Last Updated on December 2, 2025 by Bilal Hasdemir
Craniotomy Candidacy
Nearly 28,000 craniotomy procedures are done every year in the United States. This shows how important this surgery is.
We check patients for craniotomy surgery if they have certain medical issues. These include brain tumors, aneurysms, arteriovenous malformations (AVMs), and traumatic brain injuries. A detailed neurosurgical evaluation is key to see if a patient is a good candidate for brain surgery.
Our team looks at each patient’s situation to decide if a craniotomy is right. We consider the type of condition, where it is, and the patient’s health.
Key Takeaways
- Craniotomy is considered for patients with specific brain conditions.
- A thorough neurosurgical evaluation is necessary.
- Eligibility is determined on a case-by-case basis.
- Factors like overall health and condition severity are assessed.
- Our team provides personalized care for international patients.
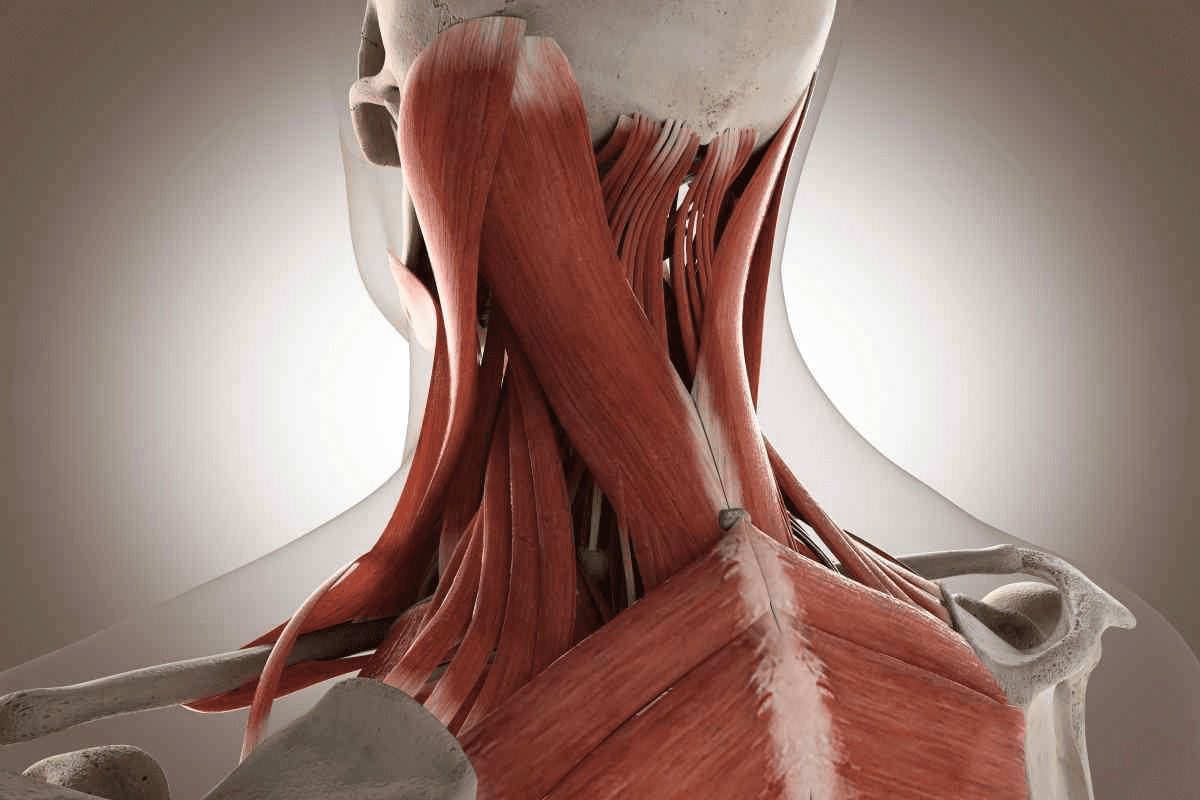
Understanding Craniotomy: A Surgical Overview
a medical illustration of a detailed craniotomy surgical procedure, showing the patient’s head with the scalp opened to reveal the skull, with the cranium neatly cut and opened to expose the underlying brain structure, with precise surgical tools and instruments visible, all under bright, evenly-distributed studio lighting that highlights the technical details, captured from a high-angle perspective to provide a clear, comprehensive view of the entire operation, with a calm, educational mood that conveys the gravity and complexity of the procedure.
