craniotomy?
Yes, physical therapy is recommended to regain strength and function. Therapy is tailored to your needs and progress.
How does age affect the recovery from awake craniotomy?
Older patients may face longer recovery times. But, individual health and condition are key in determining outcome.
Are there support resources available for patients recovering from awake craniotomy?
Yes, support resources include medical follow-up, support groups, and counseling. They help manage recovery and address challenges.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S104236801730082X