Last Updated on December 1, 2025 by Bilal Hasdemir
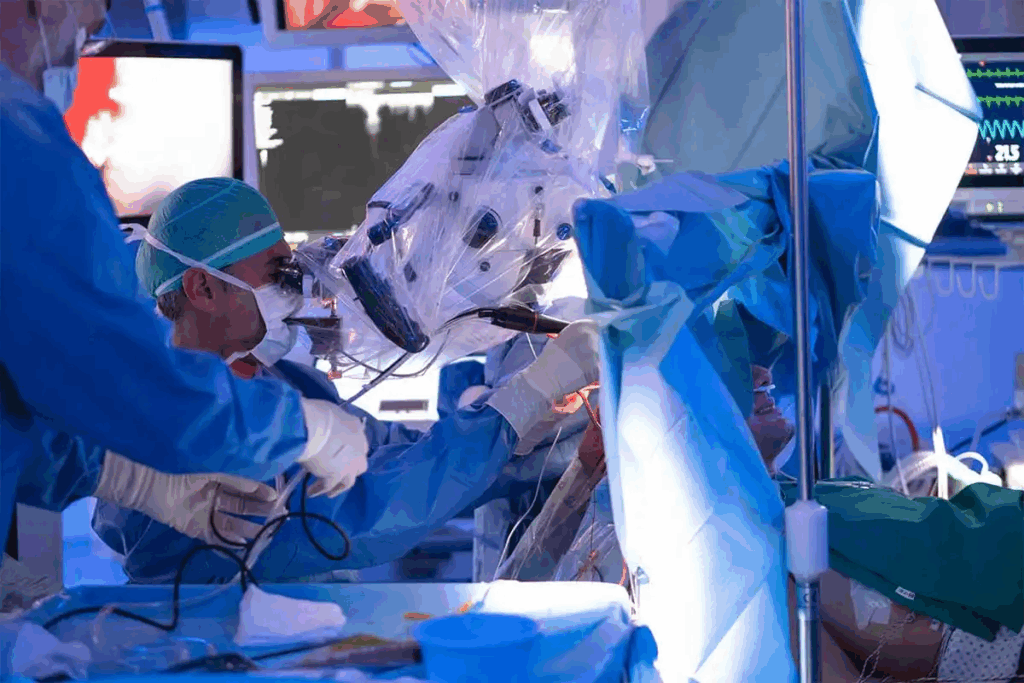
Brain surgery is a complex and delicate procedure. It requires precision and care. A craniotomy, where a part of the skull is temporarily removed, is a common technique.
After the surgery, the bone flap is put back in place. The skull is then closed. This is key for the patient’s recovery. It helps restore the skull’s natural protection and promotes healing.
Key Takeaways
- The skull is closed after brain surgery by replacing the bone flap that was removed during the craniotomy procedure.
- The bone flap is typically secured with plates, screws, or other medical devices.
- Skull closure is a critical step in the brain surgery process, as it helps to restore the skull’s natural protection.
- A successful skull closure can promote healing and reduce the risk of complications.
- The skull closure technique used may vary depending on the individual case and the surgeon’s preference.
The Purpose of Opening the Skull During Brain Surgery
Craniotomy is a surgery where a part of the skull is taken out. It lets surgeons get to the brain. This is key for brain tumor removal and other complex surgeries.
Accessing the Brain for Medical Intervention
The main goal of a craniotomy is to give surgeons a direct way to the brain. They can then do detailed work. This might be taking out a brain tumor, fixing blood vessel problems, or dealing with other brain issues.
Why Proper Closure is Critical
After a craniotomy, closing up right is very important. It helps avoid problems and makes sure the surgery works. This means putting the bone flap back and closing the dura mater, a layer that protects the brain.
Good closure helps prevent infections, helps the healing process, and lowers the chance of problems after surgery. Doctors say, “The success of a craniotomy depends on the surgery itself and how well the skull is closed after.”
Understanding Craniotomy: The Most Common Skull Opening Procedure
Neurosurgeons often use a craniotomy to reach the brain for surgery. This involves taking out and then putting back a bone flap. It’s key for treating many brain issues that need direct surgery.