Craniotomy surgery is complex but crucial for treating serious brain conditions. We’ll dive into its details to help you understand it better.
Definition and Purpose of Craniotomy Surgery

A craniotomy is a surgery where part of the skull is removed. This bone flap lets neurosurgeons access the brain. They can then remove tumors, clip aneurysms, or relieve brain pressure.
The main goal of a craniotomy is to get to the brain safely. By taking out a part of the skull, surgeons can work on the brain more accurately.
Types of Craniotomy Procedures
There are many types of craniotomy surgeries, each for different brain conditions and areas.
- Frontal Craniotomy: This type accesses the frontal lobe for tumors or injuries.
- Temporal Craniotomy: It’s for the temporal lobe, used for epilepsy or tumors.
- Parietal and Occipital Craniotomy: These are for the parietal and occipital lobes, treating conditions in these areas.
- Bifrontal Craniotomy: This removes a flap over both frontal lobes, for conditions affecting both sides.
Difference Between Craniotomy and Craniectomy
Craniotomy and craniectomy both remove skull parts, but they differ. A craniotomy removes a bone flap temporarily, which is put back after surgery. On the other hand, a craniectomy removes a skull part without replacing it, usually due to swelling or complications.
Knowing the difference between these surgeries is key for patients. It helps them understand their surgery and what to expect during recovery.
Medical Conditions That May Require Craniotomy
a highly detailed, photorealistic image of a craniotomy procedure to remove a brain tumor. The image should show the open skull of the patient, with the tumor clearly visible. The surgical team should be present, with the neurosurgeon working diligently to excise the tumor. The lighting should be bright and clinical, with a slight blue tinge to convey the sterile environment of the operating room. The angle should be slightly elevated, providing a clear view of the procedure. The image should convey the technical complexity and precision required for such a delicate operation, while also highlighting the gravity of the medical condition being treated.
Many medical conditions can lead to the need for a craniotomy. This surgery involves temporarily removing part of the skull. These conditions are serious and often require quick, effective treatment.
Brain Tumors and Masses
Brain tumors, whether they are benign or malignant, can cause symptoms. These symptoms depend on the tumor’s size and location. A craniotomy may be needed to remove large or pressing tumors.
The choice to do a craniotomy for brain tumors depends on several things. These include the tumor’s type, size, and where it is. New neurosurgical techniques have helped improve surgery outcomes for brain tumors.
Traumatic Brain Injuries
Traumatic brain injuries (TBI) can happen from severe head trauma. They can be very dangerous. A craniotomy might be needed to reduce brain pressure from swelling or bleeding.
The seriousness and type of TBI decide if surgery is needed. Sometimes, a craniotomy is done to fix damaged blood vessels or remove bone fragments in the brain.
Cerebrovascular Conditions
Cerebrovascular conditions, like aneurysms and arteriovenous malformations (AVMs), are risky. A craniotomy is often needed to treat these. This is done by clipping aneurysms or removing AVMs.
Cerebrovascular Condition | Description | Treatment |
Aneurysm | A bulge in a blood vessel caused by weakness in the vessel wall | Clipping or coiling to prevent rupture |
Arteriovenous Malformation (AVM) | An abnormal connection between arteries and veins | Surgical removal or embolization |
Neurological Disorders Requiring Surgical Intervention
Some neurological disorders may need surgery, including craniotomy. This is to help symptoms or treat the cause. Conditions like epilepsy and hydrocephalus might need surgery in some cases.
Deciding on a craniotomy for neurological disorders involves careful evaluation. It also considers less invasive options. Advances in neurosurgery have made more conditions treatable.