Definition and Surgical Objectives
A craniotomy is a surgery where a bone flap is removed from the skull to get to the brain. The main goals of this surgery change based on the problem being treated. It might be to ease brain pressure, take out tumors, or fix blood vessel problems.
The goals of surgery depend on the patient’s specific issue. Doctors plan carefully before surgery, using images and maps to find the right spot.
Craniotomy vs. Craniectomy: Key Differences
Craniotomy and craniectomy both remove part of the skull. But, the main difference is in putting the bone flap back. In a craniotomy, the bone flap goes back right after surgery. In a craniectomy, the bone is not put back right away and might stay out or be put back later.
Procedure | Bone Flap Replacement | Typical Use Cases |
Craniotomy | Replaced immediately after surgery | Tumor removal, vascular repair |
Craniectomy | Not replaced immediately; may be replaced later | Decompressive surgery, severe trauma |
Craniotomies can be different types, like pterional or frontotemporal craniotomies. These names come from where the surgery is done and the approach used.
Preoperative Planning for Skull Closure
Getting the skull closed after brain surgery needs careful planning before the surgery. This step is key to making sure the surgical team is ready. They need to think about possible problems and plan the surgery just right for each patient.
Imaging and Surgical Mapping
Scans like MRI and CT are very important in planning. They show the patient’s skull and where the surgery will be. Surgical mapping uses this info to make a detailed plan. This includes where to make the cut in the skull and how to close it.
Patient-Specific Considerations
Every patient is different, so their plan needs to be too. Things like their health, past surgeries, and the type of lesion matter. This makes the surgery safer and more likely to succeed.
Consideration | Description | Impact on Surgery |
Imaging Techniques | Use of MRI and CT scans for detailed cranial anatomy | Enhances precision in surgical planning |
Surgical Mapping | Creating a detailed plan based on imaging data | Optimizes craniotomy site and closure strategy |
Patient Health | Assessment of overall health and previous surgeries | Minimizes risks and improves outcomes |
Materials Used in Modern Skull Closure
Modern skull closure uses many materials for safe and effective surgery. The right material is key for good results. It affects both the surgery’s success and the patient’s long-term health.
Titanium Fixation Systems
Titanium systems are popular for skull closure. They are strong, safe, and fit well with the body. These systems help bones heal properly.
Titanium is a top choice for cranial surgeries. It securely holds bone flaps in place.
Biodegradable Implants
Biodegradable implants are a new way to close the skull. They dissolve as the bone heals. This means no second surgery to remove them.
Materials like polylactic acid and polyglycolic acid are used. They offer a good alternative to metal implants.
Bone Cement and Other Adjuncts
Bone cement and other materials help close the skull tightly. They fill gaps and support the skull. The choice depends on the surgery site and the surgeon.
With many materials to choose from, surgeons can customize care for each patient. This improves results in cranial surgery.
The Step-by-Step Process of Closing the Skull
Skull closure is key for a patient’s recovery. It starts with preparing the bone flap. Then, the skull piece is repositioned and secured with fixation devices.
Preparation of the Bone Flap
The bone flap is carefully kept from the craniotomy. Cleaning and inspecting the flap for damage is vital before attaching it back. It’s stored in a sterile place to avoid infection.
“The preservation of the bone flap is a critical step in the skull closure process,” experts say. Proper handling reduces the risk of problems.
Repositioning the Skull Piece
After preparing the bone flap, it’s put back in its place. This step needs precision for the right fit. Surgeons use anatomical landmarks to guide the reattachment.
Securing the Bone with Fixation Devices
The last step is securing the bone flap with devices like titanium plates or biodegradable implants. These devices help the bone heal. The choice of device depends on the patient’s health and the surgeon’s choice.
Advanced fixation devices have made skull closure better. A study found, “New materials and techniques have made skull closure more durable and effective.”
Dural Closure Techniques Following Brain Surgery
Effective dural closure is key to avoiding complications and aiding healing after craniotomy surgery. The dura mater, a protective layer around the brain and spinal cord, must be closed well. This prevents infection and ensures a smooth recovery.
Primary Suturing of the Dura Mater
Primary suturing is a traditional method for dural closure. The surgeon directly sews the dural edges together. This method is best for small dural defects where the edges can be sewn without tension. Primary suturing keeps the natural anatomy and aids healing by closing the dural edges.