Craniotomy Candidacy: Who Qualifies for the Procedure
A well-lit medical examination room with a physician reviewing a patient’s medical scans on a computer monitor. The patient, a middle-aged individual, is sitting upright on an examination table, their head exposed, indicating a discussion of potential craniotomy. The doctor’s expression is serious, yet empathetic, as they explain the procedure and evaluation process. The room is clean, with modern medical equipment visible in the background, conveying a professional, clinical atmosphere. Soft, directional lighting illuminates the scene, creating depth and highlighting the key subjects. The overall mood is one of a thoughtful, focused evaluation of the patient’s candidacy for the craniotomy procedure.
To see if someone can have a craniotomy, doctors check their health and medical conditions. This check is key to find out who can safely have the surgery and get better from it.
General Health Requirements and Evaluation
Before a craniotomy, doctors look at a patient’s health to make sure they can handle the surgery. They check the patient’s medical history, current health, and any risks from the surgery. A good check before surgery is key to avoid problems and get the best results.
What health is needed for a craniotomy can change based on the reason for the surgery. But, patients usually need to be in good health, with chronic conditions they can manage. Our medical team does a detailed check to see if each patient is right for the surgery.
Age Considerations and Impact on Eligibility
Age is important when deciding if someone can have a craniotomy. Being older can mean more risks because of less health and more health problems. Our neurosurgeons look at the age-related risks and benefits for each patient.
Deciding if an older patient can have a craniotomy depends on their health, how bad their condition is, and how well they can recover. Younger patients might recover faster, but each case is looked at on its own.
Contraindications for Craniotomy Surgery
Some health issues or situations make a craniotomy not possible. These include severe bleeding problems, active infections, or big heart problems. Patients with these issues might need to fix their problems first before surgery.
Also, people with serious brain problems or unstable health might not be good candidates for a craniotomy. Our team talks with patients and their families about the risks and benefits to find the best option.
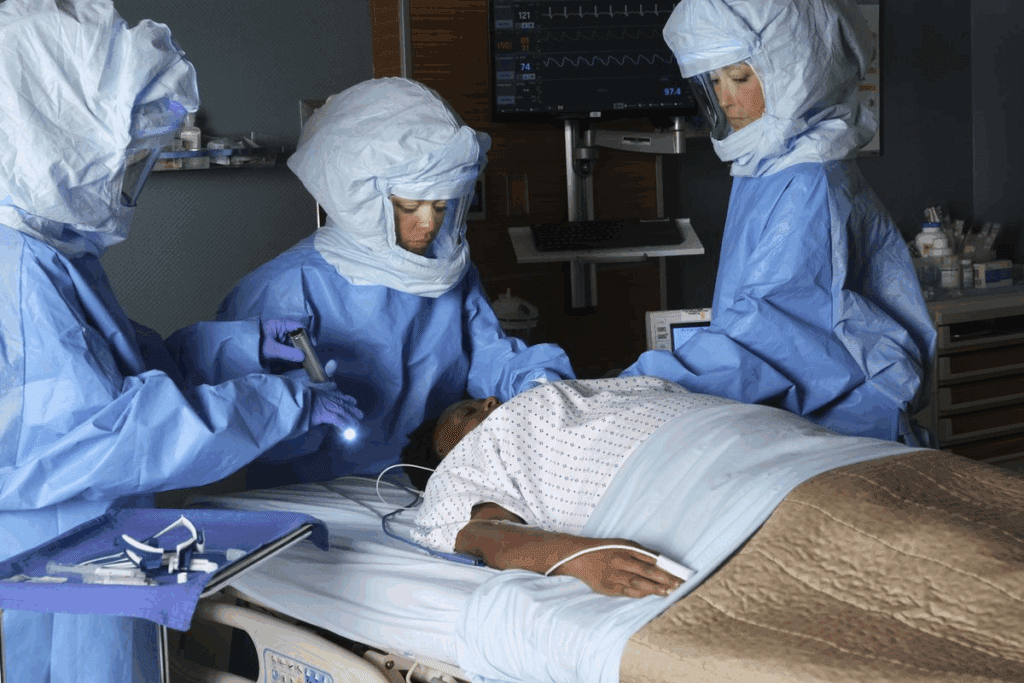
The Neurosurgical Evaluation Process
A well-lit clinical setting, with a neurosurgeon thoughtfully examining a patient’s medical scans on a high-resolution display. The doctor’s focused expression conveys deep medical expertise as they meticulously analyze the intricate structures of the brain. In the foreground, diagnostic instruments and tools are neatly arranged, reflecting the precision and care of the evaluation process. The middle ground features a comfortable examination table, evoking the intimate patient-doctor interaction. The background offers a sense of sterile professionalism, with clean white walls and subtle medical equipment. Soft, diffused lighting illuminates the scene, creating a contemplative atmosphere befitting the gravity of the neurosurgical evaluation.
A detailed neurosurgical evaluation is key for a successful craniotomy. It includes a deep look at the patient’s medical history, diagnostic imaging, and neurological tests. These steps help assess risks and plan the surgery.
Initial Consultation and Medical History Review
The process starts with an initial consultation. Here, the neurosurgeon reviews the patient’s medical history. This is important to understand the patient’s health, past medical issues, and any medications that might impact the surgery.
During this meeting, we also check the patient’s symptoms and how severe their condition is. This helps decide if a craniotomy surgery is needed.
Diagnostic Imaging and Neurological Tests
Diagnostic imaging is crucial in this process. MRI, CT scans, and angiography help see the brain’s structure and find any problems that need surgery.
Neurological tests check the patient’s brain function, motor skills, and senses. These tests give us important information about the brain. They help us plan the surgery.
Risk Assessment and Surgical Planning
After the imaging and tests, we do a detailed risk assessment. We look at the possible risks of the surgery, like infection, bleeding, or bad reactions to anesthesia.
Based on this, we create a surgical plan just for the patient. This plan outlines the surgery steps, expected results, and post-operative care for the best recovery.
Evaluation Component | Description | Importance |
Initial Consultation | Review of medical history and current symptoms | High |
Diagnostic Imaging | MRI, CT scans, angiography to visualize brain structure | High |
Neurological Tests | Assessment of cognitive function, motor skills, and sensory responses | High |
Risk Assessment | Evaluation of potential surgical risks | High |
Surgical Planning | Personalized plan outlining surgical steps and expected outcomes | High |
The Decision-Making Process Between Patient and Neurosurgeon
A well-lit examination room with a neurosurgeon and patient sitting across from each other, engaged in a serious discussion. The neurosurgeon gestures towards a detailed anatomical diagram of the human skull on the wall, explaining the craniotomy procedure. The patient listens intently, brow furrowed, as they weigh the risks and benefits of the surgery. The room exudes a somber, yet thoughtful atmosphere, capturing the gravity of the decision-making process between doctor and patient.
Choosing to have a craniotomy involves looking at if surgery is really needed, other options, and risks. This big decision is made together by the patient and neurosurgeon. They make sure to think about everything carefully.
Understanding Surgical Necessity vs. Alternatives
It’s key to know if surgery is really needed or if there are other ways to treat the problem. We check how serious the condition is and if surgery is the best choice. This helps make a choice that’s best for the patient.
Other options might be medicine, radiation, or less invasive surgeries. The right choice depends on the patient’s health and their condition’s details.
Weighing Benefits Against Risks
Every surgery has good points and possible downsides. For a craniotomy, we look at the chance to help symptoms or fix the problem against the surgery’s risks. We think about complications, how it might affect life quality, and the chance of success.
- Potential benefits include feeling better or fixing the problem.
- Risks could be surgery problems, infection, or bad reactions to anesthesia.
Informed Consent and Patient Autonomy
It’s very important that patients know everything about their condition, the treatment, and what might happen. Informed consent is a patient’s right, and we must give clear info so they can decide on their care.
We respect patient autonomy by letting them be part of the decision-making. We want to give patients the knowledge to make choices that are best for them.
Preparing for Craniotomy Surgery
Sterile surgical setting, bright overhead lighting illuminating a medical team preparing for craniotomy surgery. Close-up view of a surgeon’s gloved hands carefully arranging instruments – scalpels, retractors, bone saws – on a stainless steel tray. In the background, a patient’s shaved head with surgical markings visible, awaiting the delicate procedure. An atmosphere of focused professionalism and meticulous attention to detail pervades the scene, reflecting the critical importance of this complex neurosurgical operation.