The goal of dural closure is to restore the dura mater’s integrity.This protects the brain and lowers the risk of complications after surgery.
Synthetic Dural Substitutes and Autologous Grafts
For large dural defects, surgeons use synthetic dural substitutes or autologous grafts. Synthetic substitutes are made from biocompatible materials that blend with the surrounding tissue. Autologous grafts come from the patient’s own body, usually from the pericranium or fascia lata. They offer a natural and biocompatible solution.
The choice between synthetic substitutes and autologous grafts depends on several factors. These include the dural defect’s size, patient-specific needs, and the surgeon’s preference. Both methods aim for a watertight closure. This minimizes the risk of cerebrospinal fluid leaks and other complications.
Soft Tissue Closure After Cranial Procedures
After cranial procedures, closing soft tissues is key for healing and skull strength. This involves several layers, each needing careful attention.
Muscle and Fascia Reapproximation
The first step is to reattach the muscle and fascia. This is done by suturing, where the surgeon puts the muscle and fascia back in place. Proper reapproximation is vital for the area’s normal function and anatomy.
Subcutaneous Tissue Closure
After reattaching the muscle and fascia, the subcutaneous tissue is closed. This layer uses absorbable sutures to reduce complications and aid healing. The aim is to approximate the tissue well, cutting down on recovery time.
Skin Closure Methods and Materials
The last layer to close is the skin. Skin closure can be done with sutures, staples, or adhesives. The choice depends on the patient and the surgeon. Skin closure is important for a good look and to prevent wound issues.
In summary, soft tissue closure after cranial procedures is complex. Knowing the different techniques and materials helps surgeons improve patient results and lower complication risks.
Special Techniques for Different Types of Craniotomies
Each type of craniotomy needs its own closure method for the best results. The different ways to do a craniotomy mean we use various strategies. These are based on the surgery type and the patient’s body.
Pterional and Frontotemporal Approaches
Pterional craniotomy is used for some brain tumors and aneurysms. It’s important to close it well to fix the temporal muscle and fascia. Frontotemporal craniotomy is similar, focusing on attaching the temporalis muscle back to its original spot. This helps with both looks and function.
Posterior Fossa and Suboccipital Closures
Posterior fossa craniotomy is for tumors or lesions in the cerebellum or brainstem. Closing it right is key to avoid CSF leaks. Suboccipital craniotomy closure means fixing the suboccipital muscles and fascia. Then, we close the soft tissues in layers.
Bifrontal and Extended Craniotomies
Bifrontal craniotomy is for frontal lobe or anterior cranial fossa lesions. It needs a detailed closure. This includes putting the bone flap back, securing it with titanium plates or meshes, and closing the frontal sinus if needed.
Craniotomy Type | Closure Technique | Key Considerations |
Pterional | Reattachment of temporalis muscle | Cosmetic and functional recovery |
Posterior Fossa | Layered closure to prevent CSF leakage | Preventing postoperative complications |
Bifrontal | Securing bone flap with titanium | Ensuring stability and promoting healing |
Temporary Skull Closure in Staged Procedures
Temporary skull closure is a key method in neurosurgery for managing severe brain swelling. It’s part of staged procedures. The final closure is delayed until the patient’s health improves.
Indications for Delayed Definitive Closure
Delayed closure is needed when there’s a lot of brain swelling or the patient’s health is unstable. The main aim is to avoid more brain damage. It also gives time for the swelling to go down.
The choice to delay the final closure is made during the first surgery. It depends on the brain swelling, pressure inside the skull, and the patient’s overall health.
Synthetic Materials for Interim Protection
For temporary skull closure, synthetic materials are used to protect the brain. These can be silicone or acrylic implants. They cover the skull defect until the final closure can happen.
Material | Description | Advantages |
Silicone | Flexible, inert material | Easy to shape, minimal tissue reaction |
Acrylic | Rigid, durable material | Provides strong protection, can be molded to fit |
Using these materials helps in managing complex cases. They offer a protective barrier for the brain until the final closure.