Getting ready for a craniotomy surgery is a detailed process. It includes medical checks, lifestyle changes, and mental prep. Understanding these steps is key to a good outcome.
Medical Preparations and Pre-Surgical Testing
Before surgery, patients get a full health check. This includes blood tests, heart checks, and scans like MRI or CT. We also look at your medical history to adjust your meds and manage health issues.
Pre-surgical testing is vital to find any hidden problems. These tests help us make the surgery safer and more effective for you.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before surgery can help your recovery. This means stopping smoking, avoiding blood-thinning meds, and eating well. A healthy body is better prepared for surgery.
We suggest getting your home ready for recovery. Have the right supplies and support people ready to help. This includes help with daily tasks and personal care.
Mental and Emotional Preparation
Preparing mentally and emotionally is as important as physical prep. Talk to your healthcare team about your fears and worries. Knowing what to expect can reduce anxiety and prepare you for what’s ahead.
Try stress-reducing activities like meditation or gentle exercise. We’re here to support you, making sure you’re informed and cared for.
The Craniotomy Procedure Step by Step
A high-quality, detailed surgical illustration of a craniotomy procedure, as if captured by a professional medical photographer. The scene depicts the surgical field with a carefully exposed skull, the cranium being gently removed, exposing the dura mater and delicate brain tissue underneath. The lighting is bright and directional, casting dramatic shadows and highlights to accentuate the anatomical structures. The composition places the viewer at an angle slightly above the operating table, providing a clear, unobstructed view of the procedure. The mood is one of clinical precision and focus, conveying the gravity and importance of the neurosurgical intervention. No extraneous elements are present, allowing the viewer to concentrate solely on the step-by-step craniotomy process.
A craniotomy is a surgery where part of the skull is removed to reach the brain. It’s a complex operation that needs a skilled team of neurosurgeons.
Anesthesia and Positioning
The first step is to give the patient anesthesia. This keeps them pain-free and comfortable. The type of anesthesia depends on the patient’s health and the brain area being worked on.
After anesthesia, the patient is placed on the operating table. This position is key for the surgery’s success.
Craniotomy Incision and Bone Flap Creation
The team then makes a precise craniotomy incision. The incision’s size and location depend on the brain area being accessed. Next, a bone flap is made by removing a part of the skull.
- The bone flap is made with special tools.
- The size and location of the bone flap depend on the surgery’s needs.
Intracranial Surgical Intervention
With the bone flap off, the neurosurgeon starts the intracranial surgery. This is where the actual treatment happens. It could be removing a tumor, clipping an aneurysm, or fixing a vascular malformation.
“The intracranial part of the surgery is where the neurosurgeon’s skill and precision are most critical, as they navigate the delicate structures of the brain.” – Neurosurgical Expert
Bone Flap Replacement and Incision Closure
After the brain surgery, the bone flap is put back, and the incision is closed. The bone flap is secured with plates, screws, or sutures to help it heal.
- The bone flap is carefully put back in place.
- The incision is closed in layers to minimize scarring and promote healing.
Throughout the surgery, the team watches the patient closely. They monitor vital signs and adjust their methods as needed for the best results.
Craniotomy Recovery Timeline and Process
The journey to recovery after a craniotomy has many phases. These include immediate care after surgery and long-term rehabilitation. Knowing these phases helps patients recover well.
Immediate Post-Operative Care in ICU
After surgery, patients go to the ICU for close watch. The ICU team checks vital signs and manages pain. This is key for catching any immediate problems.
The ICU phase is where patients are closely monitored to catch any potential issues early.
“The care received in the ICU sets the foundation for a successful recovery.”
Hospital Stay Duration and Monitoring
The time in the hospital varies based on the surgery’s complexity and the patient’s condition. Patients usually stay a few days to a week. The medical team keeps an eye on their brain function, manages pain, and looks for complications.
Day | Monitoring Activities | Care Objectives |
1-2 | Vital sign monitoring, neurological checks | Stabilize patient, manage pain |
3-5 | Continued monitoring, wound care | Prevent infection, promote healing |
6-7 | Rehabilitation assessment, discharge planning | Prepare for home recovery, rehabilitation |
Short-Term Recovery at Home
After leaving the hospital, patients recover at home. It’s crucial to follow the doctor’s instructions, including wound care and medication. Patients might feel tired, have headaches, and other symptoms that get better over time.
- Rest and avoid strenuous activities
- Follow medication regimen as prescribed
- Attend follow-up appointments
Long-Term Rehabilitation and Follow-up Care
Recovery often goes beyond the hospital and short-term at home. Long-term rehab may be needed to get back strength, brain function, and independence. This includes physical, occupational, and speech therapy, based on the patient’s needs.
We know recovery can be tough, but with the right care, patients can see big improvements. Our team is dedicated to giving full care throughout the recovery journey.
Potential Risks and Long-Term Side Effects of Craniotomy
Craniotomy can save lives, but it comes with risks and long-term effects. We aim to inform you about possible complications. This way, you can make a well-informed decision.
Short-Term Complications
Short-term issues after a craniotomy can be serious. These include:
- Infection: As with any surgery, there’s a chance of infection. This can be treated with antibiotics but might need more care.
- Bleeding: Bleeding during or after surgery is a risk. Sometimes, it may need a blood transfusion or more surgery.
- Neurological Deficits: Depending on the brain area, patients might face temporary or permanent brain function issues.
Long-Term Side Effects of Craniotomy
Long-term effects can differ for each patient. Some possible long-term side effects are:
- Seizures: There’s a chance of seizures after surgery. These might need ongoing treatment with seizure medications.
- Cognitive Changes: Some patients might see changes in thinking, like memory problems or trouble focusing.
- Emotional and Behavioral Changes: The surgery can lead to emotional or behavioral changes. These might need support and management.
Risk Factors That Increase Complication Rates
Some factors can raise the risk of complications after a craniotomy. These include:
- Age: Older patients might face higher risks due to health conditions.
- Pre-existing Medical Conditions: Conditions like diabetes, heart disease, or lung disease can up the surgical risks.
- Previous Brain Surgery: Patients who’ve had brain surgery before might face extra risks because of scar tissue or other changes.
Knowing these risks and factors is key to making an informed choice about a craniotomy. We work closely with our patients. We assess their risk profile and create a plan to reduce complications.
Expected Outcomes and Success Rates
The results of craniotomy surgery can change a lot based on the condition being treated. Patients and their families want to know what to expect. They are interested in the surgery’s benefits and risks.
Condition-Specific Outcomes and Prognosis
The success of craniotomy depends on the condition being treated. For example, patients with brain tumors may have different results than those with traumatic brain injuries or cerebrovascular conditions.
- Brain Tumors: Results depend on the tumor’s type, size, and location. Some see big improvements, while others need ongoing treatment.
- Traumatic Brain Injuries: Results vary with injury severity and patient health. Quick surgery can greatly improve survival and function.
- Cerebrovascular Conditions: Surgery for aneurysms or AVMs can be very effective. It lowers the risk of future brain problems.
Quality of Life After Craniotomy Surgery
Quality of life after craniotomy is very important. The surgery is a big event, but recovery and life quality depend on many things. These include the condition, the patient’s age, and health.
Many patients see better symptoms and life quality after surgery. But, how much they recover can differ. Some go back to normal, while others need more help and support.
- Good care right after surgery is key for recovery.
- Rehab helps patients get back lost functions.
- Long-term medical care is needed to manage any lasting effects.
We stress the need for a detailed care plan. This includes getting ready for surgery, skilled surgery, and good care after. Our goal is to improve our patients’ lives and outcomes.
Special Considerations for Different Patient Groups
Different patient groups face unique challenges during craniotomy procedures. We must consider these factors to ensure the best outcomes for our patients.
Pediatric Patients and Cranial Surgery
Pediatric patients need special care for craniotomy due to their developing brains. Surgeons must consider the child’s age, size, and developmental stage when planning. The skull’s anatomy and the brain’s developmental stage are key in determining the surgical approach.
Pediatric neurosurgery is a specialized field. Our team is trained to handle these complexities. We ensure young patients get the best care.
Elderly Patients and Surgical Risk Assessment
Elderly patients often have comorbidities that can complicate surgery. We carefully assess their overall health to determine risks and benefits. This helps plan a safe and effective surgical strategy.