Cranioplasty: Reconstructing the Skull After Craniectomy
Cranioplasty is a surgery that fixes the skull after a craniectomy. It’s key to protect the brain and make the skull look normal again.
When to do cranioplasty depends on the patient’s health and why they had the craniectomy.
Timing of Reconstructive Procedures
Doctors decide on cranioplasty timing for each patient. They wait until the patient is stable and there’s no infection or swelling.
Autologous Bone vs. Synthetic Implants
Doctors often choose between using the patient’s bone or synthetic materials. Using the patient’s bone is safer but not always possible. Synthetic implants are a good backup.
Custom-Made Cranial Implants
New technology lets doctors make custom cranial implants. These are made from 3D scans to fit the patient’s skull perfectly, giving the best look and fit.
Implant Type | Advantages | Disadvantages |
Autologous Bone | Reduced risk of rejection, natural integration | Limited availability, possible resorption |
Synthetic Implants | Reliable, customizable | Risk of infection, foreign body reaction |
Custom-Made Implants | Precise fit, optimal cosmetic outcome | Higher cost, requires advanced technology |
Potential Complications of Skull Closure
Skull closure after brain surgery is vital but can face complications. Neurosurgeons work hard to avoid these issues. Yet, several problems can affect recovery and outcomes.
Infection and Bone Flap Resorption
Infection is a big risk after skull closure. It can cause serious problems if not treated quickly. Bone flap resorption happens when the bone flap is absorbed by the body. Sometimes, this requires more surgery.
Hardware Failure and Exposure
Hardware like plates and screws can fail or show. This can lead to infections and the need for more surgery. It’s a serious issue that needs quick action.
Cosmetic and Functional Issues
Skull closure can also affect how a person looks. If it’s not done with looks in mind, it can be a problem. It can also affect how things work, like if it messes with the alignment of other parts.
Complication | Description | Potential Consequences |
Infection | Bacterial or other infection at the surgical site | Delayed healing, additional surgery, prolonged antibiotic treatment |
Bone Flap Resorption | Gradual absorption of the reattached bone flap | Cosmetic deformity, need for cranioplasty |
Hardware Failure | Failure of fixation devices like plates and screws | Infection, need for revision surgery, hardware removal |
Post-Operative Care and Monitoring
The time after a craniotomy is critical for a good outcome. Good post-operative care means managing right after surgery and checking up later. This care is key for recovery.
Immediate Post-Surgical Management
Right after brain surgery, patients stay in the ICU. Here, they watch for any problems. They check vital signs, brain health, and infections. They also manage pain, stop seizures, and keep blood pressure right.
Long-Term Follow-Up Protocols
After leaving the hospital, patients need long-term follow-up. They see the neurosurgeon often, get scans, and might need rehab. This helps catch any issues early and makes sure they’re healing right.
Follow-Up Care | Frequency | Purpose |
Post-operative check-ups | Weekly for the first month | Monitor wound healing and neurological status |
Imaging studies | As needed, typically within 3-6 months | Assess the surgical site and detect any complications |
Rehabilitation | Ongoing, based on individual needs | Improve functional outcomes and quality of life |
The Healing Process: How the Skull Recovers
After a craniotomy, the skull starts a healing process. This is key to getting back to normal. It involves many steps that work together for recovery.
The healing after craniotomy surgery is complex. Bone integration is a big part of it. It’s when the bone flap reattaches to the skull.
Timeline for Bone Integration
Bone integration takes months. It starts with inflammation, then moves to repair. The body rebuilds the bone during this time.
- Immediate Post-Surgery: Inflammation phase
- First Few Weeks: Gradual reduction in inflammation
- Several Months: Bone repair and integration
Factors Affecting Healing Outcomes
Many things can change how well you heal after a craniotomy. Your age, health, and the surgery method are important.
Factor | Influence on Healing |
Age | Older patients may heal slower |
Overall Health | Chronic conditions can slow recovery |
Surgical Technique | Less invasive methods can speed up recovery |
Knowing about these factors and the bone integration timeline helps. It can make recovery better for those having craniotomy surgery.
Technological Advancements in Cranial Closure
The field of cranial surgery has seen big changes in recent years. These changes have made surgeries better, cut down recovery times, and improved life quality for those who have craniotomy procedures.