Comorbidities like heart disease, diabetes, or hypertension can affect outcomes. Our team works closely with other specialists to manage these conditions and minimize risks during surgery.
Patients with Comorbidities and Complex Cases
Patients with complex medical conditions or comorbidities need a tailored approach to surgery. Our team collaborates with specialists to develop a comprehensive treatment plan. This plan addresses the patient’s overall health.
Complex cases may involve brain tumors, vascular malformations, or traumatic brain injuries. Each case is unique and requires a customized surgical plan that considers the patient’s specific needs and health status.
Alternative Treatments to Craniotomy
In some cases, doctors might look at other treatments instead of craniotomy. These options can include minimally invasive neurosurgical procedures or non-surgical ways to manage conditions.
Minimally Invasive Neurosurgical Options
Minimally invasive neurosurgery is a growing alternative to traditional craniotomy. It uses smaller cuts and less brain disruption. This can lead to faster recovery times.
- Endoscopic Surgery: This uses a thin, flexible tube with a camera and light for small incisions.
- Stereotactic Surgery: A 3D system helps find small targets in the brain for precise surgery.
- Keyhole Surgery: Small craniotomies are used for aneurysm clipping or tumor removal.
These options are great for patients at high risk for complications from traditional craniotomy. They’re also good for conditions that can be treated this way.
Non-Surgical Alternatives for Brain Conditions
For some brain conditions, non-surgical treatments are good alternatives to craniotomy. These include:
- Medication Management: Medications can manage symptoms of certain brain tumors or epilepsy, reducing the need for surgery.
- Radiation Therapy: Gamma Knife radiosurgery or fractionated radiation therapy can treat brain tumors or vascular malformations without surgery.
- Observation and Monitoring: If the condition isn’t urgent, watching it closely with regular checks and scans might be the best approach.
It’s important for patients to talk to their doctor. They can help find the best treatment plan for their specific condition and needs.
Conclusion
Figuring out if someone needs a craniotomy involves a detailed check-up by a neurosurgeon. This includes looking at their health, any medical conditions, and the risks of brain surgery.
In this article, we’ve covered what a craniotomy is, its types, and when it might be needed. We’ve also talked about how important it is to carefully decide if someone should have this surgery.
Getting a full neurosurgical check-up is key to seeing if a craniotomy is right for someone. This helps patients and their families understand the surgery better. It helps them make choices about their health care.
Craniotomy can greatly improve or save lives for many people. We hope to help those dealing with brain surgery by providing detailed information on craniotomy and who might need it.
FAQ
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is temporarily removed. This lets neurosurgeons treat brain issues.
What conditions may require a craniotomy?
You might need a craniotomy for brain tumors, head injuries, blood vessel problems, or certain neurological disorders.
How is a patient’s eligibility for craniotomy determined?
Doctors check your health, age, and if you can handle surgery. This helps decide if you’re a good candidate.
What is the difference between craniotomy and craniectomy?
A craniotomy removes part of the skull temporarily. It’s put back later. A craniectomy removes part of the skull but doesn’t put it back right away. This is often to reduce swelling.
What are the potential risks and long-term side effects of craniotomy?
Risks include infections and bleeding right after surgery. Long-term, you might face neurological problems. This depends on your condition and health.
How long does it take to recover from a craniotomy?
Recovery time varies. You’ll first stay in the ICU, then in the hospital. After that, you’ll recover at home and possibly need rehab. It can take weeks to months.
Are there alternative treatments to craniotomy?
Yes, there are. Options include less invasive surgeries and non-surgical treatments. These depend on your condition and health.
How do I prepare for craniotomy surgery?
Get ready by following medical instructions and adjusting your lifestyle. Also, mentally prepare for the best results.
What is the success rate of craniotomy surgery?
Success rates vary. They depend on your condition, the surgery, and your health.
Can anyone undergo craniotomy surgery?
Not everyone can have the surgery. Your age, health, and certain conditions might make you ineligible.
What is the role of informed consent in craniotomy?
Informed consent is key. It makes sure you know the surgery’s need, risks, benefits, and options. This lets you make your own choice.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560922/