3D-Printed Custom Implants
One big step forward is the use of 3D-printed custom implants. These implants fit perfectly with the patient’s body, lowering the chance of problems. Thanks to 3D printing, complex shapes can be made to meet each patient’s needs.
Computer-Assisted Surgical Planning
Computer-assisted planning has changed how surgeries are planned and done. It lets surgeons make detailed 3D models of the skull. This makes planning and simulating surgeries more accurate. It also cuts down on mistakes and improves results for patients.
Technological Advancement | Benefits |
3D-Printed Custom Implants | Precise fit, reduced risk of complications, customized to patient anatomy |
Computer-Assisted Surgical Planning | Improved accuracy, reduced risk of errors, enhanced patient outcomes |
These new technologies have greatly improved cranial surgery. They offer better results for patients having craniotomy procedures. As technology keeps getting better, we can expect even more advancements in cranial closure.
Patient Experience and Recovery Expectations
Patients getting a craniotomy often wonder about recovery. The journey can differ a lot. This depends on the surgery’s complexity, the patient’s health, and their strength.
Physical Sensations During Healing
Patients may feel many things while healing. As one patient shared,
“The first few weeks were challenging, with significant swelling and discomfort, but the pain was manageable with medication.”
They might feel swelling, numbness, and some pain near the surgery site. These feelings usually go away in a few weeks as the body heals.
Timeline for Return to Normal Activities
When to get back to normal activities varies. It depends on the patient’s health and the surgery details. Usually, patients can start with light activities in 4 to 6 weeks.
But, getting back to harder activities can take several months. It’s key to follow the doctor’s advice for a safe recovery.
Conclusion
Understanding skull closure after brain surgery is key for patients. It involves careful planning, precise surgery, and postoperative care.
Craniotomy surgery needs a deep understanding of the brain’s anatomy. Surgeons use different techniques, like titanium systems and biodegradable implants, for the best results.
Recovery times vary based on the patient, the surgery’s complexity, and postoperative care. Patients will slowly get back to normal, with close monitoring and follow-ups to handle any issues.
New medical technologies, like 3D-printed implants and computer-assisted planning, are making craniotomy outcomes better. Knowing about skull closure helps patients understand their recovery better.
FAQ
What is a craniotomy?
A craniotomy is a surgery where a part of the skull is taken off. This lets doctors reach the brain for treatment.
Why is proper skull closure critical after a craniotomy?
Closing the skull right is key to avoid problems. It helps the healing process and keeps the skull protecting the brain.
What is the difference between a craniotomy and a craniectomy?
A craniotomy removes a skull part temporarily and then puts it back. A craniectomy removes a part without putting it back right away.
What materials are used for skull closure?
To close the skull, doctors use titanium systems, implants that dissolve, bone cement, and more.
How is the skull closed after a craniotomy?
Closing the skull means putting the bone flap back in place. It’s held with devices, and then the soft tissues are closed.
What are the possible complications of skull closure?
Complications can be infections, bone parts disappearing, or hardware not working. There can also be cosmetic or functional issues.
How long does it take for the skull to heal after a craniotomy?
Healing times vary. But, bone usually integrates in several months.
What is cranioplasty?
Cranioplasty is a surgery to fix skull defects or deformities. It uses the patient’s own bone or synthetic implants.
When is cranioplasty typically performed?
Cranioplasty happens after swelling goes down and the patient is stable.
What are the benefits of 3D-printed custom implants in cranial closure?
3D-printed implants fit perfectly, cut down surgery time, and look better.
What can patients expect during the recovery period after a craniotomy?
Recovery times differ. Some feel physical sensations, and it takes time to get back to normal.
How does preoperative planning impact skull closure?
Planning before surgery helps. It uses images and maps to prepare for the closure, considering the patient’s needs.
What are the different techniques used for dural closure?
To close the dura, doctors use sutures, synthetic materials, or the patient’s own tissue.
What are the different techniques used for soft tissue closure?
Soft tissue closure involves reattaching muscles and skin. There are many methods and materials used.
References
Craniotomy: The amazing facts on closing the skull https://www.ncbi.nlm.nih.gov/books/NBK560922/